Jacquelyn Gayle Bolwell, MD
- Medical Instructor in the Department of Medicine

https://medicine.duke.edu/faculty/jacquelyn-gayle-bolwell-md
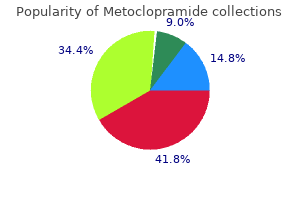
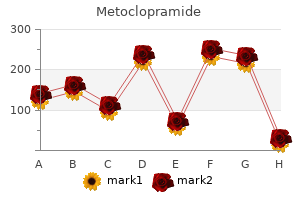
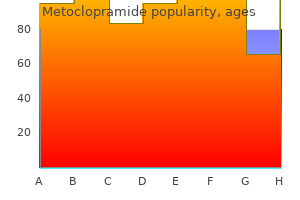
In general gastritis blog buy generic metoclopramide 10mg, in the presence of chronic febrile diarrhea gastritis icd 9 buy discount metoclopramide 10mg, it is important to carefully palpate the colon and the ileocecal region gastritis diet ìîëîäåæêà order 10 mg metoclopramide with mastercard. Abdominal examination in chronic diarrhea starts with the right iliac fossa to reveal possible ultrasound changes in the terminal ileum chronic gastritis medicine order 10mg metoclopramide with mastercard. Upper digestive endoscopy should follow for the detection of concomitant esogastro-duodenal lesions gastritis diet ocd order metoclopramide 10 mg overnight delivery. In the affected area gastritis diet soy sauce order generic metoclopramide pills, an obvious narrowing of the lumen can be seen, sometimes with upstream dilatation. Other signs of lymphoma may be detected: lymph nodes in various locations or splenomegaly. Ultrasound monitoring under treatment is useful for the evaluation of the therapeutic response. In about 30% of the cases, acute pain has an atypical location or radiation, symptoms can be mild, and leukocytosis can be at the limit. In these situations, a correct diagnosis is imperative: is it or is it not an acute appendicitisfi Experience in appendicular ultrasound is achieved by clinical, imaging, surgical correlations. Operators trained for the ultrasound visualization of the appendix will be able to see it in up to 50-70% of cases, under normal conditions. The ultrasound appearance in acute appendicitis is characterized by an appendicular diameter larger than 6 mm or by visualization of an appendicolith. For the ultrasound diagnosis of acute appendicitis, Goudet proposed major and minor diagnostic criteria. A positive diagnosis of acute appendicitis is considered when at least one major and two minor ultrasound criteria are met. The ultrasound differential diagnosis of acute appendicitis should be made with terminal ileitis, cecum cancer, mesenteric adenitis and right adnexal pathology in women. In conclusion, the ultrasound of the appendix is an adjuvant method for clinical diagnosis, particularly in atypical cases of acute appendicitis. In a typical clinical presentation with pain in the right iliac fossa and leukocytosis, no ultrasound confirmation is needed. In atypical cases, training will enable the use of ultrasound for supporting the positive diagnosis of acute appendicitis. In the presence of such a clinical presentation, the ideal investigation is colonoscopy. On the other hand, the most digestive patients are initially subjected to abdominal ultrasound examination, aimed at providing additional diagnostic elements. Careful abdominal palpation may reveal a mass situated along the colon that should subsequently be evaluated by ultrasound. They are often detected in a late stage, due to complications (most frequently intestinal obstruction) or after the diagnosis of liver metastases. In a palpable abdominal tumor, ultrasound examination may also detect an aerated tumor, belonging to the colon. In an iron deficiency anemia, the possibility of a colon tumor should be considered; if accompanied by rectal bleeding, it will be probably situated in the left colon, if not it will be probably situated in the right colon. The colon wall changed by the tumor appears as hypoechoic, with variable thickness (10-30 mm), with a symmetrical or eccentric appearance. Genrally, any tumor detected by ultrasound that contains air belongs to the digestive tract. Lymph nodes (round or oval hypoechoic images) can be seen in the vicinity of the tumor. Liver ultrasound examination is compulsory in order to confirm or exclude liver metastases. A transabdominal ultrasound technique for the evaluation of the colon is hydrocolonic sonography. After the colon is prepared the same way as for endoscopic examination, an enema with 1500 ml water is performed, possibly preceded by injection of Buscopan. The water in the enema allows for a good visualization of the colonic lumen that will become anechoic. Thus, an experienced examiner will be able to see polyps larger than 5-10 mm, as well as possible colon tumors. Also, in elderly patients, sphincter incontinence is often present, which makes the examination impossible (an inflatable rectal balloon catheter can be used for occlusion during examination). It is a relatively frequent disease in Romania and should be taken into consideration whenever there is an association of these symptoms. The endoscopic appearance is typical, rectal involvement is always present in the form of blood seeping mucosa. After the diagnosis, the extension of the disease should be assessed, which can be done by endoscopy or by ultrasound. This is why recto-sigmoidoscopy with biopsy is preferred for positive diagnosis, while the extension can be evaluated by transabdominal colonic ultrasound. A hyperchoic thickening of the inner layer (mucosa and submucosa) can be seen (Figs. The normal haustra of the colon (better visualized by hydrocolonic sonography) also disappear. In the diagnosis of ulcerative colitis, transabdominal ultrasound examination will start from the rectum upwards, noting the place up to which there are pathological changes in the colon. Diverticulosis is a common disorder, but its complications such as diverticulitis or diverticular bleeding are rare. The clinical presentation of diverticulitis is similar to that of acute appendicitis (pain, leukocytosis, possibly fever) most frequently the pain being located in the left iliac fossa since diverticula occur mostly in the sigmoid colon. In a clinical suspicion of diverticulitis, ultrasound can be the first line imaging method to use. It will demonstrate a hypoechoic area (the inflamed diverticulum) in contact with the colon (Fig. The size of the hypoechoic area is usually 1-4 cm, but in abscesses, it can be even larger. The pressure of the ultrasound probe on that particular area induces intense pain. In conclusion, we must mention that the chapter on ultrasound of the digestive tract has an informative purpose for beginners, but can become part of clinical practice for experienced ultrasonographists. The first part deals with how to examine the digestive tube using transabdominal ultrasound. Within this stratification, both organizations propose a