Michael Y. Wang, MD, FACS
- Associate Professor
- Departments of Neurological Surgery and Rehabilitation Medicine
- University of Miami Miller School of Medicine
- Miami, Florida
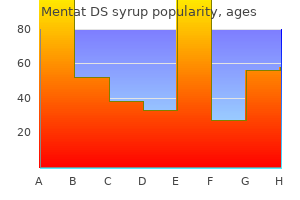
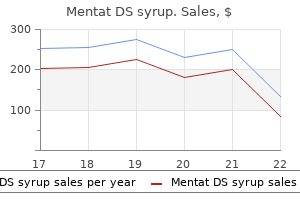
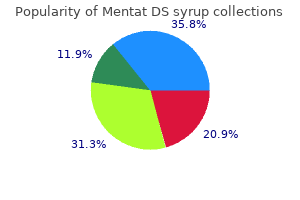
Since most patients have both Candida and erythrasma medicine emblem buy mentat ds syrup 100ml online, it may worsen if only one condition is treated counterfeit medications 60 minutes cheap mentat ds syrup 100 ml fast delivery. The duration of therapy varies treatment tendonitis buy mentat ds syrup 100ml fast delivery, but 2 weeks is usually sufficient for topical fucidin and erythromycin treatment 8mm kidney stone order mentat ds syrup master card. In these cases medications zanaflex 100 ml mentat ds syrup otc, the usual approach adopted is to give long-term antiseptic soaps medications related to the integumentary system discount 100ml mentat ds syrup fast delivery, such as povidone-iodine and to use drying agents, such as powders, in the affected areas. Superficial fungal infection of the skin Superficial fungal infections of the skin are one of the most common dermatologic conditions seen in clinical practice. However, making the correct diagnosis can be difficult, because these infections can have an atypical presentation or be confused with similar-appearing conditions. Superficial fungal infections can be divided into three broad categories: dermatophytic infections, Pityriasis versicolor and cutaneous candidasis 3. Dermatophytes Specifically Trichophyton, Epidermophyton and Microsporum species, are responsible for most superficial fungal infections. Dividing infections into the body region most often affected can help in identification of the problem. Tinea Capitis Tinea capitis is a dermatophytic infection of the head and scalp, usually found in infants, children, and young adolescents. Around puberty, sebum production by sebaceous glands becomes active, and as a result, it tends to disappear. Commonest presentation is scaly patches on the scalp with variable degree of hair loss and generalized scaling that resembles seborrhic dermatitis may occur on the scalp. An unusual scaling reaction known as favus may give the scalp a waxy or doughy appearance with thick crusted areas. Griseofulvin in a dose of 10-20 mg per kg for six weeks to 8weeks is the first-line treatment of Tinea capitis. Ketoconazole 2-4mg per kg for ten days, itraconazole and terbinafine (Lamisil) are good alternatives. Topical treatment can be added to decrease the transmission and accelerate resolution. Tinea corporis Tinea corporis is dermatophytosis of the glabrous skin of the trunk and extremities. Lesions are round, scaly patches that have a well defined, enlarging border and a relatively clear central portion. Itching is variable and not diagnostic Tinea corporis can assume a giant size (Tinea incognito) when steroids are applied for cosmetic reasons or as a result of miss diagnosis. Tinea pedis Tinea pedis is fungal infection of the feet and is usually related to sweating and warmth, and use of occlusive footwear. It may also present with a classic pattern on the dorsal surface of the foot or as chronic dry, scaly hyperkeratosis of the soles and heels. Treatment Topical anti fungal creams or ointments applied regularly for 4 6 wks. Once-weekly dosing with fluconazole is another option, especially in noncompliant patients. Tinea versicolor (Pityriasis versicolor) Versicolor versicolor is a common, benign, superficial cutaneous (stratum corneum) fungal infection at the level of stratum corneum characterized by hypo pigmented or hyperpigmented macules and patches with faint scale on the chest and the back. Etiology: Malassezia furfur (Pityrosporon ovale,) M furfur is a member of normal flora of the skin found in 18% of infants and 90-100% of adults. Predisposing factors include genetic predisposition, warm, humid environments, excessive sweating, immunosuppression, malnutrition, and Cushing disease. Treatment Patients should be informed that it is caused by a normal flora of the skin hence it is not transmitted and any skin color alterations resolve within 1-2 months after treatment. Effective topical agents include: Sodium thiosulphate solution, selenium sulfide and azole, ciclopiroxolamine, and allylamine antifungals. Weekly applications of any of the topical agents for the following few months may help prevent recurrence. Systemic treatment is also effective and is often preferred by patients because of convenience. Ketoconazole 200-mg daily for 10-days and as a single-dose 400-mg treatment, have comparative results. Oral therapy does not prevent the high rate of recurrence, unless repeated on an intermittent basis throughout the year. Candidiasis Candida infections caused by yeast-like fungi Candida albicans commonly occur in moist, flexural sites. Under certain conditions, they can become so numerous that they cause infections, particularly in warm and moist areas. Pruritic rash that begins with vesiculopustules, which enlarge and rupture, causing maceration and fissuring. Satellite lesions frequently are found that may coalesce and extend into larger lesions. Paronychia and onychomycosis Frequently, paronychia and onychomycosis are associated with immersion of the hands in water. Patients present with a painful and erythematous area around and underneath the nail and nail bed, warm, glistening, tense, and tender. There is secondary nail thickening, ridging, discoloration, and occasional nail loss in chronic cases. Physical examination reveals a diffuse erythema and white patches that appear on the surfaces of the buccal mucosa, throat, tongue, and gums. The presence of retrosternal pain, epigastric pain, nausea, and vomiting may suggest esophageal candidiasis Vulvovaginal candidiasis: this is the second most common cause of vaginitis. A patch resembling thrush appears on the