W. Cary Mobley, BS Pharmacy, PhD
- Clinical Associate Professor
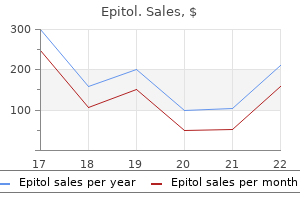
- College of Pharmacy
- University of Florida
He said medications used to treat fibromyalgia purchase epitol master card, Not least important nor least interesting in the history of these peripheral paralyses is their extension to a large part of the nervous system?one could speak of generalisation?to the point of compromising life through the invasion of the most essential nerves such as the vagus nerve [7] medicine x 2016 epitol 100mg fast delivery. It demonstrated the existence of peripheral paralysis medications errors buy discount epitol 100 mg on-line, with the possibility of extension to the nervous centres: for Dumenil medications 5113 cheap epitol 100 mg on line, they could be called chronic ascending neuritis medications 123 order cheap epitol. Even if some observations of similar patients appear by the end of the century medications known to cause miscarriage generic epitol 100mg free shipping, nothing new concerning clinical or pathological aspects was worthy of note until the description of Guillain, Barre and Strohl [8,9]. Neurology in Paris at the Turn of the Century After the death of Charcot in 1893, the main subject of discussion among neurologists remained what constituted the true nature of hysteria. Within this debate a turning point appeared with the studies of Joseph Babinski (1857?1932). Babinski had been a senior resident under Charcot, and his first conception was directly inspired by his master, but he progressively drew away from the Charcot school of thought, creating a new definition of hysteria (1901) and suggesting as a substitute the term pithiatism. After the death of Charcot, the chair for nervous diseases at the Salpetriere was held by Raymond (1844?1910), then by Jules Dejerine (1849?1917). Married to an American student, Dejerine would have an efficient teammate in his wife, especially on their masterpiece Anatomy of the central nervous system. Among their other numerous papers, 2 are eponymous: the description of the Dejerine-Roussy syndrome, caused by a lesion in the posterior thalamus, and Dejerine-Sottas neuropathy. He worked on aphasia, though his ideas were opposed to those of Paul Broca and Karl Wernicke. He started the Revue Neurologique in 1893 and the Societe de Neurologie, being its first general secretary. French Neurology during the First World War More than half of the members of the Societe de Neurologie served in the armed forces; some continued their activities in their department partially militarised, like Babinski and Froment at the Pitie Hospital or Dejerine and A. Besides a heavy traumatic pathology affecting the central nervous system and peripheral nerves, combat conditions and social attitudes during the war resulted in a considerable number of mental disorders. The distinction between emotional stress and psychic trauma directly related to fighting and simulation was a major concern for army physicians. The Societe de Neurologie and representatives of allied medical centres held a joint meeting in 1916. Many of the works from this meeting were published after the war, such as the book by Babinski and Froment, Hysteria and pithiatism and reflex nervous disorders in the neurology of war (1917) or Neurological works during war by Guillain and Barre (1920). It is remarkable that in such conditions, just after the Battle of the Somme, the 3 authors were able to publish a short note on 2 paralysed soldiers they encountered in 1916 [8]. Barre Georges Guillain classed first at the resident exam in 1898 and had the possibility of working among prestigious mentors in neurology, completing his residency with P. In this way he started with the study of cerebrospinal fluid (focusing on the benzoin colloidal reaction in nervous syphilis). Jean Alexandre Barre, a resident under Babinski in 1909?1910, defended his thesis on tabes arthropathies. He started a long collaboration with Guillain during the war and became his friend. While a professor of neurology in Strasbourg, beginning in 1919, Barre published several hundred papers. In 1925 he welcomed Joseph Babinski in Strasbourg with great warmth, ensuring a large audience for his conference on the importance of asking the right questions and in detecting subjective symptoms; he was responsible for the introduction of Guillain to Babinski. This relative reserve persisted until 1936 with a complete clarification at the Societe de Neurologie, following a paper by Theophile Alajouanine on a case of acute polyneuritis followed by death. This characteristic was for them absolutely different from infectious polyneuritis. They rejected the hypothesis of any similarity with the acute febrile neuritis recognised by Osler in 1892 and Holmes in 1917, due to the presence of fever in their syndrome. They admitted, however, with additional experience, to some modifications in the original description: cranial nerves may be involved and difficulty with micturition can occur. Furthermore, some clinical subdivisions may be described such as spinal, spinal and brain stem, brainstem, mental signs. The Unknown but Well-known Patient Harvey Cushing, along with many other American physicians, took part in the First World War. In August 1918, after an episode of flu, he suffered from an illness characterised by a progressive weakness of the legs with paraesthesia, then