beginner ultrasonographist level (ultrasound practice level I), then an advanced level, and finally, an expert level. We consider this classification very useful, as the beginner will have to differentiate between normal and pathological in ultrasound, the advanced ultrasonographist will be able to elucidate most of pathological aspects, while the expert will diagnose difficult cases. Starting from the average size of these organs, the differential diagnosis of acute vs. The kidney ultrasound approach can be through the loins (the patient in ventral decubitus), by lateral approach (right lateral decubitus for the examination of the left kidney and scanning is performed through the left lateral abdominal region), or through sagittal sections in a patient in dorsal decubitus. The right kidney is easier to visualize in lateral sections or while the patient is in dorsal decubitus, using the liver as a sonographic window. The normal ultrasound anatomy of the kidney includes the evaluation of the pyelum and the evaluation of the parenchyma (cortex). The ultrasound distinction between the cortex and the medulla is possible only in children and thin persons. In current practice, this distinction is not possible, so the pyelum and the parenchyma will be discussed in relationship to the kidney. In transverse section, approximately in the middle of the kidney, the renal hilum with the renal artery and vein can be 143 seen. The operator should know the anatomy of this region in order to be able to assess the vascular structures, if a venous (tumor) thrombosis or a renal artery stenosis are suspected. Thus, the size of the kidneys decreases with age (renal senescence) or in chronic kidney failure; the kidneys can be enlarged in acute renal failure, in some diseases such as amyloidosis or diabetes mellitus, etc. Measurement of the three renal axes (length, width and thickness) will allow estimation of the kidney volume, which is much more reliable than measurement of the long renal axis alone. Kidney ultrasound examination is part of the routine of every abdominal ultrasound examination. We consider that every abdominal ultrasound must be complete and examine all visible abdominal organs (gallbladder, common bile duct, intrahepatic bile ducts, liver, pancreas, spleen, kidneys, urinary bladder and pelvis, retroperitoneum), not just one organ. This will allow to detect anomalies which often have important clinical significance. The symptoms leading to kidney ultrasound examination are: colicky or dull pain in the lumbar region, hematuria, polakiuria, dysuria, signs of kidney failure, palpation of a tumor mass in the renal areas. In case of a tumor, locoregional invasion will be established, and for cysts, it will be determined whether they are isolated or part of a polycystic disorder: renal, or hepato-renal, or hepato-renal-pancreatic. When discussing kiney ultrasound examination, some normal entities that can pose difficult differential diagnosis problems should be described. Fetal renal lobulation may persist in adults and will generate a bosselated renal outline on ultrasound. Differential diagnosis should be made with a renal tumor (which usually is a circumscribed lesion with a different echogenicity from that of the kidney). It is a hypoechoic mass that protrudes from the cortex towards the renal pelvis (Figs. It continues the renal cortex, is well delimited towards the pyelum and usually less than 3 cm in size. Ultrasound differentiation should be made with a renal tumor, which is poorly delimitted and has a different echogenicity from that of the cortex. Renal cysts can be single or multiple (rarely more than 5 cysts in a kidney) and have variable sizes (between 1 and 10 cm). Intracystic hemorrhage is rarely possible and the cyst will change from anechoic to partially or completely hypoechoic. In clinical practice, the patient with a simple renal cyst must be assured is not a dangerous condition, of the fact that this disorder is benign, that it does not require medical or surgical treatment and that ultrasound monitoring (once or twice per year) is sufficient, also that they are not a cause for lumbar pain. Polycystic kidney is sometimes associated with polycystic liver, and much more rarely, with pancreatic or splenic polycystosis. In most cases, it is a congenital autosomal dominant disease, which is incidentally detected at the age of 30-50 years, following a hematuria episode, during the work-up of arterial hypertension or after the palpation of abdominal tumor masses. As a rule, this disease evolves into chronic renal failure, requiring hemodialysis. If a person with polycystic kidney is detected, all his/hers offspring should be examined by ultrasound to search for the disease. It is considered that if until the age of 20 years no renal cysts have developed in an offspring, he/she has not inherited the disease. The ultrasound appearance of polycystic kidneys is specific: bilateral involvement, large, poorly circumscribed kidneys, with the presence of tens of renal cysts of variable sizes (genrally 1-8 cm). Differential diagnosis can be made with multiple simple renal cysts (usually maximum 5-10 in a kidney), hydronephrosis, or with renal hydatid cysts with daughter vesicles (single cyst image with thick inner septa). The incidental ultrasound detection of renal polycystosis will be followed by the assessment of renal functional (urea, creatinine, creatinine clearance), to search for a potential renal failure. Also, the offspring of a patient with polycystic kidney disease will undergo ultrasound screening. It is recommended to refer the patient with renal polycystosis (or hepato-renal polycystosis) to the nephrologist, who will establish the monitoring strategy, given that in 5-10% of chronic hemodialysis cases, patients have a diagnosis of polycystic kidney disease. The ultrasound appearance is not typical, because cysts are extremely small and difficult to see by ultrasound. Kidney stones can be formed by calcium oxalate, calcium phosphate, ammonium-magnesium phosphate, uric acid or cysteine. Their formation depends on the family or personal predisposition, urinary salt concentration, change of urinary pH, presence of urinary infections, urinary tract anomalies. The clinical presentation of kidney stones is most often of a common renal colic (intense pain in the lumbar region radiating to the pelvis, in the presence of pollakiuria, dysuria), hematuria, recurrent urinary infections. In some cases, kidney stones can be completely asymptomatic and are incidentally detected on ultrasound.
