Henry A. Milczuk, MD
- Associate Professor
- Chief, Pediatric Otolaryngology
- Department of Otolaryngology?ead and Neck Surgery
- Oregon Health and Science University
- Portland, Oregon
The major risk factor for infection with Unfortunately diabetes insipidus growth hormone deficiency purchase prandin with american express, the emergence of resistance during therapy with other serious gram-negative pathogens joslin diabetes diet generic 0.5mg prandin amex, such as Klebsiella pneu clindamycin has been reported (especially in erythromycin moniae or Acinetobacter species diabetes prevention program nejm order prandin us, is chronic alcoholism metabolic disease nos prandin 1mg line. These conditions and results of blood cultures are not as reliable diabetes menu order 2 mg prandin, because of the speci c pathogens diabetes prevention legislation buy prandin once a day, with preferred treatment, are listed in tables signi cant risk of contamination [95]. Neither linezolid [241] nor van Treatment options may be simpli ed (table 9) if the etiologic comycin [238] is an optimal drug for methicillin-sensitive S. Choices should be modi ed on the basis of susceptibility test results and advice from local specialists. The neuraminidase the major issue with pathogen-speci c therapy is manage inhibitors are effective against both in uenza A and B viruses, ment of bacteremic S. The implications of whereas the M2 inhibitors, amantadine, and rimantadine are the observational nding that dual therapy was associated with active only against in uenza A [251]. One explanation for the reduced mor resistant to the M2 inhibitors on the basis of antiviral testing tality may be the presence of undiagnosed coinfection with an [252, 253]. The known and did not examine effects of pathogen-speci ctherapy use of in uenza antiviral medications appears to reduce the after the results of blood cultures were available. The bene t likelihood of respiratory tract complications, as re ected by of combination therapy was also most pronounced in the more reduced usage rates of antibacterial agents in ambulatory pa severely ill patients [233, 234]. Parenteral acyclovir is indicated for treatment of varicella zoster virus infection [257] or herpes simplex virus pneumonia. Use of oseltamivir and zanamivir is not recommended patients with viral pneumonias, a high clinical suspicion of for patients with uncomplicated in uenza with symp bacterial superinfection should be maintained. Patients with an illness compatible with in uenza and with known exposure to poultry in areas with previous Studies that demonstrate that treatment of in uenza is ef H5N1 infection should be tested for H5N1 infection. In patients with suspected H5N1 infection, droplet pre the impact of such treatment on patients who are hospitalized cautions and careful routine infection control measures with in uenza pneumonia or a bacterial pneumonia compli should be used until an H5N1 infection is ruled out. The severity of H5N1 infection in humans distin and zanamivir and resistant to the adamantanes (amantidine guishes it from that caused by routine seasonal in uenza. The current recommendation is spiratory failure requiring hospitalization and intensive care has for a 5-day course of treatment at the standard dosage of 75 been seen in the majority of the 1140 recognized cases, and mg 2 times daily. If a pandemic occurs, deaths will used for patients with suspected H5N1 in uenza, and they result from primary in uenza pneumonia with or without sec should be placed in respiratory isolation until that etiology is ondary bacterial pneumonia. Health care personnel should wear N-95 (or higher) consideration, recognizing that treatment recommendations respirators during medical procedures that have a high likeli will likely change as the pandemic progresses. During the current pandemic alert phase (phase 3: cases portant causes of secondary bacterial pneumonia after in u of novel in uenza infection without sustainedperson-to-person enza. Appropriate agents would therefore include cefotaxime, transmission), testing should be focused on con rming all sus ceftriaxone, and respiratory uoroquinolones. Early clinical features of H5N1 or a compatible clinical presentation (shock and necrotizing infection include persistent fever, cough, and respiratory dif pneumonia). Exposure to sick and agnostic tests will be even more important to help target an dying poultry in an area with known or suspected H5N1 activity tibacterial therapy whenever possible, especially for patients has been reported by most patients, although the recognition admitted to the hospital. Time to First Antibiotic Dose Rapid bedside tests to detect in uenza A have been used as screening tools for avian in uenza in some settings. Convalescent-phase serum can be signi cant attention from a quality-of-care perspective. This tested by microneutralization for antibodies to H5 antigen in emphasis is based on 2 retrospective studies of Medicare ben a small number of international reference laboratories. Speci e ciaries that demonstrated statistically signi cantly lowermor mens from suspected cases of H5N1 infection should be sent tality among patients who received early antibiotic therapy[109, to public health laboratories with appropriate biocontainment 264]. The initial study suggested a breakpoint of 8 h [264], facilities; the case should be discussed with health department whereas the subsequent analysis found that 4 h was associated officials to arrange the transfer of specimens and to initiate an with lower mortality [109]. During later phases of an ongoing rst antibiotic dose do not consistently demonstrate this dif pandemic, testing may be necessary for many more patients, ference, although none had as large a patient population. Most so that appropriate treatment and infection control decisions importantly, prospective trials of care by protocol have not can be made, and to assist in de ning the extent of the pan demonstrated a survival bene t to increasing the percentage of demic. A Patients with con rmed or suspected H5N1 in uenza should problem of internal consistency is also present, because, in both be treated with oseltamivir. Arterial oxygen saturation 90% or pO2 60 mm Hg on room air Conversely, a delay in antibiotic therapy has adverse conse a Ability to maintain oral intake quences in many infections. De a Important for discharge or oral switch decision but not necessarily for lay in beginning antibiotic treatment during the transition from determination of nonresponse. The committee felt that the best and most domized to receive either oral therapy alone or intravenous practical resolution to this issue was that the initial dose be given therapy, with the switch occurring after 72 h without fever. Given that there are even more concerns to resolution of symptoms for the patients with nonsevere ill regarding timing of the rst dose of antibiotic when the patient ness was similar with either regimen. Among patients with more is directly admitted to a busy inpatient unit, provision of the severe illness, the rapid switch to oral therapy had the same rst dose in the physicians office may be best if the recom rate of treatment failure and the same time to resolution of mended oral or intramuscular antibiotics are available in the symptoms as prolonged intravenous therapy. Patients should be switched from intravenous to oral bility is achieved has been questioned, even though physicians therapy when they are hemodynamically stable and im commonly choose to observe patients receiving oral therapy proving clinically, are able to ingest medications, and for 1 day. Even in the presence of pneumococcal bacteremia, have a normally functioning gastrointestinal tract. Such patients generally take longer (approximately half ically stable, have no other active medical problems, and a day) to become clinically stable than do nonbacteremic pa have a safe environment for continued care. The bene ts