his hands, and lastly associated with bilateral facial paresis. Back in Boston in February 1919, he resumed his operative schedule, but remained exhausted after operations. The exact diagnosis of his illness was unknown and particularly difficult to establish due to an association with peripheral vascular disorder. This seems to be confirmed by the evolution: rapid deterioration, plateau phase and slow improvement albeit incomplete. Walusinski O (2013) Pioneering the concepts of Stereognosis and Polyradiculoneurits: Octave Landry (1826?1865). Guillain G (1936) Radiculoneuritis with acellular hyperalbuminosis of the cerebrospinal fluid. Haymaker W, Schiller F (1970) the Founders of Neurology, One Hundred and Forty-Six Biographical Sketches by Eighty-Nine Authors. Dumenil L (1866) Contributions pour servir a l?histoire des paralysies peripheriques et specialement de la nevrite. Babinski J, Froment J (1917) Hysterie-pithiatisme et troubles nerveux d?ordre reflexe en neurology de guerre. Generally left out in the cold thereafter, the 1977 obituary notice of Strohl refers to the syndrome of Guillain, Strohl and Barre. Also jostling for a place on the podium when speaking of acute ascending paralysis is the description in 1859 by Jean Baptiste Octave Landry (1826?1865) [2]?an omission partly corrected by Webb Haymaker (1902 1984) and James Kernohan (1911?1981) when reviewing their experience of the Landry-Guillain-Barre syndrome [3]. Thomas Willis entitled the last of his 12 treatises Pharmacutice rationalis (1674?1675), emphasising that treatment in medicine should be mechanism-based [6]. But that ideal presupposed a concept of disease and a system for nomenclature [7]. By the late 17th century, as far as the nervous system was concerned, not much had changed for over 2 millennia since the Greeks and Romans rationalized existing concepts. It was a short step to extend the concept of physiology (Francis Glisson, 1597?1677) to that of a pathological process that encapsulated primitive origins of the concept of immunology (Girolamo Frascatoro, 1478?1553). Although previous images had shown appendages attached to the brain and spinal cord, Andreas Vesalius (1514?1564) first accurately depicted the nervous system?brain, spinal cord and peripheral nerves?as one structure in his drawing of the nerves, which shows the origin of the 7 pairs of nerves that arise from the brain and the beginning of the spinal cord, and superbly explains the ordering and succession of all the pairs that take their origin from the spinal cord that is contained in the bones of the back. Thomas Sydenham (1624?1689) advanced the concept of natural history, detected by observation of untreated disease over time. There followed studies on the anatomical seat of disease (Giovanni Morgagni, 1682?1771); and the final transition to the notion of cellular (dis)organization as the basis of all pathology (Rudolph Virchow, 1821?1902). Thus, when Guillain, Barre and Strohl studied medicine, disease consisted of a pathological process affecting one or more parts of the body, with a natural history and a cellular basis for alterations in physiology underlying the characteristic symptoms and signs. But how best could one disease be distinguished from another, and appropriately named? As clinical descriptions proliferated, nomenclature switched from reference to the most obvious manifestations?the falling sickness, the sick headache, the scrofulous palsy?to hagiography and the medical eponym. Later, a mechanism-based taxonomy seemed preferable, and pathology started contributing to the classification of disease. Nonetheless, custodians of the eponym fought back, as the celebration of this book concedes. In the preface to Neurological Eponyms, Peter Koehler, George Bruyn (1928?2002) and John Pearce argue that medical eponyms are again in vogue, and the feeble attempt of would-be scientific doctors to emulate the real sciences of mathematics and physics has suffered a volte face in which the silent revolution of molecular biology in identifying mutations, deletions and frame-shifts has reconciled the inferiority complex allowing medicine, once again, to luxuriate in the eponym [8]. It usually takes a while for eponyms to settle down and the designated heroes to emerge. Inevitably, many eponymous attributions attract rival claims for priority on behalf of others who provided earlier accounts of that particular disorder. Indeed, a brief wander through any reasonable library easily identifies examples appearing before the eponym-defining publication(s). In writing A Practical Treatise of Painful Distempers with Some Effectual Methods of Curing Them, Exemplified in a Great Variety of Histories (1739), Theophilus Lobb (1678?1763) considered some of the most frequent and common painful distempers which afflict human bodies: they are many, and some of them very dreadful, both on account of the exquisite torment they give, and the hazard into which they put the lives of those who fall under them [9]. Mrs M-y W?r, aged 24 years, seen on 26 April 1733, complained that for several days she had noticed pains in the bottom of her feet and pricking in the ankles such that she could not tell how to walk. A complete cure of the complaint, caused by acrid particles brought into contact with the extremities of the nerves of her feet, was soon effected through the judicious administration of various tinctures. As a general conclusion, Dr Lobb anticipated subsequent elucidation of the pathology and mechanisms of demyelinating peripheral neuropathies: If the covering membrane of the nerves happens to be corroded, and the extremities of them made naked, acrid particles by striking thro?