glans and may spread to the thighs, gluteal folds, buttocks, and scrotum. Treatment Candida intertrigo Topical azoles and polyenes, including clotrimazole, miconazole, and nystatin, are effective. Paronychia the most important intervention is drainage followed by oral antifungal therapy with either ketoconazole, fluconazole or itraconazole. Single daily dose of itraconazole taken for 3-6 months or a pulsed-dose regimen that requires a slightly higher dose daily for 7 days, followed by 3 weeks off therapy. Warts Warts or verrucae are benign growths on the skin or mucous membranes that cause cosmetic problems as well as pain and discomfort. They are seen on people of all ages but most commonly appear in children and teenagers. The incubation period of a wart is 2 to 9 months during which time an excessive proliferation of skin growth slowly develops. In immunodeficiency states warts can become fulminantly wide spread and difficult to treat. Management is based on the age of the individual as well as the size, number, and location of warts. Common warts, especially in children, do not necessarily need to be treated, because they exhibit a high rate of spontaneous remission. Treatment fi Salicylic acid 25% ointment twice daily followed by cutting or scraping fi Preparation of salicylic acid 5-20% and lactic acid 5-20 in collodion are easier to use fi Electrodessication and curettage fi Freezing with liquid nitrogen if available. Protect the skin around the wart with Vaseline apply the podophyllin with a match stick carefully on the top of the war and wash after 6 hours. Molluscum contagiosum Molluscum contagiosum is a viral infection of the skin that causes discrete papules that may be mistaken for warts. Etiologic agent: Pox virus It is common in children and some time in immunocompromised adults. The rash of molluscum contagiosum is characterized by discrete, 2 to 5 mm papules that are fleshcolored (skin color) and dome-shaped with a central umbilication (depressed centre). In adults it appears in the pubic and genital region it is a sexually transmitted infection. Molluscum contagiosum is a self-limited disease, meaning it will eventually go away on its own. Each lesion generally lasts for about 6 to 9 months, but they can last for several years. Cryosurgery Using liquid nitrogen to freeze the lesion Salicylic Acid (Compound W) A solution applied to the lesion with or without tape occlusion 3. Pathogenesis of herpes simplex virus 30 Primary infection Latency Transmission can occur in all stages; more at the primary Reactivation stage What causes latencyfi Manifestations: Grouped blisters on erythematous base on the lips, cheeks, eyelids, intraoral. Zinc oxide paste, zinc oxide ointment or zinc oxide and topical antiseptic or antibiotic. Herpetic Whithlow Infection of pulp of fingertips, it could appear after touching a primary lesion of ones owns lesion or that of others. Lesions are bilateral and symmetrical, inguinal lymph nodes may be enlarged, fever and flu like symptom may be there. Manifestations: Skin vesicles, Encephalitis, Hepatitis, Pneumonia, Coagulopathy Mortality rate (M/R) >50% in ideal setting. Scabies Definition: scabies is one of the commonest intensely pruritic, highly contagious infectious conditions of the skin caused by a mite Sarcoptis scabei and transmitted by close personal and sexual contacts 34 Historically It has been recognized as a disease for over 2500 years. In 1687 Francesco Redi identified Sarcoptes scabei Scabies is one of the first diseases with a known cause. Romans used the term to describe any pruritic skin disease; so, it has been known as the great imitator Etiologic agent Sarcoptes scabei var. Epidemiology 9 Commoner in children and adolescents 9 It is a disease of disadvantaged community 9 Epidemic occurs during wars and social upheavals 9 Endemic in many developing countries Transmission Pathogenesis Female and male make mating on the surface of the skin. The male mite dies and the gravid female mite burrows into the epidermis lays up to 3 eggs per day for the duration of her 30-60 day lifetime. It starts on the wrist, finger webs and on the medial sides of fingers, the flexor aspect of 35 the wrist, the elbows and the anterior axillary folds, the genitalia and inner thighs and the gluteal folds More disseminated presentation in infants and toddlers. Scabies in infants and young children 9 Distribution and morphology:generalized 9 the face the scalp, palms an soles are affected 9 Papules, vesicle and pustules 9 Secondary eczematization and impetiginazation are common Crusted (Norwegian) scabies In 1848, Danielssen and Boeck described a highly contagious variant of scabies occurring in immunocompromised patients, elderly or mentally incompetent patients. Thousands to million mites are found instead of the normal 8-11 mites in the normal host. In Norwegian scabies, pruritus may not be there (in about 50% of the cases do not itch) It is psoriasiform and generalized with nail changes and scalp involvement Skin becomes thickened and involves all part of skin including face, palms and sales. Diagnosis of scabies o Itching, worse at night o Presence of similar condition in the family or intimate contacts o Characteristic distribution of lesions o Demonstration of the mite, eggs or feces o Therapeutic test Management o Treat with a scabicide agent o All family members and close contacts should receive treatment at the same time o Provide antihistamines to alleviate pruritus. Complications of scabies Bacterial super infection Eczematization Nodule formation Urticaria Treatment of complications: Use antibiotic and anti histamine. Causes of therapeutic failure Improper counseling Poor compliance of patient 37 Inadequate application Improper application Not treating family members who have close contacts 3. Eczemas Eczemas are groups inflammatory skin conditions manifesting either as acute eczematous lesions, which are characterized