of in-hospital observation after a switch to observation while receiving oral therapy is not necessary. Patients with persistent clinical instability are often read be initiated early for these patients. Short-duration therapy may be suboptimal agent as the intravenous antibiotic or the same drug class for patients with bacteremic S. Switching to a different class of agents simply the risk of associated endocarditis and deep-seated infection), because of its high bioavailability (such as a uoroquinolone) for those with meningitis or endocarditis complicating pneu is probably not necessary for a responding patient. An therapy, a switch to a macrolide alone appears to be safe for 8-day course of therapy for nosocomial P. Stud ies of duration of therapy have focused on patients receiving empirical treatment, and reliable data de ning treatment du 32. A longer duration of therapy may be needed if initial spite adequate uid resuscitation should be considered for therapy was not active against the identi ed pathogen treatment with drotrecogin alfa activated within 24 h of or if it was complicated by extrapulmonary infection, admission. However, the survival advantage therapy in either inpatients or outpatients [276]. The small sample size in that trial, and the bene t of the low-tidal-volume ventilatory and baseline differences between groups compromise the con strategy appeared to be equivalent in the population with pneu clusions. Although the criteria for steroid replacement therapy monia compared with the entire cohort. Patients who do not require immediate intubation but who Although difficult to de ne, nonresponse is not uncommon. Noninfectious Mortality among nonresponding patients is increased sev Complication of pneumonia. Overall mortality rates as high as 49% have been reported Drug fever Deterioration or progression for an entire population of nonresponding hospitalized patients Early (! Empyema/parapneumonic Endocarditis, meningitis, arthritis De nition and classi cation. Lack of a clear-cut and validated Myocardial infarction de nition in the literature makes nonresponse difficult to study. Persistent fever after the rst day of treatment differs signi cantly from fever persisting (or recurring) at day 7 of tory failure or hypotension 172 h after initial treatment is often treatment. Nonresponse can be de ned as absence of or delay sponse are seen in hospitalized patients [101]. The rst is pro in achieving clinical stability, using the criteria in table 10 [274, gressive pneumonia or actual clinical deterioration, with acute 294]. When these criteria were used, the median time to achieve respiratory failure requiring ventilatory support and/or septic clinical stability was 3 days for all patients, but a quarter of shock, usually occurring within the rst 72 h of hospital ad patients took 6 days to meet all of these criteria for stability mission. Deterioration and development of respira achieving this degree of clinical stability occurred in! A separate multicenter trial demonstrated similar ndings further diagnostic testing, and (3) escalation or change in treat [297]. Decisions regarding further di used to refer to the conditions of patients who present with agnostic testing and antibiotic change/escalation are intimately persistence of pulmonary in ltrates 130 days after initial pneu intertwined and need to be discussed in tandem. In a different study, independently associated with a better response in one study mortality among patients with microbiologically guided versus [84], whereas discordant antimicrobial therapy was associated empirical antibiotic changes was not improved (mortality rate, with early failure [81]. However, no antibioticchanges tective factors and their respective odds ratios are summarized. Although in the original study only 8 (16%) of 49 cases are major causes of apparent antibiotic failure. Therefore, the could not be classi ed [101], a subsequent prospective multi rst response to nonresponse or deterioration is to reevaluate center trial found that the cause of failure could not be deter the initial microbiological results. Overall failurea Early failureb Risk factor Decreased risk Increased risk Decreased risk Increased risk Older age (165 years) 0. Other family members or coworkers may have In addition, a positive pneumococcal antigen test result would developed viral symptoms in the interval since the patient was also help with interpretation of subsequent sputum/tracheal admitted, increasing suspicion of this cause. The evaluation of nonresponse is severely hampered if a Nonresponse may also be mimicked by concomitant or sub microbiological diagnosis was not made on initial presentation. Positive including pleural effusions, lung abscess, or central airway blood culture results in the face of what should be adequate obstruction. The pattern of opacities may also suggest al antibiotic therapy should increase the suspicion of either an ternative noninfectious disease, such as bronchiolitis obli tibiotic-resistant isolates or metastatic sites, such as endocarditis terans organizing pneumonia. Empyema and parapneumonic effusions are Despite the high frequency of infectious pulmonary causes important causes of nonresponse [81, 101], and thoracen of nonresponse, the diagnostic utility of respiratory tract cul tesis should be performed whenever signi cant pleural uid tures is less clear. If the warranted because early colonization, rather than superinfec differential of nonresponse includes noninfectious pneu tion with resistant bacteria, is not uncommon in specimens monia mimics, bronchoscopy will provide more diagnostic obtained after initiation of antibiotic treatment. An etiology was determined by bronchoscopy alveolitis pointing toward virus or Chlamydophila infection. Stopping the b-lactam component of combination ther complications, household contacts of high-risk persons, apy to exclude drug fever is probably also safe [156]. Adapted from the Advisory Committee on Immunization Practices, Centers for Disease Control and Prevention [304]. Health care workers in inpatient and outpatient settings saccharide vaccine and inactivated in uenza vaccine are rec and long-term care facilities should receive annual in ommended for all older adults and for younger persons with uenza immunization. The effectiveness of the Coverage levels are lower for younger persons with vaccine vaccine against pneumococcal disease in immunocompromised indications. Ideally, patients should be vac been demonstrated, current guidelines do not suggest repeated cinated before developing pneumonia; therefore, admissionsfor revaccination. The pneumococcal conjugate vaccine is under illnesses other than respiratory tract infections would be an investigation for use in adults but is currently only licensed for appropriate focus. However, its use in children important trigger for assessing the need for immunization. Patients with an acute fever should tors and on how closely the antigens in the vaccine are matched not be vaccinated until their fever has resolved. A systematic review a febrile reaction to immunization with recurrent/superinfec demonstrates that in uenza vaccine effectively prevents pneu tion pneumonia is a risk. A recent large for pneumonia is warranted for patients for whom outpatient observational study of adults 65 years of age found that vac follow-up is unreliable, and such vaccinations have been safely cination against in uenza was associated with a reduction in given to many patients. In long In uenza and pneumococcal vaccines can be given at the same term-care facilities, vaccination of health care workers with time in different arms. Because the main virulence factors of in uenza for prevention and control of in uenza. Vaccination status should be assessed at the time of hos in uenza vaccine takes 2 weeks in adults; chemoprophylaxis pital admission for all patients, especially those with may be useful during this period for those with household medical illnesses. Vaccination may be performed either at hospital dis in uenza complications in the setting of a community outbreak charge or during outpatient treatment. In uenza vaccine should be offered to persons at hospital vaccination for those who may not respond well to in uenza discharge or during outpatient treatment during the fall vaccine. Because it is unknown whether administering in uenza department about a condition of interest is the rst step to antiviral medications affects the performance of the new live getting public health professionals involved. Rules and regu attenuated intranasal vaccine, this vaccine should not be used lations regarding which diseases are reportable differ between in conjunction with antiviral agents. For pneumonia, most states require reporting for le Other types of vaccination can be considered. However, pneumonia is one of gation can determine whether others may be at risk and whether the major complications of pertussis. One-time vaccination with the new tetanus breaks caused by environmental contamination [130].