(ugh) the common covering membrane of the nerves, may excite pain. John Pearce [10] has drawn attention to the epidemic of acute sensorimotor polyneuropathy in Paris, described by Auguste Francois Chomel (1788?1858) [11], and observed by Robert Graves (1796?1853) during his Parisian visit in the summer of 1828?the illness characterised by sensations of pricking and severe pain in the integuments of the hands and feet, accompanied by so acute a degree of sensibility that the patients could not bear these parts to be touched by the bed-clothes [followed by] a diminution or even absence of sensation the power of motion declined advancing with progressive pace. This and the subsequent work of Louis Dumenil (1823?1890) of Rouen [13] went largely unnoticed. Grainger Stewart reported 3 examples of the illness already described by Graves [15]. He noted loss of the tendon reflexes (which Grainger Stewart had introduced into routine medical practice in the United Kingdom), and electrical inexcitability of the limbs. Whereas the brachial plexus was normal, the axis cylinders in nerves of the forearms had undergone degeneration. Between 1861 and 1876, Grainger Stewart progressed steadily from lecturer and consultant in pathology and medicine to professor of physic at the Royal Infirmary of Edinburgh. His most influential books were the Teaching of Medicine in Edinburgh (1877) and An Introduction to Disease of the Nervous System (1884). Attendance grew steadily at his lectures in the Extra-Academical School in Edinburgh. The 2 manuscript notebooks in which Grainger Stewart drafted these 141 lectures cover 594 pages [16]. Lecture 98 includes a section on Paralysis and other conditions due to disease of nerve endings or nerves (neuritis, peripheral neuritis, multiple neuritis, alcoholic paralysis). Amongst other details, the attentive medical students were told: Paralysis and other cond[i]t[ions] due to dis[ease] of n[erve] endings or nerves. We noted that there was paralysis in hands & feet spread up to arms and legs & that there was interference of sensation and motion. Very often the dis[ease] affects the fib[rous] tiss[tissue] bet[ween] the fibres accounting for the parenchymatous changes. There is a change in the n[erve] medullary sheath centre of n[erve] and sens[ory] struct[ure]. Often the changes proper to the n[erve] begin at periphery and spread up towards centre. Occasionally there are patches on the n[erve] involved, normal p[ar]ts and then involved portions. It very seldom happens that peripheral n[erve] is confined to one n[erve] but gener[erally] occurs in hands and feet?spreads up. There is a peculiar sensation in hands at first there is awkwardness in the hands at first. These cases go on till pat[ient] is unable to help himself but with treat some good improve sets in always and then there are felt various morbid sensations and espec[ially] tenderness on press[ure] along line of nerves. Often serious sym[toms] arise viz by involving vital n[erve]; h[ear]t and resp[iratory] nerves may be attacked & death. Pasted alongside is the printed galley summarising the lecture with the annotation: Some get a peripheral neuritis recurring y[ea]r after y[ea]r. Despite this emphatic formulation of the diseases of peripheral nerve, Lecture 56 (pages 220?21) describes acute ascending paralysis (Landry) as a disease of the spinal cord. Wijdicks and Ropper credit James Wardrop (1782?1869) and Charles-Prosper Ollivier d?Angers (1796?1845) with original contributions to the subject [17]. Readers of this book will have little difficulty in identifying additional, equally deserving celebrants. But if we are to stick with eponym for describing patients with acute post-infectious polyneuropathy, why not the Lobb-Wardrop-Ollivier-Chomel-Graves-LandryDumenil-Grainger Stewart-Ross-Guillain-Barre-Strohl syndrome? Lobb T (1739) A Practical Treatise of Painful Distempers with Some Effectual Methods of Curing Them Exemplified in a Great Variety of Suitable Histories. Dumenil L (1864) Paralysie peripherique du mouvement et du sentiment portant sur les quatres membres. Grainger Stewart T (1881) Paralysis of the hands and feet from disease of the nerves. As well as being of intrinsic interest, the patient perspective may broaden medical sensibility to , and perception of, the experiential aspects of disease, and rightly give the impression that clinicians are actually listening to their patients rather than simply shaping their narratives for their own purposes. In the Heller/Vogel account, neurological problems began with weakness (difficulty pulling open a door, removing a heavy sweater over his head), along with dysphagia (trouble swallowing a meal after the first few mouthfuls, a symptom calculated to ring alarm bells in a prodigious eater?) and cacogeusia (food tasting metallic). The following day, a Sunday, Heller again noted food tasted metallic, as well as chewing his food more slowly than usual, and he reflected that something neurologically unpleasant was taking place inside me, something I could not control and could not fathom. His weakness was profound, with dysarthria and