During this procedure gastritis diet ùâ discount 10 mg metoclopramide mastercard, the physician is able to see two sets of images gastritis or pancreatitis buy cheap metoclopramide 10mg line, the endoscopic image of the duodenum and major papilla gastritis root word order metoclopramide discount, and the fluoroscopic image of the biliary and pancreatic ducts gastritis symptoms and treatments buy generic metoclopramide 10mg line. The right hand is responsible for advancing gastritis diet õ??õýëäýéí generic 10mg metoclopramide with visa, withdrawing and torquing the insertion tube gastritis symptoms in toddlers order cheap metoclopramide on-line. Lithotripsy devices, for both mechanical and electrohydraulic lithotripsy, may be inserted through the scope. These devices are used when stones are large and need to be broken into smaller pieces to facilitate removal or when the end of the bile duct is too narrow to allow easy stone removal. Video cameras may also be attached for full-color motion picture viewing during endoscopic procedures, or for later review. From a position in the stomach or duodenum, the endoscope allows visualization of the pancreas and adjacent structures (Figure 14). Each treatment option has different outcomes for patients presenting with different clinical characteristics. Symptomatic patients should be treated to relieve their symptoms and prevent the development of complications in the future. There is no benefit to prophylactic treated; asymptomatic patients should be managed expectantly. Medical Therapy Several medical treatment options are available for symptomatic gallstones. Surgical Therapy Cholecystectomy is the only definitive treatment for symptomatic gallstones. While open cholecystectomy was the standard surgical option for patients in the past, laparoscopic cholecystectomy has replaced the open procedure as the treatment option of choice in all but a few instances. Laparoscopic cholecystectomy is a minimally invasive procedure in which the surgeon makes a few small incisions in the abdomen and uses a small video camera to magnify the organs of the abdominal cavity. Using the video monitor to guide his actions, the surgeon identifies, isolates, and removes the gallbladder from its connections to the liver and bile ducts through the laparoscope (Figure 15). The procedure does not involve a large abdominal incision and results in less pain, shorter hospital stay, and fewer days missed from work. On occasion, the surgeon may begin a procedure using the laparoscopic approach and then may have to convert to an open procedure because of the presence of scarring, infection, or variant biliary anatomy. These shock waves are transmitted through water and tissue and have the ability to generate compressive and tensile waves. Disintegration and fragmentation of the gallstones occurs by producing forces strong enough to fracture the stones. The side effects of this procedure include abdominal wall and skin changes (ecchymosis, petechiae), pain, hematuria, nausea, emesis, and biliary colic. Fragmentation of large stones by a fluoroscopically guided mechanical lithotripsy device can be achieved in most cases, and complete ductal clearance is frequently successful. Percutaneous Therapy In high-risk patients with acute calculous diseases, surgical intervention may be associated with increased morbidity and mortality. Studies have demonstrated that the transperitoneal approach to the gallbladder is more difficult because of interposing right colon or liver, and consequently, it is employed in less than 20% of patients. Percutaneous cholecystolithotomy involves puncturing the gallbladder, dilating the tract, and removing any gallstones with a cholecystoscope. The advantages of this procedure are the immediate removal of uncrushed gallstones, the production of little gallstone debris, and the reduction of danger associated with sludge entering the cystic duct. Monooctanoin was shown to have high in vitro activity in dissolving cholesterol stones but is less efficient in vivo. Both solvents may continue to have some role in the care of patients with symptomatic gallstones who are poor surgical candidates. Endoscopic Gallbladder Stenting Endoscopic gallbladder stenting is another nonsurgical approach to treatment of gallstones that may be useful in high-risk patients. A hydrophilic wire is passed from the ampulla of Vater into the common bile duct and into the gallbladder through the cystic duct. Additionally, unlike other procedures that leave the gallbladder intact, further stone formation does not hinder the effectiveness of endoscopic stenting. Acute Cholecystitis the most common complication of gallstones is acute cholecystitis. Acute cholecystitis is usually caused by impaction of a gallstone in the cystic duct. Whereas gallstones in the gallbladder usually result in relatively benign conditions such as recurrent biliary colic or acute cholecystitis, choledocholithiasis can result in life-threatening conditions such as cholangitis (bacterial infection of obstructed bile) or acute pancreatitis. If cholangitis develops, pain, jaundice, fever, mental confusion, lethargy and delirium may all be present. Leukocytosis, elevations in bilirubin and alkaline phosphatase, and positive blood cultures are also present. Percutaneous removal of common bile duct stones using: A, balloon dilation catheter; B, balloon extraction catheter. Approximately 15% of the adult population are thought to have gallstone disease, and most of these people experience no symptoms. For a small proportion of people with gallstone disease, the stones irritate the gallbladder or block part of the biliary system, and this can cause symptoms such as pain, infection and inflammation. If these symptoms are left untreated, gallstones can cause more serious and in some cases life-threatening conditions such as cholecystitis, cholangitis, pancreatitis and jaundice. Some people with symptomless gallstone disease are offered treatment to prevent symptoms developing in the future, whereas others are offered a watch-and-wait approach. When people experience symptoms of gallstone disease they often need surgery to remove their gallbladder. In addition, if surgery is appropriate there is uncertainty about whether it should be performed as soon as possible after a gallstones attack or delayed until any infection