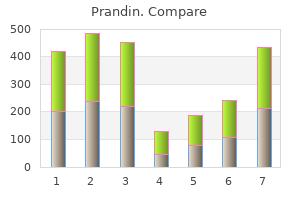
Decision-making process With regard to prospective donors with treated hypertension diabetes diet chart pdf order prandin 1mg, the Guideline Development Group reviewed the evidence from the systematic review and agreed on the following recommendations diabetes type 1 low discount prandin 0.5mg online. Recommendations Accept Individuals with stable uncomplicated hypertension controlled by medication Defer Individuals who have recently started taking anti-hypertensive medication diabetes 7 prandin 2mg online, or whose dose of anti-hypertensive medication has been adjusted: defer for 28 days after the blood pressure has been stabilized Defer permanently Individuals with hypertensive heart or renal disease 151 5 diabetes type 1 emergency effective 2 mg prandin. Population Intervention outcome Prospective blood Acceptance or Minimize adverse effects related to donors deferral for blood blood donation donation Avoid unnecessary deferral of suitable blood donors Minimize risk of adverse reactions in recipients of blood Systematic review of safety of blood donation from individuals with diabetes 1 Stainsby D et al diabetes symptoms hives buy cheap prandin 2 mg line. Decision-making process the Guideline Development Group reviewed the evidence from this systematic review and agreed on the following recommendations diabetes type 2 blood sugar range purchase prandin master card. Decision-making process the Guideline Development Group agreed on the following recommendations based the above reference, on their medical knowledge and experience from best practice. A comparison between Questionnaire answers and the presence of circulating IgE antibodies. Decision-making process the Guideline Development Group agreed on the following recommendations with reference to the above background literature and based on their medical knowledge and experience from best practice. Over a 2-year period from 1987, 613 donors with a history of seizures donated blood a total of 723 times; of these, 186 (35. Total adverse reactions were slightly but not signifcantly higher in donors with seizure disorders (3. The authors concluded that individuals with seizures or epilepsy are not at greater risk of adverse reactions after blood donation and restrictions on their participation as blood donors are not warranted. Critical evaluation of study this multicentric observational study was carried out twenty years ago and has not been repeated since. Clinical practice in donor care has not altered signifcantly in the interim so the fndings remain relevant and are applicable worldwide. The incidence of adverse reactions in the study group was compared to the overall incidence in all blood donors. Matched controls were not identifed and there was no allowance for confounding factors such as age and donor status (whether frst-time or repeat donor) that are known to be signifcant factors in predicting the incidence of adverse reactions. Regulations prohibiting blood donation by individuals with seizures or epilepsy are not necessary. Managing the risk of transmission of variant Creutzfeld-Jakob disease by blood products. Decision-making process the Guideline Development Group reviewed the evidence on prospective donors with epilepsy and concluded that, until further evidence is available, a precautionary approach should continue to be recommended. In the absence of relevant published evidence on other central nervous system disorders, the group agreed on the following recommendations based on their medical knowledge and experience from best practice. Edgren et al report a landmark large retrospective cohort study of cancer incidence among patients who received blood from donors deemed retrospectively to have a subclinical cancer at the time of donation (diagnosed with cancer within fve years of the donation). There was no excess risk of cancer among recipients of blood from pre-cancerous donors compared with recipients of blood from non cancerous donors. Decision-making process Based on the available evidence summarized above, and their medical knowledge and expertise, the Guideline Development Group agreed on the following recommendations. Recommendations regarding the use of medication by prospective blood donors are addressed in Section 6. Recommendations Accept Individuals with anxiety disorders or mood (affective) disorders. Decision-making process the Guideline Development Group agreed on the following recommendations based on the above references, and on their medical knowledge and experience from best practice. Decision-making process the Guideline Development Group therefore recommended endorsement of currently accepted recommendations based on published literature, medical principles and experience from best practice. In the absence of any such evidence, the Guideline Development Group based their recommendations on their medical knowledge and experience from best practice. These recommendations are endorsed, although the work of Park et al suggests that they may be overly precautionary. Recommendations regarding the use of aspirin and related drugs are based on well-documented knowledge of the effects of these drugs on platelet function. Dutasteride and fnasteride (prescribed for benign prostatic hypertrophy) have been shown to cause genital abnormalities in male fetuses of experimental animals; there is no evidence of harm in humans. Recommendations for the deferral of prospective donors following transfusion are therefore consistent with other risk factors for infection. The Guideline Development Group agreed on the following recommendations based on their medical and scientifc knowledge and experience from best practice. Decision-making process There is no published evidence of transfusion-transmitted infection from a donor who was the recipient of a tissue transplant. In view of the theoretical risk, the Guideline Development Group agreed that the same recommendations should be applied as for recipients of labile blood components. The Guideline Development Group agreed on the following recommendations based on a precautionary deferral period of 12 months. Bacteremia following surgical dental extraction with an emphasis on anaerobic strains. Decision-making process There is no published evidence to guide recommendations regarding recent minor or major surgical procedures. The Guideline Development Group therefore agreed on the following recommendations based on the above studies and on their medical knowledge and experience from best practice. However, sexual contact is one of the main routes of infection among adolescents and adults in areas of low endemicity. Hepatitis C virus: molecular and epidemiological evidence of male-to-female transmission. In addition, direct blood contact in the household environment, from needlestick injuries and sharing of items, has resulted in transmission between