by active papules; erythema, excoriations and oozing (weeping), sub acute eczemas, also have excoriation, erythema with papules and scales or as a chronic eczematous lesion, characterized by thickening of the skin, and accentuation of the creases (lichenification) and hyperpigmentations 3. The hereditary tendency to develop allergies to food and inhalant substances as manifested by eczema, asthma and hay (allergic conjunctivitis and allergic rhinitis) fever is called atopy. It is the interaction of genetics and environmental factors that results atopic eczema. More than fi of the offsprings of atopic mother develop atopic dermatitis in the first 3 months of life. If one parent is atopic, more than 50% of the children would develop allergic symptoms by the age of two years and if both parents are affected, the chance of the child to have allergic symptoms would be about 79%. Diagnostic Criteria for Atopic Dermatitis the diagnosis of atopic eczema is made by constellation of criteria. Evidence of pruritus fi Three minor features are: fi Xerosis/ ichthiosis / hyperlinearity of palms and soles fi Perifollicular accentuation fi Post auricular fissure fi Chronic scalp scaling the hall mark of atopic eczema is pruritus and dryness of the skin. Long standing pruritus results in lichenified dry skin which would call for further scratching and in this way the itch scratch cycle establishes which assumes a vicious form. The flexures like the popilitial fossa, wrist, and anticubital fossa are affected. The pattern of distribution in atopic eczemas depends on the age and activity of the disease. Based on that atopic eczemas are classified in to: infantile eczema (from 2 39 months up to 2 years), childhood atopic eczema (from 2 years to 10 years) and atopic eczema of adolescents and adults. Infantile Atopic eczema Atopic dermatitis usually starts in the first year of life. During this phase, there is facial erythema, vesicles, oozing and crusting located mainly on the face, scalp, forehead and extensor surface of the extremities. Psychological effects often are very prominent Adolescent and adult atopic dermatitis: Flexural predilection of lesions persists. Localized, eczematous or lichenified plaques often predominates the clinical picture. Resolved cases show dryness and irritability of the skin with a tendency to itch with sweating and other triggers. Topical Steroids High potency steroids are used for a short period to rapidly reduce inflammation. Maintenance therapy, if needed is best done with mild steroids like hydrocortisone.
Environmental services medicine syringe discount 100 ml mentat ds syrup mastercard, infection prevention and control symptoms quitting tobacco buy discount mentat ds syrup 100ml on line, and occupational health and safety should be consulted as key stakeholders prior to the purchase of new electronic equipment that will be used in care areas new medicine purchase 100ml mentat ds syrup free shipping. Noncritical medical equipment used in the health care setting treatment for strep throat cheap 100 ml mentat ds syrup mastercard, including purchased treatment wrist tendonitis order mentat ds syrup visa, borrowed or donated equipment and equipment used for research purposes medications multiple sclerosis purchase online mentat ds syrup, shall be able to be cleaned and disinfected with a hospital disinfectant. Facilities must have item-specific instructions from manufacturers for cleaning and disinfecting all noncritical medical equipment, including purchased, borrowed or donated equipment and equipment used for research purposes. Disinfection is a process used on inanimate objects and surfaces to kill microorganisms. Cleaning products used in the health care setting: fi Must be approved by infection prevention and control, occupational health and safety, and environmental services. A hospital disinfectant is a kind of hard surface disinfectant that carries 140 efficacy claims against the bacteria Pseudomonas aeruginosa and Staphylococcus aureus. This will simplify the cleaning process, minimize the training requirements for environmental service workers, and reduce the potential for errors. This can be achieved by ensuring proper dilution of the disinfectant, frequently changing the disinfectant solution and wiping cloths, not dipping a soiled cloth into the 163 disinfectant solution. The pail holding the disinfectant solution had been used repeatedly for months without being emptied and dried between uses. This may be achieved using either a cloth and sufficient quantities of a disinfectant, or a large, pre-prepared (ready-to-use) wipes saturated with an appropriate disinfectant product. These cleaning 184 products can hold more water than conventional cleaning cloths (up to 6 times their weight). The use of microfibre and ultramicrofibre cleaning products can reduce the amount of water and cleaning disinfecting chemicals used and disposed in cleaning environmental surfaces and in reprocessing these cleaning products, resulting in lower cost and reduced exposure to disinfectant 184,188 chemicals, and less time spent in preparing and replenishing the cleaning solution. In addition, although microfibre and ultramicrofibre cleaning products claim to deliver superior cleaning with water only, the use of disinfectants can be helpful to destroy any bacteria spread by these products during cleaning. Although the cleaning efficacy of microfibre cleaning products used dry does not surpass that of 189 other commonly used cleaning materials, dusting with microfibre products may be better due to its 184 electrostatic properties. Must be approved by environmental services, infection prevention and control and occupational health and safety. Health care facilities should select a limited number of hospital disinfectants to minimize training requirements and the risk of error. These risks can be minimized by the correct and consistent use of good infection