and inflammation has subsided. This guideline addresses some of these uncertainties and provides recommendations about how gallstone disease should be identified, diagnosed and managed in adults. Patients should have the opportunity to make informed decisions about their care and treatment, in partnership with their healthcare professionals. If someone does not have capacity to make decisions, healthcare professionals should follow the code of practice that accompanies the Mental Capacity Act and the supplementary code of practice on deprivation of liberty safeguards. Reassure people with asymptomatic gallbladder stones found in a normal gallbladder and normal biliary tree that they do not need treatment unless they develop symptoms. Offer early laparoscopic cholecystectomy (to be carried out within 1 week of diagnosis) to people with acute cholecystitis. Reconsider laparoscopic cholecystectomy for people who have had percutaneous cholecystostomy once they are well enough for surgery. The full guideline gives details of the methods and the evidence used to develop the guidance. Terms used in this guideline Asymptomatic Stones that are found incidentally, as a result of imaging gallstones/ investigations unrelated to gallstone disease in people who have asymptomatic been completely symptom free for at least 12 months before common bile duct diagnosis. Why this is important In the evidence reviewed for this guideline, there was a lack of randomised controlled trials of intraoperative cholangiography, and the evidence that was available did not support the knowledge and experience of the Guideline Development Group. Therefore, there is a need for large, high-quality trials to address clinical questions about the benefits and harms of intraoperative cholangiography. It is unclear what effect the timing of laparoscopic cholecystectomy has on clinical outcomes and resource use. Why this is important There is a lack of information on the long-term impact of cholecystectomy on patient outcomes. Many patients report a continuation of symptoms or the onset of new symptoms after laparoscopic cholecystectomy, and these affect quality of life. The team established a Guideline Development Group (see section 4), which reviewed the evidence and developed the recommendations. Strength of recommendations Some recommendations can be made with more certainty than others. The Guideline Development Group makes a recommendation based on the trade-off between the benefits and harms of an intervention, taking into account the quality of the underpinning evidence. For some interventions, the Guideline Development Group is confident that, given the information it has looked at, most patients would choose the intervention. The wording used in the recommendations in this guideline denotes the certainty with which the recommendation is made (the strength of the recommendation). This discussion aims to help them to reach a fully informed decision (see also Patient-centred care). Other versions of this guideline the full guideline, Gallstone disease, contains details of the methods and evidence used to develop the guideline. Implementation Implementation tools and resources to help you put the guideline into practice are also available. Healthcare professionals are expected to take it fully into account when exercising their clinical judgement. However, the guidance does not override the individual responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or guardian or carer, and informed by the summaries of product characteristics of any drugs. Implementation of this guidance is the responsibility of local commissioners and/or providers. Commissioners and providers are reminded that it is their responsibility to implement the guidance, in their local context, in light of their duties to have due regard to the need to eliminate unlawful discrimination, advance equality of opportunity and foster good relations. Nothing in this guidance should be interpreted in a way that would be inconsistent with compliance with those duties. We considered within-study risk of bias (methodological quality), directness of evidence, heteroGallstones or cholelithiasis are a major public health problem in geneity, precision of effect estimates, and risk of publication bias. Europe and other developed countries and affect up to 20% of the Each recommendation has been qualified by giving the grade of population. The evidence is nal disorder for which patients are admitted to hospitals in graded as follows: (A) high quality evidence: further research is European countries [1]. In contrast, primary prevention and may change the estimate (downgraded randomized trials for this common disease is still in its infancy. Prevention of gallstones very uncertain about the estimate (case series/case reports, 2. These guidelines have been produced using evidence from Both cholesterol and pigment gallstone diseases originate from PubMed and Cochrane database searches until September 2015. Sevuptake of cholesterol [53] predisposing to increased secretion of bileral risk factors exist for cholesterol, pigment and mixed galliary cholesterol [54] and decreased secretion of bile acids (both constones. SuchconPolyand monounsaturated fats [77], and specifically nut ditions represent additional targets for the prevention of gallstones. After 5 and 14 years, 135 tive effects of alcohol consumption on gallstone formation (uncomplicated) and 290 (complicated) incident cases of sympto[31,78,79], and multifactorial analysis indicated that Danish patients matic gallstones were recorded, respectively (68% women). The latter effect disease in the general population, apart from high risk groups might increase the risk of gallstone disease. Incidence of gallstone formation also a causal risk factor for symptomatic gallstone disease [30]. Weight cycling is also a modest major concern was the poor therapeutic outcome due to lack of independent risk factor for gallstone formation [48,82,132,140]. Appropriate fat content (at least 7 g/day) in very-low-calorie No indication exists for aspirin use to prevent gallstone recurdiets might improve gallbladder motility and decrease the risk rence [167]. Patients undergoing rapid weight loss are more likely to become symptomatic for gallstones, with incidence Should prophylactic cholecystectomy be performed during reaching 