partners and other household contacts. Based on the available evidence, and their medical and scientifc knowledge and expertise, the Guideline Development Group agreed on the following recommendations. Transfusion-acquired hepatitis A in a premature infant with secondary nosocomial spread in an intensive care nursery. Prevention of transfusion-transmitted hepatitis E by donor-initiated self exclusion. However, the retrospective reporting of diagnosed infections in the month following donation may prevent the issue of products that may transmit infection and/or enable the monitoring of treatment of recipients of such donations. The Guideline Development Group agreed on the following recommendations, based on the above papers, their medical and scientifc knowledge, and experience from best practice. The Guideline Development Group agreed on the following recommendations based on the above mentioned papers, their medical and scientifc knowledge and experience from best practice. Analysis of the infection system of human T-cell leukaemia virus type I based on a mathematical epidemic model. The appearance of circulating virus also coincides with that of circulating antibody. The Guideline Development Group agreed on the following recommendations based the above mentioned studies, on their medical and scientifc knowledge and experience from best practice. The transmission of other herpes viruses is not unknown, but not commonly reported. Although donors may have evidence of a range of herpesvirus infections, not all of these are likely to be relevant to transfusion. Only those herpes viruses with a proven viraemia in asymptomatic individuals are likely to be transmitted, but even then identifed transmission rates are not as high as might be expected. Transmission to immunocompetent individuals is unlikely to result in serious sequelae, if indeed a productive infection results. However, immunocompromised individuals are highly susceptible and infections are likely to have serious consequences. The Guideline Development Group agreed on the following recommendations based the above studies, on their medical and scientifc knowledge and experience from best practice. Infection is acute and rapid, but infected individuals would normally be asymptomatic whilst infectious. Infection is generally seasonal with cases occurring during the season when mosquitoes are most active. In endemic areas, all donors may require specifc screening if cases of transfusion transmission are to be avoided. Decision-making process Dengue and chikungunya are infectious agents which have been present for some time, but more recently have increased in signifcance in relation to transfusion transmission. Transfusion-transmissions of dengue and chikungunya have been reported, but are relatively low in number considering the number of infected individuals. In non-endemic countries, risk may often be mediated through existing malarial deferral policies; where this is not the case, individuals who have visited endemic areas should be deferred for a minimum of 28 days following their return. The Guideline Development Group agreed on the following recommendations based on the above studies, their medical and scientifc knowledge and experience from best practice. Measures to prevent transfusion-associated protozoal infections in non endemic countries. Documented cases of post-transfusion malaria occurring in England: a review in relation to current and proposed donor-selection guidelines. Decision-making process the Guideline Development Group agreed on the following recommendations based on data from the above studies, their expert knowledge and experience from best practice. Assessment of a travel Question to identify donors with risk of Trypanosoma cruzi: operational validity and field testing. Decision-making process In non-endemic countries, individuals with potential exposure to T. In endemic countries infected individuals can be identifed through antibody screening, but the possibility of recent infection where antibody has not yet become detectable must be considered. Individuals presenting as potential donors are likely to be asymptomatic and only those who have previously been diagnosed with babesiosis can be identifed and deferred. The Guideline Development Group agreed on the following recommendations based on data from the above studies, their expert knowledge and experience from best practice. Recommendation Defer permanently Individuals who have ever had a diagnosis of babesiosis 7. Decision-making process the identifcation of individuals at risk of leishmaniasis is not straightforward. Although travel to an endemic area is a clear risk, sand fies are not present all year round in many endemic areas. Those spending signifcant amounts of time in such areas may have been exposed, but are likely to remain asymptomatic for long periods of time, in some cases for longer than a year. The Guideline Development Group agreed on the following recommendations based on their expert knowledge and experience from best practice. Recommendations Defer Individuals who have spent extended periods in endemic areas: defer for at least 12 months since their last return 209 Defer permanently Individuals who have ever had a diagnosis of leishmaniasis 7. Decision-making process No publications were identifed that directly address the specifc questions. Recommendations Accept Household contacts of individuals with syphilis Defer Current sexual contacts of individuals with syphilis Former sexual contacts of individuals with syphilis: defer for 12 months since last sexual contact Individuals with gonorrhoea: defer for 12 months following completion of treatment and assess for high-risk behaviour Current sexual contacts of individuals with gonorrhoea Former sexual contacts of individuals with gonorrhoea: defer for 12 months since last sexual contact Defer permanently Individuals who have ever had a diagnosis of syphilis 7. Recommendation Defer permanently Individuals who have ever had a diagnosis of brucellosis 7. Decision-making process the Guideline Development Group agreed on the following recommendations based on the above study, their medical and scientifc knowledge and experience from best practice. Recommendations Defer Individuals with tuberculosis: defer for 2 years following confrmation of cure Contacts of individuals with tuberculosis: defer household contacts and other close contacts until screened and confrmed clear of infection 7. Decision-making process the Guideline Development Group agreed on the following recommendations based on this published article, their medical and scientifc knowledge and experience from best practice. Risk of acquiring Creutzfeldt-Jakob disease from blood transfusions: systematic review of case-control studies. Decision-making process the Guideline Development Group agreed on the following recommendations based on published literature, their medical and scientifc knowledge and experience from best practice. Three are risk/ beneft studies using mathematical modelling; seven are discussions of available evidence, two of which are by the same author. Evaluation of the de-selection of men who have had sex with men from blood donation in England. Moreover, the studies use epidemiological data from the developed world and the risk estimates are applicable only to the blood transfusion services in which they were carried out. Men having sex with men donor deferral risk assessment: an analysis using risk management principles. Scientifc background on the risk engendered by reducing the lifetime blood donation deferral period for men who have sex with men. Why are all men who have had sex with men even once since 1977 indefnitely deferred from donating blood However, he considered that a continued policy of permanent deferral was diffcult to justify on scientifc grounds, in the absence of evidence of increased risk resulting from a deferral period of fve years since last sexual activity.