prevention and control practices, most importantly the use of Routine Practices (see below) at all times when in the care environment. The principle of Routine Practices is that all clients/patients/residents may carry harmful microorganisms regardless of their isolation status or diagnosis. Hand hygiene must be practised: fi Before initial patient/patient environment contact. Prolonged exposure to gloves increases 222,223 the risk of irritant contact dermatitis from sweat and moisture within the glove and the risk of tears. Environmental service workers must not walk from patient environment to patient environment and between patient and health care environment wearing the same pair of 32,58 7,226,227 gloves. Hand hygiene must be performed immediately before putting on gloves and immediately after gloves are 7,32,64,216,218,228 removed. Selection of gloves should be based on a risk analysis of the type of setting, the task that is to be performed, likelihood of exposure to body substances, length of use and amount of stress on the 218 glove. Gloves must be removed and hand hygiene performed upon leaving each client/patient/resident room or bed space. However, personal protective equipment requirements identified on safety data sheets shall be followed when using chemical agents. The specific type of Additional Precautions required is based on the method of transmission of the suspected infectious agent. The health care setting must ensure that environmental services has the human resources, 237 education and equipment required to perform effective cleaning. These recommendations and cleaning practices apply to all health care settings regardless of whether cleaning is conducted by in-house staff, or contracted out. They are designed to be used as a standard against which in-house services can be benchmarked, as the basis for specifications if cleaning services are contracted out, and as the framework for auditing of cleaning services by cleaning supervisors and managers. Contracts should support (without penalty or financial barrier) a proactive and cooperative environment to consistently implement appropriate cleaning measures. Staffing levels must be appropriate to each department of the health care facility, with the ability to increase staffing in the 242 event of outbreaks. Environmental service departments of Canadian acute care facilities are frequently under-resourced, potentially increasing the risk of health care-associated infections, 245-248 antibiotic-resistant organism transmission, and outbreaks. General staffing levels and human resource requirements may be estimated by determining the average time required for environmental service workers to adequately perform daily and terminal cleaning of client/patient/resident rooms. One survey of environmental service managers at 50 Canadian acute care hospitals identified that cleaning times varied significantly based on cleaning type. Adequate supervisory staffing levels will help ensure that these requirements are being met and, as increasingly complex auditing procedures are adopted, additional staffing may be required to ensure that audits are conducted and responded to appropriately (see 9. Conversely, facilities with high rates of environmentally associated health care-associated infections should review their environmental service program, and consider adopting strategies to increase the effectiveness of environmental cleaning, including increasing staffing levels where low staffing levels may be contributing to inadequate 15,16,69,74,85,159,254,256 cleaning and disinfection. Individual facilities will, therefore, need to consider all of these factors when determining staffing levels required for environmental services. Each health care setting is encouraged to perform their own time management studies to determine appropriate staffing levels for cleaning and supervisory staff, taking into consideration the factors discussed above. In some health care facilities, environmental service workers may be assigned other tasks. Levels of supervisory staff must be appropriate to the number of staff involved in cleaning and sufficient to ensure that a. A safe workplace is maintained at all times, and occupational health and infection prevention and control procedures are routinely followed, including the correct use of personal protective equipment. Clinical areas include but are not limited to areas where clients/patients/residents receive care but also include patient waiting areas, areas for storage of medical equipment and supplies, medication preparation areas, and other areas involved in the provision of health care. This includes public areas such as lobbies; offices; corridors; elevators and stairwells; and service areas. Areas designated as part of the hotel component are cleaned with a hotel clean regimen. Areas designated as part of the health care component are cleaned with a health care clean. The health care component of the health care setting should be the priority for environmental cleaning. Additional cleaning practices may be required for clients/patients/residents known or suspected to be colonized or infected with a specific organism (or clients/patients/residents with a specific clinical syndrome). Additional cleaning practices are often directed towards clients/residents/patient colonized or infected with organisms that can persist for a prolonged time within the care environment, and may be relatively resistant to standard disinfectants. Additional cleaning practices may also be required for microorganisms that pose an extreme risk to clients/ patients/residents, staff and visitors such as Ebola Virus Disease. In addition to the above, enhanced cleaning and disinfection is often required during outbreaks of organisms when environmental contamination and subsequent transmission is known to be related to the type of organism suspected of causing the outbreak. Additional cleaning