28% to 71% after gastric bypass [27,150,151,155,156]. Caution is therefore recommended in prescribing prevention can be given (very low quality evidence; different types of continuous hormone therapy for controlling weak recommendation) menopausal symptoms. The natural history of asymptomatic gallstones suggests that most remain asymptomatic throughout life. Although bil(very low quality evidence; weak recommendation) iary pain has a positive likelihood ratio of 1. Currently, there are no valiresults from gallbladder distention after acute and usually trandated prophylactic measures. Symptoms such as dyspepsia, hearton medical history, clinical findings, and imaging. Alternative causes of upper abdominal pain should be conadditional information but is not necessary to make the diagnosis sidered in the differential diagnosis of biliary pain. Based on evidence from only one for the need of cholecystectomy at 24 and 48 h follow-up [289]. However, no correlation between the severity an open procedure and prolong hospital stay after cholecystecof symptoms, gallbladder description, or positive gallbladder tomy. Depending on additional risk factors between asymptomatic gallbladder stones (very low quality 67 and 769 cholecystectomies have to be performed to prevent a evidence; weak recommendation) gallbladder tumor [313]. The annual incidence of complications such as acute weak recommendation) cholecystitis, acute pancreatitis, obstructive jaundice, or cholangitis is 0. Furthermore, costs are lower for patients with asymptomatic gallstones if one waits until Cholecystectomy is not indicated in patients with symptoms or complications occur rather than prophylactic asymptomatic gallbladder stones and gallbladder polyps cholecystectomy or litholysis (see recommendation: Should fi5 mm (moderate quality evidence; strong recommendation) gallbladder stones be dissolved with bile acids taken orallyfi In several large studies polyps that were P1 cm in diameter had a clearly Exceptions increased probability of adenomas.
A unit of alcohol is equal to about half a pint of normal strength lager chronic gastritis h pylori buy metoclopramide mastercard, a small glass of wine or a pub measure (25ml) of spirits gastritis video buy discount metoclopramide 10mg. The most effective way to prevent gallstones is to eat a healthy gastritis symptoms during pregnancy cheap metoclopramide 10mg amex, low-fat diet that includes plenty of fresh fruit and vegetables (at least fve portions a day) gastritis and gastroparesis diet discount generic metoclopramide canada. Your diet should also include whole grains gastritis rash order metoclopramide overnight, which are found in wholemeal bread gastritis diet 2012 buy generic metoclopramide on line, brown rice and oats. Being overweight increases the amount of cholesterol in your bile and your chances of developing gallstones. Maintain a healthy weight by eating a balanced diet and taking plenty of regular exercise. Department of Anatomy, Ebonyi, the study was carried out to evaluate the gallbladder dimension in healthy adults of Abakaliki Area of Ebonyi State University, A 343, Abakaliki, State, South-Eastern Nigeria. Sixty healthy adult volunteers, consisting of thirty one (31) males and t wenty Nigeria nine (29) females were assessed by ultrasound following an overnight fast. Gallbladder Length, Width, Height, Wall Thickness and anthropometric variables (Body Height and Weight) were measured for each subject. Keywords: Ultrasonography, Gallbladder volume, Gallbladder wall thickness, Gallbladder length, Abakaliki. It functions in the storage and concentration of bile which is later released into the duodenum during the digestion of fatty substances[1][2]. The Fundus is a rounded end that faces the front of the body while the body [3] is in contact with the liver lying in a depression at the bottom of the liver. The cystic ducts unite with the common hepatic duct to become the common bile duct. The size of the normal adult gallbladder is approximately 8cm long and 4cm in diameter when fully distended[4]. It has capacity of about 50ml and varies in shape and size between the fasting and post prandial states. The gallbladder wall thickness is influenced by the degree of distension of the organ[5]. Alteration in the size of gallbladder is therefore likely to be indicative of health complications in the individual. Therefore, the assessment of normal size of the organ in a healthy individual is paramount in checking the health complications associated with the organ. However, ultrasonography is the modality of choice because it is cheap, non-invasive and reproducible and, does not utilize ionizing radiation[6][7]. Consequently, the technique of ultrasound has rapidly evolved, leading to its wide spread use in almost all fields of medical practice. Ultrasonography provides information about gallbladder size, gallbladder volume and gallbladder wall thickness. Traditionally, ultrasound is used as the initial imaging technique for evaluating patients with suspected gallbladder disease because of its high specificity and sensitivity in the detection of gallbladder dimensions, real-time character, speed and portability[8][9]. Also, it is paramount in identifying gallbladder pathologies like distension, contraction, sludge, stones and tumors[5]. Correspondence: the present study tries to evaluate the normal mean gallbladder dimensions of healthy adult subjects in Dr. Department of Anatomy, Ebonyi, the Abakaliki Area of Ebonyi State, South-Eastern Nigeria. This is clinically important in monitoring the State University, A 343, Abakaliki, health status of the individuals considering the notable variation in gallbladder size/volume in certain Nigeria disease conditions which could predispose the individual to stone formation, especially in those with 96 larger fasting gallbladder volume[10]. The data for this study was collected from 60 apparently healthy and physically active volunteers, comprising 31 males and 29 females. They the body height (Ht) in meters (m) was measured with a Metre-Rule were students and staff of Ebonyi State University, Abakaliki in the while the subject was standing barefooted in normal straight posture South-Eastern Nigeria. The body weight (Wt) in Kg was measured using a Weighing Balance while the subject was standing on the Weighing the gallbladder dimensions