Purchase generic prandin canada. What happens in LUNG DISEASE | Pollution Smoking Allergy Asthma | Dr.Education (HIndi + ENg).
Often managing diabetes 80mgdl generic prandin 0.5 mg free shipping, another child or adult touches a surface that has been contaminated and then touches their own mouth blood sugar vs blood glucose prandin 2mg with amex. A child with rotavirus infection may be contagious before the onset of diarrhea and for a few days after the diarrhea has ended diabetes diet chart pdf buy 0.5 mg prandin with amex. Although there is no specific therapy for rotavirus diarrhea diabetic diet ideas buy cheapest prandin and prandin, the most effective therapy is to encourage ill children to drink plenty of fluids to avoid dehydration blood glucose 300 purchase prandin 2mg visa. The virus causes fever blood sugar solution 10 day detox diet order generic prandin, swollen lymph nodes behind the ears, and a rash that starts on the face, spreads to the torso and then to the arms and legs. Rubella is no longer very common because most children are immunized beginning at 12 months of age. Rubella is not usually a serious disease in children, but can be very serious if a pregnant woman becomes infected. Infection with rubella in the first three months of pregnancy can cause serious injury to the fetus, resulting in heart damage, blindness, deafness, mental retardation, miscarriage, or stillbirth. Rubella is spread person-to-person by breathing in droplets of respiratory secretions exhaled by an infected person. It may also be spread when someone touches his or her nose or mouth after their hands have been in contact with infected secretions (such as saliva) from an infected person. A person can spread the disease from as many as five days before the rash appears to five to seven days after. People are considered immune only if they have received at least one dose of Rubella vaccine on or after their first birthday or if they have laboratory evidence of rubella immunity. Any children under 12 months who have not yet been vaccinated against rubella should be excluded until they have been immunized or until three weeks after the onset of rash in the last case. Exclude the infected child or adult until seven days after the onset of the rash or as directed by the Division of Public Health. Note: Notify the Division of Public Health, Office of Infectious Disease Epidemiology at 1-888-295 5156 if you become aware that a child or adult in your facility has developed Rubella. These bacteria are often found in the digestive tract of a variety of animals, as well as humans. Persons with Salmonella infections often experience fever, stomach cramps, nausea and vomiting, in addition to diarrhea. Salmonella is present in the feces of ill and recently recovered persons and infections may be spread from person to person. However, outbreaks in childcare settings are rare and most persons are believed to have acquired their infections from contaminated food. Some foods, such as chicken, come from naturally infected sources while others, such as tomatoes and some vegetables, are contaminated during processing. Food handlers may also contaminate food if they are infected and do not practice good hand hygiene in preparing food. Ordinarily safe foods, such as baked goods, may become contaminated from juices of uncooked foods such as poultry. Although it has been known that Salmonella may be present in cracked eggs for some time, it is only recently that salmonella has been found in uncooked whole eggs. Given sufficient moisture and temperatures between 40-140 C, small numbers of salmonella will quickly increase to the point where they can cause illness in a large numbers of persons. Some pets, especially turtles, lizards and birds, often carry Salmonella in their digestive tracts. While childcare providers are most likely to encounter this condition because of infection outside their facility, they need to be aware of good hand hygiene and food handling practices to prevent foodborne illness from occurring within their facility. Because of the risk of Salmonella infection, turtles, lizards, and other reptiles should not be kept as pets in childcare centers. Home-prepared snacks may be not only prepared under less than optimal circumstances but may be transported and stored under conditions that will allow bacteria to grow. Dairy products and liquid formula should also be kept refrigerated in order to limit the growth of bacteria, including Salmonella. Exclude any child or adult with Salmonella infection until symptoms resolve, usually 5 7 days or as directed by the Delaware Division of Public Health. Note: Notify the Division of Public Health, Office of Infectious Disease Epidemiology at 1-888-295 5156 if you become aware that a child or adult in your facility has developed Salmonella. Over-the-counter insecticide lotion treatments are available for killing the mites. If scabies is diagnosed in a child or adult in your facility: > Notify any other adults or the parents of children who may have had direct contact with the infected person. Other providers and children and their families may have been infected and may need treatment. If a person has had scabies previously, it will take only days for the rash to develop. A second treatment may be needed a week later Exclude the person until 24 hours after treatment has been completed. Only a few bacteria are needed to cause an infection and, unlike many of the diarrheal agents in childcare settings, Shigella may spread through groups of children who are toilet trained as well as through groups of children who are in diapers. Depending on the infectious dose, infection with Shigella may be very mild or it may result in severe bloody diarrhea, fever, cramping, nausea, and vomiting. Children may spread infections acquired in childcare facilities to their parents and siblings and whole families may be ill within a matter of days. Deaths have been reported from this illness and it is one of the more serious infections providers are likely to encounter in the childcare setting. Explain to them the value of handwashing with soap and running water in stopping the spread of infection in the home. In the absence of treatment with antibiotics, two negative cultures should be obtained before readmitting children. Note: Notify the Division of Public Health, Office of Infectious Disease Epidemiology at 1-888-295 5156 if you become aware that a child or adult in your facility has developed Shigellosis. Strep throat is easily spread when an infected person coughs or sneezes