in an outbreak generally depends on the microorganism causing the outbreak. While this contamination is concentrated in the vicinity of the client/patient/resident and the areas used by the client/patient/resident. Given the potential for surfaces and items to become contaminated with microorganisms, all areas, surfaces, and items within care areas of the health care setting require cleaning on a routine basis. Low-touch surfaces require cleaning on a regular basis, when soiling or spills occur, and when a client/patient/resident is discharged 92 from the health care setting. Areas can be considered lightly contaminated or not contaminated if surfaces are not exposed to blood or body fluids or items that have come in contact with blood or body fluids. As the activity or vulnerability of clients/patients/residents in an area changes, the risk score will change as well, impacting on the cleaning frequency. A system should be in place to clearly identify equipment which has been cleaned and disinfected. Regular education and support must be provided by health care organizations and contract agencies to help staff consistently implement safe and effective cleaning, infection prevention and 15-17,158,159,253,254,291-293 control, and occupational health and safety practices. Shall include: [Legislation] [modified 2018] fi the correct and consistent use of Routine Practices. Occupational Health and Safety Issues Related to Environmental Services Environmental service workers are exposed to occupational risks including exposure to infectious microorganisms from clients/patients/residents and the health care environment, exposure to the chemical agents used for cleaning, and ergonomic stressors related to the mechanics of cleaning that 147,222,297-303 may involve repeated pushing, pulling, lifting or twisting. Health care facilities shall ensure that these risks are minimized to protect their environmental service workers and allow them to 229 perform their work in an optimal and safe environment. Strategies should also be in place to reduce the risk of 219,220,229,296,304 injury due to ergonomic or other workplace hazards. Irritants in health care settings associated with skin symptoms (irritant contact dermatitis) include water, soaps and detergents, most frequently in those who have underlying atopic dermatitis (allergy, eczema). Caution should be taken when cleaning and disinfection is performed in small and/or poorly ventilated spaces to reduce the risk of irritation to exposed skin and respiratory tract, and to ensure that exposure limits are not exceeded. Products that are lighter in weight, easily emptied and having proper handle length help reduce the risk of injury. Additionally, a variety of handle lengths should be available to ensure that differently sized cleaning staff have access 222 to appropriate ergonomically designed equipment. A soiled utility room is used for temporary storage of supplies and equipment that will be removed for 80 341 cleaning, reprocessing or destruction, for the disposal of small amounts of liquid human waste, and 81 for rinsing and gross cleaning of medical instruments. Soiled utility rooms should: 80,81 fi Be physically separate from other areas, including clean supply/storage areas. A clean utility/supply room for storing sterile supplies and equipment should: 80,81 fi Be separate from and have no direct connection with soiled workrooms or soiled holding areas. When choosing a tool for cleaning toilets, consideration should be given to equipment that will minimize splashing. Infection prevention and control must assess construction and maintenance projects during planning, work, and after completion to verify that 31,86 infection prevention and control recommendations are followed throughout the process. Infection prevention and 31 control and occupational health and safety have the authority to halt projects if there is a safety risk. Cleaning is of particular importance both during construction and after completion of the construction project. The level of cleaning that is expected during construction and at commissioning must be stated in the contract and the responsibility for cleaning 86 both the job site and adjacent areas shall be clearly defined. Wet carpets, if present, must be dried completely within 48 hours as the risk of mould growth increases substantially 86 after that point. Food service areas cannot re-open until the flood is controlled, the area has been cleaned, disinfected, and approval for food preparation has been obtained from public health units. Includes overflow Remove and discard wet Heavily and from a toilet bowl containing faeces, broken carpet, drywall, furniture and grossly sewer line, backed up sewage, all forms of ground other porous materials. Shall be physically separate from other areas, including clean supply/storage areas. All health care settings must have a plan in place to deal with floods and water leaks. Any sharps found in linen shall be reported to management and documented to prevent future 304 incidents from happening. There must be policies and procedures to ensure that clean laundry is transported and stored in a manner that will ensure that cleanliness is maintained. To prevent spillage and to protect the safety of waste handlers, waste containers should 296 not be overfilled. Legislation dictates that biomedical waste be handled and disposed of in a manner that avoids 2,3,92,219,229,363 transmission of potential infections: fi Biomedical waste (excluding sharps waste) destined for incineration shall be placed in leak proof single use biomedical waste containers, which may be rigid plastic containers or cardboard 2 containers that are sealed and lined with a leak proof plastic bag that can be securely tied. Single-use containers should have a lid that cannot be removed after the container is sealed; re-usable containers should have a lid that is locked 2 when the container