were assessed using Digital Real Time Balance barefooted with no object in the pocket. All statistical analyses were carried out in Life Scan Ultrasound Centre, Felix Memorial Hospital, Abakaliki, Microsoft Excel data base using Statistical Package for Social Science Ebonyi State. The mean values of the gallbladder parameters are as follows: under their heads to widen intercostal spaces. Table 1: Descriptive statistics of anthropometric parameters and gallbladder dimension Parameters Minimum Maximum Mean Std. Table 2: Descriptive statistics of anthropometric parameters and gallbladder dimension by age Parameters 18-23 24-29 30-35 36-41 PValue N= 34 N= 13 N= 7 N= 6 Weight(kg) 62. Table 2: Descriptive statistics of anthropometric parameters and gallbladder dimension by age Parameters Male Female T Df p-value N =31 N = 29 Age (yrs) 26. This may be suggestive of a significant variation in a large spectrum of pathological conditions. Moreover, Caroli-Bosc et al[9] reported that age correlated with significantly higher compared to their female counterparts. This could be attributed to ageing which leads to replacement of was also reported by Caroli-Bosc et al[9]. This fact could also be Pathophysiological significance of gallbladder volume changes in gallstone diseases. Sonographic measurement of fasting gallbladder volume in healthy adults in North-West, Nigeria. Gallbladder this study has successfully established the mean values of gallbladder contents and fasting gallbladder volumes during and after pregnancy, dimensions in healthy young adults of southeastern Nigeria. Sonographic gallbladder wall thickness in normal adult significant difference in the gallbladder dimensions with respect to population in Nigeria. Ultrasound quantification of gallbladder volume to establish baseline contraction indices in healthy adults: A pilot and reference reasons. Chicago: Year Hospital, Abakaliki, Ebonyi State and all the students and staff of Book Medical Publishers. Palasciano G, Serio G, Portincasa P, Palmieri V, Fanelli M, Velardi A, et and Superficial Structures. Gallbladder volume in adults and its relationship to age, sex, body mass index, body surface area and gallstones. Sonographic evaluation of gallbladder dimensions in healthy adults in Benin City, Nigeria. Ultrasonographic Assessment of the Fasting Gallbladder Volume in Healthy Adults in Calabar; Correlation with Body Weight Journal of Dental and Medical Sciences. Purpose and scope this guideline summarises the evidence for the fetal risks associated with obstetric cholestasis and provides guidance on the different management choices and the options available for its treatment. The wide range of definitions of obstetric cholestasis and the absence of agreed diagnostic criteria make comparisons of the published literature challenging and limit the ability to provide detailed recommendations for specific aspects of care. Areas of uncertainty are highlighted along with recommendations for future research in this field. Background In England,obstetric cholestasis (also referred to as intrahepatic cholestasis of pregnancy) affects 0. The clinical importance of obstetric cholestasis lies in the potential fetal risks, which may include spontaneous preterm birth,iatrogenic preterm birth and fetal death. There can also be maternal morbidity in association with the intense pruritus and consequent sleep deprivation. Selection of articles for analysis and review was then made based on relevance to the objectives. The National Library for Health and the National Guidelines Clearing House were also searched for relevant guidelines and reviews. Pruritus that involves the palms and soles of the feet is particularly suggestive. C Pruritus in pregnancy is common, affecting 23% of pregnancies, of which a small proportion will have obstetric cholestasis. The skin should be inspected and care must be taken to differentiate dermatographia artefacta (skin trauma from intense scratching),which may be seen in obstetric cholestasis,from other common skin conditions such as eczema or atopic eruption of pregnancy (previously referred to as eczema of pregnancy, prurigo and pruritic folliculitis). Other evidence of cholestasis should be sought, including pale stool, dark urine and jaundice, and other risk factors identified such as a personal or family history of obstetric cholestasis, multiple pregnancy, carriage of hepatitis C and presence of gallstones. In clinical practice, otherwise unexplained abnormalities in transaminases, gamma-glutamyl transferase and/or bile salts are considered sufficient to support the diagnosis of obstetric cholestasis. The increase in alkaline phosphatase in pregnancy is usually placental in origin and so does not normally reflect liver disease. For transaminases,gamma-glutamyl transferase and bilirubin, the upper limit of normal throughout pregnancy is 20% lower than the non-pregnant range. This may include carrying out a viral screen for hepatitis A, B, and C, Epstein Barr and cytomegalovirus, a liver autoimmune screen for chronic active hepatitis and primary biliary cirrhosis (for example,anti-smooth muscle and antimitochondrial antibodies) and liver ultrasound. D Typically,transaminases will range from just above the upper limit of normal to several hundreds. Postnatal resolution of symptoms and of biochemical abnormalities is required to secure the diagnosis. What is the risk of stillbirth for pregnancies complicated by obstetric cholestasisfi In a hospital setting, the current additional risk of stillbirth in obstetric cholestasis B above that of the general population has not been determined but is likely to be small. Stillbirth is the major concern for those involved in the management of obstetric cholestasis. Perinatal mortality of six deaths from 56 cases (107/1000) was described from a singleAustralian centre between 1965 and 1974. The contributions of active management,case selection (it is possible that more recent series include less severe cases) and reporting bias are unknown. These rates are comparable to whole population figures over the same time period: for England and Wales in 1980, the perinatal mortality rate was 13. What additional risks are associated with pregnancies complicated by obstetric cholestasisfi Obstetricians should be aware (and should advise women) that the incidence of B premature