contaminated droplets into the air and another person inhales them. A person can also be infected from touching these secretions and then touching their mouth or nose. Symptoms of strep throat infections may include severe sore throat, fever, headache, and swollen glands. If not treated, strep infections can lead to scarlet fever, rheumatic fever, skin, bloodstream and ear infections, and pneumonia. A bright red, rough textured rash that spreads all over the childs body characterizes scarlet fever. If you suspect a case of strep throat in your childcare facility: > Call the parents to pick up the child and have her or him evaluated by their healthcare provider. Exclude a child diagnosed with strep throat until 24 hours after beginning antibiotic therapy. This recommendation from the American Academy of Pediatrics and the National Back to Sleep Campaign applies to most babies. However, some babies should lie in a prone position, such as those with respiratory disease, symptomatic gastro-esophageal reflux, or certain upper airway malformations. Do not smoke; provide a smoke-free environment for babies in your care; encourage parents who smoke to quit. Consumer Product Safety Commission has issued advisories for parents on the hazards to infants sleeping on beanbag cushions, sheepskins, foam pads, foam sofa cushions, synthetic-filled adult pillows, and foam pads covered with comforters. Dress your baby in light sleep clothing and keep the room at a temperature that is comfortable for an adult. Prepare to talk with law enforcement officers, a coroner or medical examiner, and licensing and insurance agencies. Children receive tetanus vaccine in combination with the pertussis and diphtheria vaccine. After childhood, adults need a booster injection every 10 years to assure they are protected. Any wound or cut contaminated with the soil and not open to the air (such as a puncture wound or even a rose prick) will provide a suitable environment for the bacteria. Tetanus is usually acquired when a person who has not been immunized acquires such a wound by stepping on a dirty nail or being cut by a dirty tool. Anyone who has an open wound injury should consult with their healthcare provider regarding the date of his or her last tetanus booster. A person, who has not had a booster within the past 10 years, should receive a booster dose of vaccine and/or other medications to prevent tetanus disease. For some wounds, a person may need a booster if more than five years have passed since the last dose. Note: Notify the Division of Public Health, Office of Infectious Disease Epidemiology at 1-888-295 5156 if you become aware that a child or adult in your facility has developed Tetanus. Parents should discuss and follow the recommendations of their childs healthcare provider. The urinary tract includes: Kidneys which form the urine from liquid waste in the blood Ureters tubes that carry urine from the kidneys to the bladder Bladder which stores urine Urethra where urine exits the body the most common urinary tract infections are caused by bacteria from feces on the skin that enter through the urethra to infect the bladder, particularly in girls. Anything that irritates the opening of the urethra can make it easier for infection to occur. In girls, the urethra is much shorter than in boys, so infection from the outside into the bladder occurs more easily. Bathing in soapy water or a bubble bath can be irritating and predispose girls to getting urinary tract infections. Signs and symptoms of urinary tract infections include pain when urinating, increased frequency of urinating, fever, cloudy or reddish urine and loss of potty training after the child has had good control of urine for a period of time, especially when loss of control occurs in the daytime with little warning. Ignoring urinary tract infections can lead to kidney damage, even if the symptoms seem to go away by themselves. Diluting the urine gives bacteria less food to grow and makes it easier for the body to fight the infection. Anyone can become infected with the virus if bitten by an infected mosquito, but children need adult help in taking precautions against mosquito bites. Parents and caregivers should take the following precautions to help protect children from getting mosquito bites. If children take a field trip to an area where there are weeds, tall grass, bushes or known high mosquito activity, or if the trip is at dusk, during the evening, nighttime or at dawn, students should be advised to wear long pants, long sleeves and socks to minimize the possibility of exposure to mosquitoes. Mosquitoes can enter homes through unscreened windows or doors, or broken screens. These organisms are part of the germs normally found in various parts of the body and ordinarily do not cause any symptoms. Certain conditions, such as antibiotic use or excessive moisture, may upset the balance of microbes and allow an overgrowth of Candida. However, in newborns or persons with weak immune systems, this yeast can cause more serious or chronic infections. Many of those that escape this infection soon acquire Candida from close contacts with family members, relatives, and friends. These early exposures may result in an oral infection (thrush) that appears as creamy white, curd-like patches on the tongue and inside of the mouth. In older persons, treatment with certain types of antibiotics or inhaled steroids may upset the balance of microbes in the mouth, allowing an overgrowth of Candida that will also result in thrush. Outbreaks of thrush in childcare settings may be the result of increased use of antibiotics rather than newly acquired Candida infections. Candida may also exacerbate diaper rash, as this yeast grows readily on damaged skin. The infected skin is usually fiery red with lesions that may have a raised red border. Children who suck their thumbs or other fingers may occasionally develop Candida around their fingernails. Oral thrush and Candida diaper rash are usually treated with the antibiotic, nystatin. A corticosteroid cream can be applied to highly inflamed skin lesions on the hands or diaper areas. For children with diaper rash, childcare providers should change the diaper frequently, gently clean the childs skin with water and a mild soap and pat dry. While cornstarch or baby powder may be recommended for mild diaper rash, it should not be used for children with inflamed skin. Plastic pants that do not allow air to circulate over the diaper area should not be used, although the diapering system should be able to hold urine or liquid stool.