is full. Health care facilities shall have a contingency plan for dealing with the storage of refrigerated waste in 296 the event of: fi excess waste production fi the on-site cold storage unit or treatment equipment becoming inoperative fi other disruption of disposal services 7. If a dedicated elevator is not available, waste should not be transported at the same time as clients/patients/residents, food serving carts or clean/sterile instruments/supplies/linen. Shall be transported in leak-proof and covered carts which are cleaned on a regular basis. Additionally, one study using copper oxide impregnated linens 385 demonstrated a 24% reduction in health care-associated infection in a chronic care ward, and another study demonstrated a 44% reduction in health care-associated infection in the acute care setting among patients admitted to a room containing six copper items as compare to patients admitted to a room 380 24 with noncopper items. There is, therefore, insufficient evidence to recommend for or against the use of copper surfaces or copper impregnated linens in the health care setting, and facilities should weigh the cost, functionality, the limitation of copper (See Table 6) against its known antimicrobial properties, and low quality evidence suggesting it may impact infection rates when considering the use of copper surfaces or linens. No-touch disinfection systems are systems that use chemical disinfectants or physical agents to disinfect surfaces and which do not require that the active agent is directly applied to and removed from the surface manually. It is difficult to estimate the magnitude of this effect, as sampling methodology and microbiological outcomes measured varied widely between studies. In the five studies evaluating hydrogen peroxide vapour in the outbreak 405,409,410 setting, three used hydrogen peroxide vapour as a one-time treatment of an entire ward, two additional studies did the same thing but then continued using hydrogen peroxide vapour for discharge 402,411 cleaning of rooms occupied by patients with antibiotic-resistant organisms on an ongoing basis.
Incidence in healthy children generally is 10% to 40% each year symptoms narcolepsy cheap mentat ds syrup 100 ml without a prescription, but illness rates as low as 3% also have been reported symptoms 2dp5dt buy cheap mentat ds syrup online. Tens of thousands of children visit clinics and emergency departments because of infuenza illness each season medicine for diarrhea buy genuine mentat ds syrup. Infuenza and its complications have been reported to result in a 10% to 30% increase in the number of courses of antimicrobial agents prescribed to children during the infuenza season symptoms 7 days before period order mentat ds syrup on line amex. Hospitalization rates among children younger than 2 years of age are similar to hospitalization rates among people 65 years of age and older symptoms vaginal yeast infection discount 100ml mentat ds syrup overnight delivery. However symptoms 5dp5dt fet purchase 100 ml mentat ds syrup overnight delivery, children younger than 24 months of age consistently are at a substantially higher risk of hospitalization than older children. Antecedent infuenza infection sometimes is associated with development of pneumococcal or staphylococcal pneumonia in children. Methicillin-resistant staphylococcal community-acquired pneumonia, with a rapid clinical progression and a high fatality rate, has been reported in previously healthy children and adults with concomitant infuenza infection. Rates of hospitalization and morbidity attributable to complications, such as bronchitis and pneumonia, are even greater in children with high-risk conditions, including hemoglobinopathies, bronchopulmonary dysplasia, asthma, cystic fbrosis, malignancy, diabetes mellitus, chronic renal disease, and congenital heart disease. Infuenza virus infection in neonates also has been associated with considerable morbidity, including a sepsis-like syndrome, apnea, and lower respiratory tract disease. Fatal outcomes, including sudden death, have been reported in both chronically ill and previously healthy children. During the entire infuenza A (H1N1) pandemic period lasting from April 2009 to August 2010, a total of 344 laboratory-confrmed, infuenza-associated pediatric deaths were reported. Most pediatric deaths are attributable to infuenza A and occur in children younger than 5 years of age, and approximately 50% of children who died did not have a high-risk condition as defned by the Advisory Committee on Immunization Practices. A pandemic is defned by emergence and global spread of a new infuenza A virus subtype to which the population has little or no immunity and that spreads rapidly from person to person. Pandemics, therefore, can lead to substantially increased morbidity and mortality rates, compared with seasonal infuenza. During the 20th century, there were 3 infuenza pandemics, in 1918 (H1N1), 1957 (H2N2), and 1968 (H3N2). The pandemic in 1918 killed at least 20 million people in the United States and perhaps as many as 50 million people worldwide. The 2009 infuenza A (H1N1) pandemic was the frst in the 21st century, lasting from April 2009 to August 2010. Pediatric health care professionals should be familiar with national, state, and institutional pandemic plans, including recommendations for vaccine and antiviral drug use, health care surge capacity, and personal protective strategies that can be communicated to patients and families. Public health authorities have developed plans for pandemic preparedness and response to a pandemic in the United States. Specimens of nasopharyngeal secretions obtained by swab, aspirate, or wash should be placed in appropriate transport media for culture. After inoculation into eggs or cell culture, infuenza virus usually can be isolated within 2 to 6 days. Additionally, many rapid diagnostic antigen tests cannot distinguish between