birth, especially iatrogenic, is increased. Women should be advised of the increased likelihood of meconium passage in B pregnancies affected by obstetric cholestasis. Obstetric cholestasis has been linked with an increased incidence of passage of meconium, premature delivery, fetal distress, delivery by caesarean section and postpartum haemorrhage. All studies, except the earliest two,12,14 practised some form of active surveillance and/or elective early delivery, so outcomes are a reflection of both the disease process and its management. No studies stated how pregnancy was dated, so gestational age may not have been accurately assessed. It is difficult to establish the relative roles played of obstetric cholestasis itself, of induction of labour/other obstetric indications and of obstetrician/patient anxiety. Despite physiological reasons (see section 9) and a high caesarean section rate, which might suggest an increased risk of postpartum haemorrhage,evidence from current practice does not show this. Postpartum haemorrhage is reported in only five case series, with rates ranging from 2% to 22%. Poor outcome cannot currently be predicted by biochemical results and delivery B decisions should not be based on results alone. No specific method of antenatal fetal monitoring for the prediction of fetal death can D be recommended. Ultrasound and cardiotocography are not reliable methods for preventing fetal death C in obstetric cholestasis. There is some evidence, mainly from in vitro work, that bile salts may play a role in fetal demise. The management of the cases of obstetric cholestasis analysed was at the discretion of the attending obstetrician,not subject to a uniform protocol and not revealed. There remained one stillbirth in a twin pregnancy with bile acid levels of 27 micromoles/litre. The authors in subsequent correspondence attribute this to a true Evidence knot in the umbilical cord. There were two stillbirths in the group with bile acids over 40 level 2+ micromoles/litre (one of a twin and one of a singleton). In a later paper by the same authors describing an intervention arm of the study, there was a stillbirth in a woman with obstetric cholestasis receiving placebo and with bile acids of 16 micromoles/litre. Other studies applying such cut-off values retrospectively have not shown differences in adverse obstetric outcomes. It may be that rates of fetal death are too low for a robust assessment of the relationship of this complication with bile acid levels. There are currently insufficient data available to inform decisions about the best intervention to prevent fetal death, but a relationship with bile acid levels is suspected and remains the focus of much research. There are also conflicting data relating to prediction of fetal death and liver enzyme concentrations,with one study reporting more fetal distress with high alanine aminotransferase35 and another showing no correlation.
Syndromes
- Transfusion reaction
- Large amounts of urine leaking around the catheter
- The American Association of Diabetes Educators
- Do not eat undercooked meat.
- Blood potassium level
- Cluster headache
- Abdominal aortic aneurysm
- Vomiting
- Excessive bleeding
- Strips of bone graft material may be placed over the back part of the spine.
Like other forms of dystonia gastritis diet 50 buy metoclopramide us, blepharospasm may be relieved by sensory tricks (geste antagoniste) gastritis y gases buy generic metoclopramide pills, such as talking gastritis diet 13 order metoclopramide 10mg on line, yawning gastritis kronik adalah cheap metoclopramide 10 mg with amex, singing gastritis diet pregnancy 10mg metoclopramide with amex, humming gastritis or gerd purchase cheap metoclopramide, or touching the eyelid. Blepharospasm may be aggravated by reading, watching television, and exposure to wind or bright light. Blepharospasm is usually idiopathic but may be associated with lesions (usually infarction) of the rostral brainstem, diencephalon, and striatum; it has been occasionally reported with thalamic lesions. The pathophysiological mechanisms underlying blepharospasm are not understood, but may refiect dopaminergic pathway disruption causing disinhibition of brainstem refiexes. Local injections of botulinum toxin into orbicularis oculi are the treatment of choice, the majority of patients deriving benefit and requesting further injection. Failure to respond to botulinum toxin may be due to concurrent eyelid apraxia or dopaminergic therapy with levodopa. Minor enlargement of the blind spot is difficult to identify clinically, formal perimetry is needed in this situation. Enlargement of the blind spot (peripapillary scotoma) is observed with raised intracranial pressure causing papilloedema: this may be helpful in differentiating papilloedema from other causes of disc swelling such as optic neuritis, in which a central scotoma is the most common field defect. Enlargement of the blind spot may also be a feature of peripapillary retinal disorders including big blind spot syndrome. In contrast, blink rate is normal in multiple system atrophy and dopa-responsive dystonia, and increased in schizophrenia and postencephalitic parkinsonism. These disparate observations are not easily reconciled with the suggestion that blinking might be a marker of central dopaminergic activity. In patients with impaired consciousness, the presence of involuntary blinking implies an intact pontine reticular formation; absence suggests structural or metabolic dysfunction of the reticular formation. Care should be taken to avoid generating air currents with the hand movement as this may stimulate the corneal refiex which may simulate the visuopalpebral refiex. It is probable that this refiex requires cortical processing: it is lost in persistent vegetative states. It has been reported that in the evaluation of sensory neuronopathy the finding of an abnormal blink refiex favours a non-paraneoplastic aetiology, since the blink refiex is normal in paraneoplastic sensory neuronopathies. These signs may help to distinguish tardive dyskinesia from chorea, although periodic protrusion of the tongue (fiycatcher, trombone tongue) is common to both. The pouting quality of the mouth, unlike that seen with other types of bilateral (neurogenic) facial weakness, has been likened to the face of the tapir (Tapirus sp. Cross Reference Facial