Antimicrobial treatment is most effective when children are treated during the frst week of illness diabetes prevention medication buy prandin 0.5 mg visa. If the disease remains untreated during the second week diabetes symptoms excessive sweating buy prandin 2mg, therapy is less effective in preventing complications diabetes symptoms headache buy discount prandin 2mg line. The causative agents of some of these infections share the same group antigen as Rickettsia rickettsii diabetes in dogs fits discount 1mg prandin free shipping. These diseases are of importance among people traveling to or returning from areas where these agents are endemic and among people living in these areas diabete 0 90 order cheapest prandin and prandin. The rash develops 1 to 4 days after onset of fever and 3 to 10 days after appearance of an eschar at the site of the bite of a house mouse mite diabetes type 2 reversal purchase prandin cheap. Fluoroquinolones and chloramphenicol are alternative drugs, although fuoroquinolones are not approved for this use in children younger than 18 years of age (see Fluoroquinolones, p 800). Rodent-control measures are important in limiting or eliminating spread of rickettsialpox; however, they should be conducted only in conjunction with acaricide application to ensure vector control. Fever, myalgia, severe headache, nausea, vomiting, and anorexia are typical presenting symptoms. The rash usually begins within the frst 6 days of symptoms as erythematous macules or maculopapules. Rash usually appears frst on the wrists and ankles, often spreading within hours proximally to the trunk and involves the palms and soles. Delay in appropriate antimicrobial treatment is associated with severe disease and poor outcomes. Patients treated early in the course of symptoms may have a mild ill ness, with fever resolving in the frst 48 hours of treatment. Other wild animals and dogs have been found with antibodies to Rickettsia rickettsii, but their role as natural reservoirs is not clear. Mortality is highest in males, people older than 50 years of age, children 5 to 9 years of age, and people with no recognized tick bite or attachment. Most cases are reported in the south Atlantic, southeastern, and south central states, although most states in the contiguous United States record cases each year. The acute sample should be taken early in the course of illness, preferably in the frst week of symptoms, and the convalescent sample should be taken 2 to 3 weeks later. Both IgG and IgM antibodies begin to increase around day 7 to 10 after onset of symp toms; therefore, an elevated acute titer may represent past exposure rather than acute infection. Currently, commercially available enzyme immunoassays are not quantitative, cannot be used to evaluate changes in IgG titer, and should not be used for monitoring titer changes. Sensitivity of skin biopsy testing decreases greatly after the frst 24 hours of appropriate treatment. Treatment is most effective if started in the frst few days of symptoms, and treatment started after the ffth day of symptoms is less likely to prevent death or other adverse outcomes. Use of chloramphenicol should be considered only in rare cases, such as severe doxycycline allergies or during pregnancy. If the mothers life is in danger, doxycycline may be considered and the theoretical risk to the fetus should be discussed with the patient. These exceptions should be considered on a case-by-case basis, and the risks and benefts should be discussed with the patient. Antimicrobial treatment should be continued until the patient has been afebrile for at least 3 days and has demon strated clinical improvement; the usual duration of therapy is 7 to 10 days. If a tick-infested area is entered, people should wear protective clothing and apply tick or insect repellents to clothes and exposed body parts for added protection. All pets should be treated for ticks according to veterinary guidelines and untreated animals should be excluded to prevent the yard and home from becoming a suitable habitat for ticks. Adults should be taught to inspect themselves, their children (bodies and clothing), and pets thoroughly for ticks after spending time outdoors during the tick season and to remove ticks promptly and properly (see Prevention of Tickborne Infections, p 207). In moderate to severe cases, dehydration, electrolyte abnormalities, and acidosis may occur. In certain immunocompromised children, including children with severe con genital immunodefciencies or children who are hematopoietic stem cell or solid organ transplant recipients, persistent infection and diarrhea can develop. Rotavirus is present in high titer in stools of infected patients several days before and several days after onset of clinical disease. Rotavirus can be found on toys and hard surfaces in child care centers, indicating that fomites may serve as a mechanism of transmission. Rarely, common-source outbreaks from contaminated water or food have been reported. The epidemiology of rotavirus disease in the United States has changed dramatically since rotavirus vaccines became available in 2006. There also were substantial reductions in offce visits for gastroenteritis during this time period. Orally administered Human Immune Globulin, administered as an investigational therapy in immunocompromised patients with prolonged infection, has decreased viral shedding and shortened the dura tion of diarrhea. General measures for interrupting enteric transmission in child care centers are available (see Children in Out-of-Home Child Care, p 133). There is no evidence that this virus is a safety risk or causes illness in humans. Some studies performed outside the United States have detected a low level of increased risk of intussusception following rotavirus immunization shortly after the frst dose. Although an increased risk of intussusception from rotavirus vaccine has not been documented in the United States, data currently available cannot exclude a risk as low as that detected in other locations. However, immunization should not be deferred if the product used for previ ous doses is not available or is unknown. In this situation, the health care professional should continue or complete the series with the product available. Preterm infants should be immunized on the same schedule and with the same precautions as recommended for full-term infants. The potential risk of transmission of vaccine virus should be weighed against the risk of acquiring and transmitting natural rotavirus. Lymphadenopathy, which may precede rash, often involves posterior auricular or suboccipital lymph nodes, can be generalized, and lasts between 5 and 8 days. Mild forms of the disease can be associated with few or no obvious clinical manifestations at birth. Congenital defects occur in up to 85% if mater nal infection occurs during the frst 12 weeks of gestation, 50% during the frst 13 to 16 weeks of gestation, and 25% during the end of the second trimester. Postnatal rubella is transmit ted primarily through direct or droplet contact from nasopharyngeal secretions. Although volunteer studies have demonstrated rubella virus in nasopharyngeal secretions from 7 days before to 14 days after onset of rash, the period of maximal com municability extends from a few days before to 7 days after onset of rash. A small number of infants with congenital rubella continue to shed virus in nasopharyngeal secretions and urine for 1 year or more and can transmit infection to susceptible contacts. Before widespread use of rubella vaccine, rubella was an epidemic disease, occur ring in 6 to 9-year cycles, with most cases