dysphagia requiring a nasogastric tube, and respiratory and cardiac monitoring. His major gripe was sleep deprivation, and then a fear of not waking from sleep, which led to low mood and psychiatric consultations. There was some doubt about the diagnosis because 2 lumbar punctures returned normal results and it was with relief (according to Heller) that a third puncture (all were reported to be painless) showed a raised protein, confirming the suspected clinical diagnosis. Despite a weakness so profound that he could not lift his head or roll over, Heller commented that I never once throughout the entire experience thought of myself as weak. In passing, Vogel gives an answer to the perennial question of why we refer to Guillain-Barre syndrome and not Guillain-Barre-Strohl syndrome, despite the tripartite authorship of the original 1916 paper. Brief notes on his illness appear in his political diaries [2], beginning with an entry on 5th May: I wasn?t feeling very well today. I have had this tingling in my legs and now my hands, and my face has been very hot and my skin has been rough. After consulting a fellow member of Parliament who was medically qualified and being reassured, Benn then consulted his general practitioner on 14th May: I reported the fact that I have got this tingling in my legs. At the moment, walking is like having on wellington boots full of water with a sponge in the feet. By 1st June, referral to a neurologist was made, and on 4th June I was taken to see Dr Clifford Rose [1926?2012], who examined me. If this was only a medical consideration, I would recommend you came into hospital at once.
Parents often struggle with knowing how much information to share with their children out of a wish to protect them from worry or fear medicine park oklahoma order epitol 100 mg with mastercard. Children who can communicate openly with their parents about their illness feel safer and experience less anxiety and depression symptoms 7 days pregnant buy epitol 100mg lowest price, no matter what their medical prognosis is medications derived from plants buy epitol with visa. Children who have been appropriately prepared tend to cope better with treatment demands and symptoms medicine xyzal buy discount epitol on-line, and most importantly continue to trust their parents as sources of information and support through hard times (9) symptoms you may be pregnant purchase 100mg epitol with amex. Course of transplant the days and weeks prior to transplant and through the process of induction chemotherapy are usually the most anxiety-provoking for patients and families medicine woman buy generic epitol 100mg. Anxiety tends to peak at this time and decline signifcantly after the actual transplant infusion, even though patients may remain in isolation awaiting engraftment for several more weeks. The prolonged hospitalization can be marked by signifcant discomfort and symptoms of nausea, pain, and fatigue, which should be treated aggressively with medication. Patients often fnd relief in other modalities as well, including hypnosis, behavioral therapy, and relaxation techniques. For many patients, physical symptoms steadily improve over time but may persist past discharge into the outpatient setting, which can be dismaying to patients who have not been adequately prepared. This is the work of getting better, and patients need encouragement to stay active in their own recovery. During this period, caregivers need signifcant support coping with, and keeping track of, extremely complex medical regimens?in some cases, patients take as many as 20-30 medications daily. Once the patient has been cleared to return to school, children should be involved in discussions and decisions about the re-entry process. This exercise can help the student fnd comfortable explanations that balance his or her need for privacy with answers that will satisfy the curiosity of peers. Adolescents and young adults may struggle with adherence to the recovery plan in the post-transplant phase due to a variety of psychosocial factors, including denial, anxiety, developmentally typical struggles with dependency and vulnerability, or posttraumatic stress disorder. Patients should be assessed for these and other issues, and to encourage positive personal care behaviors. Issues Surrounding Death When nearing death, the patient and the family need emotional support, space to allow for clear thinking, practical forms of assistance, and tremendous understanding. By this point, the family has likely endured countless struggles with the illness. Continuing the fght and looking towards experimental options are essential pieces of armor that families use to cope and, for some families, it may make sense to search for options as long as possible. No one can determine when a specifc family should cease searching for treatment; therefore, physicians can offer invaluable support by providing information and opportunities for discussion, helping families make decisions, accepting their choices, comforting them, and remaining available. Support after the death of a child, whether the child was very young or an adult, is essential yet surprisingly diffcult to fnd. Rarely do bereaved parents feel that their loss is understood?and in fact, others fnd it diffcult to understand what they are going through. Grieving parents may fnd it diffcult to accept support, except from people who have endured similar