infuenza subtypes, a feature that can be critical during seasons with strains that differ in antiviral susceptibility and/or relative virulence. Results of immunofuorescent and rapid diagnostic tests should be interpreted in the context of clinical fndings and local community infuenza activity. Careful clinical judgment must be exercised, because the prevalence of circulating infuenza viruses infuences the positive and negative predictive values of these infuenza screening tests. False-positive results are more likely to occur during periods of low infuenza activity; false-negative results are more likely to occur during periods of peak infuenza activity. In the United States, 2 classes of antiviral medications currently are available for treatment or prophylaxis of infuenza infections: neuraminidase inhibitors (oseltamivir and zanamivir) and adamantanes (amantadine and rimantadine). Since 2005, all H3N2 strains in the United States have been resistant to adamantanes. Since January 2006, neuraminidase inhibitors (oseltamivir, zanamivir) have been the only recommended infuenza antiviral drugs because of this widespread resistance to the adamantanes and the activity of neuraminidase inhibitors against infuenza A and B viruses. However, the 2009 pandemic infuenza A (H1N1) virus, which subsequently replaced the previous infuenza A (H1N1) seasonal strain, largely is susceptible to neuraminidase inhibitors (oseltamivir and zanamivir) and resistant to adamantanes (amantadine and rimantadine). These resistance patterns among circulating infuenza A virus strains simplify antiviral treatment, as 2009 infuenza A (H1N1), infuenza A (H3N2), and infuenza B all were susceptible to neuraminidase inhibitors and resistant to adamantanes. Antiviral Drugs for Infuenzaa Prophylaxis Drug (Trade Treatment IndicaName) Virus Administration Indicationsb tionsb Adverse Effects Oseltamivir A and B Oral 1 y of age 1 y of age Nausea, vomiting (Tamifu) or older or older Zanamivir A and B Inhalation 7 y of age 5 y of age Bronchospasm (Relenza) or older or older Amantadinec A Oral 1 y of age 1 y of age Central nervous (Symmetrel) or older or older system, anxiety, gastrointestinal Rimantadinec A Oral 13 y of age 1 y of age Central nervous (Flumadine) or older or older system, anxiety, gastrointestinal a For current recommendations about treatment and chemoprophylaxis of infuenza, see Each year, options for treatment or chemoprophylaxis of infuenza in the United States will depend on infuenza strain resistance patterns. Therapy for infuenza virus infection should be offered to any child with presumed infuenza or severe, complicated or progressive illness, regardless of infuenza-immunization status and for infuenza infection of any severity in children with a condition that places them at increased risk. Treatment should be considered for any otherwise healthy child with infuenza infection for whom a decrease in duration of clinical symptoms is felt to be warranted by his or her health care professional, particularly if treatment can be initiated within 48 hours of illness onset. Children with severe infuenza should be evaluated carefully for possible coinfection with bacterial pathogens (eg, S aureus) that might require antimicrobial therapy. Clinicians who want to have infuenza isolates tested for susceptibility should contact their state health department. If antiviral therapy is prescribed, treatment should be started as soon after illness onset as possible and should not be delayed while waiting for a defnitive infuenza test result, because beneft is greatest when treatment is initiated within 48 hours of onset of symptoms. Treatment should be discontinued approximately 24 to 48 hours after symp-1 toms resolve. The duration of treatment studied was 5 days for both the neuraminidase inhibitors (oseltamivir and zanamivir) and the adamantanes (amantadine and rimantadine). Recommended dosages for drugs approved for treatment and prophylaxis of infuenza are provided in Table 4. Patients with any degree of renal insuffciency should be monitored for adverse events. Only zanamivir, which is administered by inhalation, does not require adjustment for people with severe renal insuffciency. Postmarketing reports, mostly from Japan, have noted self-injury and delirium with use of oseltamivir among pediatric patients, but other data suggest that these occurrences were related to infuenza disease itself rather than antiviral therapy. Nevertheless, cautioning parents and patients regarding abnormal behavior is advised. Zanamivir use has been associated with bronchospasm in some people and is not recommended for use in patients with underlying airway disease. Both amantadine and rimantadine, but especially amantadine, may cause agitation, which resolves with discontinuation of the drug. An increased incidence of seizures has been reported in children with epilepsy who receive amantadine and, to a lesser extent, rimantadine. Because of a lower incidence of adverse events, rimantadine generally is preferred over amantadine for both prophylaxis and treatment. Control of fever with acetaminophen or other appropriate antipyretic agents may be important in young children, because fever and other symptoms of infuenza could exacerbate underlying chronic conditions. Children and adolescents with infuenza should not receive aspirin or any salicylate-containing products because of the potential risk of developing Reye syndrome. Respiratory tract secretions should be considered infectious, and strict hand hygiene procedures should be used. Typically, 1 or more strains are changed each year in anti cipation of the predominant infuenza strains expected to circulate in the United States in the upcoming infuenza season. During the past 25 years, there have been only 4 times that the vaccine strains in the infuenza vaccine have not changed from the previous year. Febrile seizures were most common in children 12 through 