paresis Bovine Cough A bovine cough lacks the explosive character of a normal voluntary cough. It may result from injury to the distal part of the vagus nerve, particularly the recurrent laryngeal branches which innervate all the muscles of the larynx (with the exception of cricothyroid) with resultant vocal cord paresis. Because of its longer intrathoracic course, the left recurrent laryngeal nerve is more often involved. A bovine cough may be heard in patients with tumours of the upper lobes of the lung (Pancoast tumour) due to recurrent laryngeal nerve palsy. Cross References Bulbar palsy; Diplophonia; Signe de rideau Bradykinesia Bradykinesia is a slowness in the initiation and performance of voluntary movements in the absence of weakness and is one of the typical signs of parkinsonian syndromes, in which situation it is often accompanied by difficulty in the initiation of movement (akinesia, hypokinesia) and reduced amplitude of movement (hypometria) which may increase with rapid repetitive movements (fatigue). It may be overcome by refiexive movements or in moments of intense emotion (kinesis paradoxica). Bradykinesia in parkinsonian syndromes refiects dopamine depletion in the basal ganglia. It may be improved by levodopa and dopaminergic agonists, less so by anticholinergic agents. There is a mild and transient aphasia or anomia which may share some of the characteristics of aphemia/phonetic disintegration. More commonly there is infarction in the perisylvian region affecting the insula and operculum (Brodmann areas 44 and 45), which may include underlying white matter and the basal ganglia (territory of the superior branch of the middle cerebral artery). Passive fiexion of the neck to bring the head onto the chest is accompanied by fiexion of the thighs and legs. Cross References Blepharospasm; Dystonia Bruit Bruits arise from turbulent blood fiow causing arterial wall vibrations which are audible at the body surface with the unassisted ear or with a stethoscope (diaphragm rather than bell, better for detecting higher frequency sounds). They are associated with stenotic vessels or with fistulae where there is arteriovenous shunting of blood. Examination for carotid bruits in asymptomatic individuals is probably best avoided, other than in the clinical trial 67 B Brushfield Spots setting, since the optimal management of asymptomatic carotid artery stenosis has yet to be fully defined. Dysfunction of efferent and/or afferent thalamic and striatopallidal tracts has been suggested as the neural substrate. If necessary, a rubber gum shield or bite may be worn in the mouth to protect the teeth. This may be differentiated clinically from bulbar weakness of upper motor neurone origin (pseudobulbar palsy). A myogenic bulbar palsy may be seen in oculopharyngeal muscular dystrophy, inclusion body myositis, and polymyositis. Cross References Cauda equina syndrome; Refiexes Buphthalmos Buphthalmos, literally ox-eye, consists of a large and bulging eye caused by raised intraocular pressure due to congenital or secondary glaucoma. Cross Reference Diamond on quadriceps sign Calf Hypertrophy Calf enlargement has many causes; it may refiect true hypertrophy (enlargement of muscle fibres) or, more commonly, pseudohypertrophy, due to infiltration with tissue elements other than muscle. Calf (and other muscle) hypertrophy is also a feature of limb girdle muscular dystrophy type 2I. Head fiexion to 30fi above the horizontal allows maximum stimulation of the horizontal semicircular canals, whereas 60fi below horizontal maximally stimulates the lateral semicircular canals. Induced nystagmus is then timed both with and without visual fixation (in the dark, Frenzel glasses). Normally, the eyes show conjugate deviation towards the ear irrigated with cold water, with corrective nystagmus in the opposite direction; with warm water the opposite pattern is seen. A reduced duration of induced nystagmus is seen with canal paresis; enhancement of the nystagmus with removal of visual fixation suggests this is peripheral in origin (labyrinthine, vestibulocochlear nerve), whereas no enhancement suggests a central lesion. As coma deepens even the caloric refiexes are lost as brainstem involvement progresses. A distinction is sometimes drawn between camptodactyly and streblodactyly: in the latter, several fingers are affected by fiexion contractures (streblo = twisted, crooked), but it is not clear whether the two conditions overlap or are separate. The term streblomicrodactyly has sometimes been used to designate isolated crooked little fingers. Camptodactyly may occur as part of a developmental disorder with other dysmorphic features or in isolation. Awareness of the condition is important to avoid unnecessary neurological investigation. Initially described in patients with psychiatric disorders, it may also occur in traumatic, metabolic, and neurodegenerative disorders. Neurologists have encompassed this phenomenon under the term reduplicative paramnesia. Capgras syndrome may be envisaged as a Geschwindian disconnection syndrome, in which the visual recognition system is disconnected from the limbic system, hence faces can be recognized but no emotional significance ascribed to them. Clearly, this term is cognate with or overlaps with waxy fiexibility which is a feature of catatonic syndromes. Catalepsy should not be confused with the term cataplexy, a syndrome in which muscle tone is transiently lost. Cross Reference Cataplexy; Catatonia Cataplexy Cataplexy is a sudden loss of limb tone which may lead to falls (drop attacks) without loss of consciousness, usually lasting less than 1 min. Attacks may be precipitated by strong emotion (laughter, anger, embarrassment, surprise). Sagging of the jaw and face may occur, as may twitching around the face or eyelids. During an attack there is electrical silence in antigravity muscles, which are consequently hypotonic, and transient arefiexia. Rarely status cataplecticus may develop, particularly after withdrawal of tricyclic antidepressant medication. Therapeutic options for cataplexy include tricyclic antidepressants such as protriptyline, imipramine, and clomipramine; serotonin-reuptake inhibitors such as fiuoxetine; and noradrenaline and serotonin-reuptake inhibitors such as venlafaxine.
Order metoclopramide 10mg with amex. Good Habits For Gastritis Patients.