losses. Relationships between clinicians and families should not end abruptly during the bereavement period, as it is a most diffcult phase. Explaining to families that intense feelings of anger, regret, loneliness, and depression are part of the natural grieving process is often helpful. The added complication of a genetic illness?one that a family will continue to deal with for generations to come?adds to the complexity of coping after a child dies. Paper presented at the Association of Pediatric Oncology Social Workers meeting in Norfolk, Virginia. I no longer believe people travel through such predictable stages to some ultimate resolution. Furthermore, I failed to appreciate fully that families dealing with a genetic illness grieve a series of losses inherent in living with a child or children with a life-threatening illness. Even within a family, each person experiences emotions with different intensities and at varying times. We lost our daughter Katie in 1991 at the age of 12, and Kirsten died in 1997 at the age of 24. Our Amy is now 27 and her health is stable, but knowledge of this disease makes us fearful for her future. Living with our unspeakably profound losses has inescapably deepened and altered my understanding of the grieving process. The loss of the normal child one expected and eagerly anticipated can be devastating. The realization that one does not share the unreserved joy that others experience upon the birth of a child can be wrenching. Parents typically experience intense shock and a range of painful emotions as they realize that their child does not look like other children and may require a series of diffcult medical interventions. With that diagnosis comes the realization that the child has an inherited disorder that results in bone marrow failure, sometimes leukemia and other cancers, and a shortened life expectancy. The cumulative impact of this devastating information plunges parents into an immediate and extremely painful grieving process. But whenever the diagnosis is made, parents will experience the acute loss of the expectation that their child would lead a full and normal life. Learning what might lie ahead, they ache for their precious child and, indeed, for their entire family. With every acute crisis such as worsening bone marrow failure or the diagnosis of cancer, loved ones experience again the most painful phases of the grieving process. Parents may tell themselves that the diagnosis is inaccurate, that someone has made a dreadful mistake, or that there must be a magic pill that will make this go away. They carry on with their daily routines, perform regular tasks, and ask appropriate questions. This phase can last from hours to months and is often intermingled with other characteristics of grief. Roller coaster of emotions Shock and denial give way to a roller coaster of emotionality. Family members commonly experience feelings of crippling sadness, anger, guilt, anxiety, despair, terror, and being out of control. When parents have unknowingly passed lethal genes on to their children, feelings of guilt can be quite intense, even though guilt is entirely unjustifed. Following a successful bone marrow transplant, patients may experience decades of stability. Waves of sadness, anger, anxiety, and other disabling emotions are far less intense. With the appearance of new symptoms and the onset of feared or unexpected medical problems, they must deal, again, with the most painful phases of grief. Parents worry about how this illness will affect the emotional stability and coping abilities of their healthy children. The medical and emotional demands of this illness can absorb much, and at times all, of the parents time and attention, especially during times of medical crisis or extended intervention, such as transplant. Parents can feel guilty, fearing that their physical and emotional absence will negatively affect the entire family. The family needs to consider ways in which the unaffected siblings can obtain support during the most stressful times. Knowing that one is doing the best one possibly can under extremely diffcult circumstances can lessen guilt. I am always aware that I must not let our daughter feel left out, even inadvertently. She must never feel that our son gets all the attention because he is sick, or that he is loved more due to his illness. Usually, parents know no other person in their community whose child has the same disorder. Most parents feel that part of their role is to protect their children from 355 Fanconi Anemia: Guidelines for Diagnosis and Management dangerous, unhappy experiences. They feel helpless and out of control when confronted with the knowledge that they cannot shield their children from a life-threatening condition. Coping strategies I must use my energy to do something good for others?to put purpose to the pain. Many families have found that a focus on fundraising for research is an enormously therapeutic outlet, and one that might hasten lifesaving results. Parents of children with a life-threatening illness also need to give themselves a break. Families speak of having a greater compassion and empathy for the suffering of others. Instead of living in the past or future, some families consciously focus on making the most of the present. Some report deeper and more satisfying relationships with family and friends, and an enhanced capacity to appreciate the