23 months of age when the 2 vaccines were given during the same visit. In this group, approximately 1 additional febrile seizure occurred among every 2225 children immunized. Getting recommended childhood vaccines during a single visit has important benefts of protecting children against many infectious diseases; minimizing the number of visits that parents, caregivers, and children must make; and preventing febrile seizures by protecting children against infuenza and pneumococcal infections, both of which can cause fever. This method of delivery involves a microinjection with a needle 90% shorter than needles used for intramuscular administration. A high-dose infuenza vaccine is available for adults 65 years of age and older ( The 3 vaccine strains are attenuated, cold adapted, temperature sensitive viruses that replicate in the cooler temperature of the upper respiratory tract and stimulate both an IgA and IgG antibody response. Signifcant protection against disease is achieved 1 to 2 weeks after the second dose. In seasons in which vaccine strains do not change from the previous year, children 6 months through 8 years of age who received 1 vaccine dose the previous season need to receive only 1 dose in the current season. Recommendations for 2 doses of vaccine will resume for seasons when 1 or more of the vaccine strains change. The effcacy (ie, prevention of illness among vaccine recipients in controlled trials) and effectiveness (ie, prevention of illness in populations receiving vaccine) of infuenza vaccines depend primarily on the age and immunocompetence of vaccine recipients, the degree of similarity between the viruses in the vaccine and those in circulation, and the outcome being measured. The effectiveness of infuenza immunization on acute respiratory tract illness is less evident in pediatric than in adult populations because of the frequency of upper respiratory tract infections and infuenzalike illness caused by other viral agents in young children. Antibody titers for seasonal infuenza vaccines wane up to 50% of their original levels 6 to 12 months after immunization. After administration of a live vaccine, at least 4 weeks should pass before another live vaccine is administered. Physicians should refer to the product circular each year to ensure that the appropriate dosage is given. For infants and young children, the preferred site is the anterolateral aspect of the thigh. Infuenza immunization should begin in September or as soon as the vaccine becomes available and continue into March or for as long as vaccine is available. Some children 2 through 4 years of age have a history of wheezing with respiratory tract illnesses but have not been diagnosed with asthma. Consideration should be given to the potential risks and benefts of administering infuenza vaccine to any child with known or suspected immunodefciency. In children receiving immunosuppressive chemotherapy, infuenza immunization may result in a less robust response than in immunocompetent children. The optimal time to immunize children with malignant neoplasms who must undergo chemotherapy is more than 3 weeks after chemotherapy has been discontinued, when the peripheral granulocyte and lymphocyte counts are greater than 1000/fiL (1. Children with hemodynamically unstable cardiac disease constitute a large group potentially at high risk of complications of infuenza. Corticosteroids administered for brief periods or every other day seem to have a minimal effect on antibody response to infuenza vaccine. Prolonged administration of high doses of corticosteroids (ie, a dose of prednisone of either 2 mg/kg or greater or a total of 20 mg/day or greater or an equivalent) may impair antibody response. Infuenza immunization can be deferred temporarily during the time of receipt of high-dose corticosteroids, provided deferral does not compromise the likelihood of immunization before the start of infuenza season (see Vaccine Administration, p 20). Studies have shown that infants born to women who received infuenza vaccine have better infuenza-related health outcomes. However, data suggest that no more than half of pregnant women receive seasonal infuenza vaccine, even though both pregnant women and their infants are at higher risk of complications. In addition, there is limited evidence that infuenza immunization in pregnancy may decrease the risk of preterm birth. Immunization of people who are in close contact with children with high-risk conditions or with any child younger than 60 months (5 years) of age is an important means of protection for these children. In addition, immunization of pregnant women may beneft their unborn infants, because transplacentally acquired antibody and human milk may protect infants from infection with infuenza virus. Because 1 voluntary immunization programs have failed to raise coverage rates among health care personnel above an average of 40%, a mandate is necessary to achieve herd immunity, reach Healthy People 2020 objectives, and suffciently protect people who come in contact with health care personnel. Infuenza causes signifcant morbidity and mortality for both patients and health care personnel. A mandate is expected to cut costs and increase effciency in health care settings. There is growing support for a mandate among medical organizations, and hospitals that already have implemented mandatory infuenza immunization for health care personnel have had enormous success. The recommended time ranges from the beginning of September to the end of April and longer when vaccine is available and not expired. Infuenza vaccine administration throughout the entire season now is recommended, because the infuenza season extends into March and April. Immunization throughout the season may protect some people against late outbreaks of infuenza.
Buy mentat ds syrup overnight delivery. Pneumonia Symptoms Precautions Medicines and Treatment by Dr Aadil Chimthanawala.