occurring in children. The incidence of rubella in the United States has decreased by more than 99% from the prevaccine era. Among children and adolescents 6 through 19 years of age, seroprevalence was approximately 95%; however, approxi mately 10% of adults 20 through 49 years of age lacked antibodies to rubella, although 92% of women were seropositive. The incubation period for postnatally acquired rubella ranges from 14 to 21 days, usually 16 to 18 days. For diagnosis of postnatally acquired rubella, a fourfold or greater increase in antibody titer or seroconversion between acute and convalescent IgG serum titers also indicates infection. The hemagglutination-inhibition rubella antibody test, which previously was the most commonly used method of serologic screening for rubella infection, generally has been supplanted by a number of equally or more sensitive assays for determining rubella immunity, including enzyme immunoassays and latex agglutination tests. The presence of high-avidity IgG or lack of increase in IgG titers can be useful in identifying false-positive rubella IgM results. The avidity assay is not a routine test and should be performed in reference laboratories. Rubella virus can be isolated most consistently from throat or nasal specimens (and less consistently, urine) by inoculation of appropriate cell culture. Most postnatal cases are positive virologically on the day of symptom onset, and most congenital cases are positive virologically at birth. Laboratory personnel should be notifed that rubella is suspected, because specialized testing is required to detect the virus. Blood, urine, and cataract specimens also may yield virus, particularly in infants with congenital infection. Children with postnatal rubella should be excluded from school or child care for 7 days after onset of the rash. During an outbreak, children without evi dence of immunity should be immunized or excluded. All birth defects in which rubella infection is suspected etiologically should be investigated thoroughly and reported to the Centers for Disease Control and Prevention through local or state health departments. When a pregnant woman is exposed to rubella, a blood speci men should be obtained as soon as possible and tested for rubella antibody (IgG and IgM). An aliquot of frozen serum should be stored for possible repeated testing at a later time. The presence of rubella-specifc IgG antibody in a properly performed test at the time of exposure indicates that the person most likely is immune. Immunization of exposed nonpregnant people may be indi cated, because if the exposure did not result in infection, immunization will protect these people in the future. Immunization of a person who is incubating natural rubella or who already is immune is not associated with an increased risk of adverse effects. Vaccine can be given simultaneously with other vaccines (see Simultaneous Administration of Multiple Vaccines, p 33). At least 1 dose of live-attenuated rubella-containing vac cine is recommended for people 12 months of age or older. Special emphasis must continue to be placed on the immunization of at-risk postpu bertal males and females, especially college students, military recruits, recent immigrants, health care professionals, teachers, and child care providers. Clinical diagnosis of infection is unreliable and should not be accepted as evidence of immunity. If a woman is found to be susceptible, rubella vaccine should be administered during the immediate postpartum period before discharge. Joint involvement usually begins 7 to 21 days after immunization and generally is transient. The incidence of joint manifestations after immunization is lower than that after natural infection at the corresponding age. The maximal theoretical risk for occurrence of congenital rubella is estimated to be 1. In view of these observations, receipt of rubella vaccine during pregnancy is not an indication for termination of pregnancy. Immunizing susceptible children whose mothers or other household contacts are pregnant does not cause a risk. However, if other manifestations suggest a more serious illness, the child should not be immunized until recovery has occurred. Immunocompromised patients with disorders associated with increased severity of viral infections should not receive live-virus rubella vaccine (see Immunocompromised Children, p 74). The risk of rubella expo sure for patients with altered immunity can be decreased by immunizing their close susceptible contacts. Although small amounts of virus are shed after immunization, no evidence of transmission of vaccine virus from immunized children has been found. For patients who have received high doses of corticosteroids (2 mg/kg or greater or more than 20 mg/day) for 14 days or more and who otherwise are not immunocompromised, the recommended interval before immunization is at least 1 month (see Immunocompromised Children, p 74) after steroids have been discontinued. The most common illness associated with nontyphoidal Salmonella infection is gastroenteritis, in which diarrhea, abdominal cramps, and fever are common manifestations. Salmonella enterica serotypes Typhi, Paratyphi A, Paratyphi B, and certain other uncommon serotypes can cause a protracted bacteremic illness referred to , respectively, as typhoid and paratyphoid fever and collectively as enteric fevers. The onset of enteric fever typically is gradual, with manifestations such as fever, constitutional symptoms (eg, headache, malaise, anorexia, and lethargy), abdominal pain and tenderness, hepato megaly, splenomegaly, dactylitis, rose spots, and change in mental status. The major food vehicles of transmission to humans include food of animal origin, such as poultry, beef, eggs, and dairy products. Unlike nontyphoidal Salmonella serotypes, the enteric fever serotypes (Salmonella serotypes Typhi, Paratyphi A, Paratyphi B) are restricted to human hosts, in whom they cause clinical and subclinical infections. Chronic human carriers (mostly involving chronic infection of the gall bladder but occasionally involving infection of the urinary tract) constitute the reservoir in areas with endemic infection. In the current taxonomy, only 2 species are recognized, Salmonella enterica and Salmonella bongori. S enterica has 6 subspecies, of which subspecies I (enterica) contains the overwhelming majority of all Salmonella pathogens that affect humans, other mam mals, and birds. Serotypes are now written nonitalicized with a capital frst letter (eg, Typhi, Typhimurium, Enteritidis). Consequently, typhoid fever and paratyphoid fever infections in residents of the United States usually are acquired during international travel. Age-specifc incidences for nontyphoidal Salmonella infection are highest in children younger than 4 years of age. Most reported cases are sporadic, but widespread outbreaks, includ ing health care-associated and institutional outbreaks, have been reported. The incidence of nontyphoidal Salmonella gastroenteritis has diminished little in recent years, in contrast to other enteric infections of bacterial etiologies. Every year, nontyphoidal Salmonella organisms are one of the most common causes of laboratory-confrmed cases of enteric disease reported by the Foodborne Diseases Active Surveillance Network (FoodNet [ Twelve weeks after infection with the most common nontyphoidal Salmonella serotypes, approximately 45% of children younger than 5 years of age excrete organisms, compared with 5% of older children and adults; antimicrobial therapy can prolong excretion. Approximately 1% of adults con tinue to excrete Salmonella organisms for more than 1 year.