things they have taken for granted. The rush of support from caring friends and family, the public or private events that follow the death, and the need to survive this intense period can carry one through the initial days of the grieving process. But the enormity of the loss usually leaves the bereaved with overwhelming sadness, despair, and an intense longing for the child who has died. Marital issues Some couples report that struggling with a life-threatening illness and the death of a child brought them closer together. For others, their different coping strategies became a threat to their relationship. Some are uncomfortable expressing their feelings and believe they must project strength to their family and friends. Differences in coping often lead to marital stress, as spouses can feel misunderstood, unappreciated, and resentful of one another. Each may feel that the other spouse is unable or unwilling to provide suffcient emotional support. Some couples report an unhappy disruption of their previously satisfying sex lives together. Marriage counseling may be crucial to help couples learn to be more tolerant, understanding, and supportive of one another throughout this extremely painful time. Even those who have learned all they could about this disease, followed the advice of esteemed physicians, and tried their best to make the right decision at each step of the way can be riddled with guilt when a child ultimately dies. They may remember those times they could not be there for their child, and dismiss all the hours they spent, in fact, being there. If they felt responsible for protecting their child, they conclude they have ultimately failed. Parents need to reassure themselves that they made the best decision they could at that particular time, that they can never know the outcome of an alternative decision, and that they must learn to be more compassionate towards themselves. Crisis in religious beliefs Parents with strong religious convictions often state that their faith has brought them peace and comfort, and has enabled them to cope with this illness and the death of a child. Many fnd solace in the belief that everything happens for a reason, their child is in a better place, and someday they will be reunited with the lost child. They state that their religious community has been a tremendous source of help and support. For others, the suffering and death of a child have caused them to question their beliefs. Some experience a deeply painful crisis as they try to reconcile their frm convictions and the enormity of their suffering. Those who have always believed that God does not give us more than we can bear suspect that they have, in fact, been given more than they can bear. Parents who believe that everything happens for a reason, even when we cannot understand the reason, wonder what possible beneft could come from the suffering of an innocent child? Those who believe strongly in miracles question why a miracle did not rescue their precious child. A trusted minister, priest, rabbi, or other spiritual leader may be crucial in helping parents work through and come to peace with these most diffcult issues. One can suffer forgetfulness, memory loss, slowed thinking, confusion, short attention span, and diffculty in making decisions or problem solving. Common physical symptoms include insomnia, headaches, respiratory problems, higher blood pressure, gastro-intestinal problems, and weight gain or loss. Those experiencing chronic grief are themselves at higher risk for serious health problems. We can think of each of us as having a grief bank in which we make deposits (adding to our griefs/ traumas/losses) and withdrawals (letting go of our griefs/traumas/ losses). Every loss has a distinct weight and bundle of emotions, and as you move through life, you deposit each into your grief bank. With many losses, your bank becomes quite full, and as you grieve new losses, the contents mix and begin to spill over. It is an unimaginable and devastating tragedy to live for years or decades with multiple children with a complicated disorder; one that can pose a series of life-threatening challenges unique to each child, and that can end in the death of two or more children. Each loss reactivates a previous one as a parent relives the earlier emotions of loving and losing another child or children. The experience of grief is compounded and the work of integrating yet another loss is overwhelming. Families dealing with multiple losses need a tremendous amount of support and strong coping strategies to manage the grieving process. In addition to giving and receiving advice and emotional support, families are also deeply affected by the ups and downs of others in the support network. Ironically, the many medical challenges and ultimate loss of others in this close network can be threatening to other families and can add to the cumulative losses experienced by this unique group. It is an emotional, physical, and spiritual necessity, the price you pay for love. In my experience, anti-depressants and even therapy did not help (although both can help many). I fnally concluded that I owned this grief, and if life could ever become more bearable, I had to walk right through the middle of the most painful feelings imaginable. I had to cry (incessantly, my husband would say), and I had to express my deepest feelings if a special friend would listen.
Safe 100 mg epitol. Thyroid Storm Nursing Pathophysiology NCLEX Review Thyrotoxic Crisis.
In randomized symptoms of kidney stones buy epitol with american express, double-blind x medications buy epitol master card, placebo-controlled trials medications that cause constipation order epitol american express, the drug was well tolerated by patients with cancer or cystic fbrosis treatment jalapeno skin burn buy epitol discount, but resulted in little or no weight gain (12 treatment centers for alcoholism cheap epitol 100 mg free shipping, 13) medications names purchase epitol 100 mg fast delivery. However, some physicians elect to try this medication before resorting to nasogastric or gastrostomy feedings. Patients may beneft from cyproheptadine, as it improves gastric accommodation to reduce retching (14). Signifcant complications may result from overweight and obesity, including elevated levels of fat and cholesterol in the blood, diabetes, obstructive sleep disorder, and other aspects of metabolic syndrome?a combination of disorders that increase the risk of developing cardiovascular disease and diabetes. While a full discussion of the management of overweight and obesity is beyond the scope of this chapter (see references 16-18 for a review), some useful starting points can be offered. Physicians should ask patients to keep a 6-day diary of diet and daily activity, both of which provide the foundation for counseling regarding dietary and exercise changes. Most families will require monthly counseling sessions for a time to insure achievement of appropriate weight. Psychological counseling may also help, especially if an eating disorder is suspected. The obese patient should be assessed for the primary health consequences of obesity. Obese patients with sleep disturbance or snoring will require a sleep study and may need an echocardiogram (a noninvasive imaging procedure that is used to assess heart function). Management of overweight and obesity is a long-term process, requiring the commitment of the entire family for success. Patients should be urged to avoid fad diets and over-the-counter weight loss preparations and to focus on healthy lifestyle modifcations. Screening for esophageal carcinoma can be 86 Chapter 4: Gastrointestinal, Hepatic, and Nutritional Problems done using an endoscope, a thin, fexible tube-like device used to look inside the body. Some experts recommend yearly ultrasound imaging of the liver to screen for liver tumors, even for the youngest patients. Good to Know Androgens are hormones produced in the body that stimulate the development of male sex characteristics, such as testes formation and sperm production. As a general rule, patients with liver disease should be referred to a gastroenterologist with expertise in liver disease. Thus, careful monitoring for hepatic complications of androgen therapy is essential. This condition can occur with any dose of androgen therapy and at any time during treatment. This condition is best diagnosed via liver biopsy, although imaging techniques. There are case reports of liver cirrhosis in patients on continued androgen therapy (19). Cessation of androgen therapy will usually lead to complete resolution of symptoms. However, if liver enzyme levels do not return to normal after androgen withdrawal, then liver biopsy may be indicated (see more information on androgens in Chapter 3). An adenoma is a benign tumor that does not invade surrounding tissue; however, it can rupture, leading to life-threatening bleeding. The risk of bleeding in hepatocellular adenomas is increased in patients with thrombocytopenia, a condition in which the blood has an abnormally low number of platelets, which help blood to clot. Elevated levels of conjugated bilirubin refect obstruction of bile fow in the liver or signifcant liver cell injury. Liver cell function can be investigated by testing how quickly the blood clots. A Doppler ultrasound may reveal the accumulation of fat or scar tissue, impaired blood fow, and obstruction of bile fow in the liver. Patients with elevated liver enzyme levels should have a full evaluation of their liver by a hepatologist or pediatric hepatologist. Patients should be immunized against varicella zoster virus (unless live virus vaccines are contraindicated), hepatitis A virus, and hepatitis B virus. The levels of antibodies against these viruses should be measured to insure that the patient has acquired immunity. Drugs that are toxic to the liver, including alcohol, should be avoided when possible. Levels of fat-soluble vitamins should be monitored on a yearly basis in patients with most forms of liver disease, particularly in cases where bile fow is reduced, known as cholestatic disease. If undiagnosed chronic abdominal pain exists, endoscopy for detection of potential sources of bleeding or infection may be required. In addition, diarrhea should be evaluated to detect opportunistic organisms, optimal nutritional status should be achieved, and the liver cell injury and/or function should be evaluated (see above) prior to the transplant. Pancreatic insuffciency?a lack of digestive enzymes made by the pancreas that results in impaired food digestion?is uncommon, but should be considered in patients with poor absorption of fat. Cholestasis may lead to poor absorption of the fat-soluble vitamins A, E, D, and K; therefore, levels of these vitamins should be monitored to determine whether vitamin supplementation is needed. Physicians participating in the long-term management of these patients must be aware of this risk. Good to Know Transferrin is a protein in the body that binds and transports iron in the blood. Transferrin saturation refers to the amount of iron carried by the transferrin protein in the blood. The levels of ferritin in the blood increase as the amount of iron in the body increases. The unsaturated iron binding capacity test reveals the amount of transferrin that is not being used to transport iron. A single transfusion unit of packed red blood cells contains 200-250 mg of elemental iron. The body is unable to excrete excess iron; thus, all iron obtained via transfusions must be deposited somewhere in the body. The organs most commonly affected by iron overload include the liver, pancreas, and heart. Patients with iron overload are generally asymptomatic; fatigue is the only commonly reported symptom. Patients often have an enlarged liver, which may be discovered by physical exam, and elevated blood levels of the liver enzyme aminotransferase. Cirrhosis is a rare but irreversible complication of iron overload; therefore, it is important to prevent liver fbrosis, the scarring process 92 Chapter 4: Gastrointestinal, Hepatic, and Nutritional Problems that occurs in response to liver injury that can lead to cirrhosis. Fibrosis may occur earlier than usual in patients with viral hepatitis (particularly hepatitis C), non-alcoholic fatty liver disease, and/or alcohol abuse. Diabetes, joint pain, and heart disease are common in patients with severe iron overload and liver disease. Heart disease may include cardiomyopathy (weakening and enlargement of the heart muscle), irregular heartbeats, or heart failure. Patients receiving blood transfusions should be screened yearly for iron overload. Screening is performed using blood tests to measure transferrin saturation, ferritin, and unsaturated iron binding capacity. Patients with highly elevated blood levels of amino acids, obesity, or those suspected of chronic alcohol consumption may need a liver biopsy to detect liver disease or to determine the extent of liver injury due to other causes. Patients who develop iron overload at an early stage in their blood transfusion history or who have a family history of primary iron overload should undergo genetic testing for hemochromatosis, an inherited disorder that causes the body to absorb too much iron. Free radicals are naturally produced in the body as our cells use energy, and may be produced in response to environmental factors such as pollution. Patients with iron overload should avoid vitamins or medications containing iron and vitamin C, but do not need to restrict their consumption of foods 93 Fanconi Anemia: Guidelines for Diagnosis and Management containing iron and vitamin C. Oral chelation should be chosen and monitored in consultation with a physician with some experience with these agents. Nutrition as Therapy Complementary and alternative therapies include any treatments and practices that have not been shown to be effective by evidence-based clinical studies. Complimentary therapies are used in conjunction with standard medical care, and alternative therapies are used in place of standard medical care. Many families view food, and by extension, dietary supplements, vitamins, and micronutrients, as natural and thus safe. The multi-billion dollar industry that produces complementary/alternative nutritional regimes lacks federal regulation and has a clear incentive to promote its products regardless of the degree of evidence of the effectiveness of these products. Many complementary/alternative nutritional regimes and supplements are directly harmful or, by displacing standard medical therapy, indirectly harmful. Controlled clinical trials of 94 Chapter 4: Gastrointestinal, Hepatic, and Nutritional Problems supplements are necessary to demonstrate effectiveness and limit the risk of toxicity. Products containing iron must be avoided to reduce the risk of exacerbating iron accumulation in the liver and other tissues. Vitamin C increases iron absorption; therefore, products containing vitamin C, such as multivitamins or fortifed fruit juices/drinks should be avoided. In large studies, both vitamin A and vitamin E supplements have been associated with an increased risk of some cancers; therefore, they should be avoided until further study indicates otherwise. Large doses of omega-3 fatty acids, commonly found in fsh oil supplements, can increase the risk of bleeding due to inactivation of platelets, blood cells that mediate blood clotting. Establishing a non-judgmental, but candidly informative discussion of complementary and alternative therapies offers the physician a chance to educate parents about their choices. Physicians and families can access information about complementary/alternative nutritional therapies at the website of the Offce of Complementary and Alternative Medicine of the National Institutes of Health, available at: Pediatric neurogastroenterology: gastrointesinal motility and functional disorders in children. Rodriguez L, Diaz J, Nurko S (2013) Safety and effcacy of cyproheptadine for treating dyspeptic symptoms in children. Westaby D, Portmann B, Williams R (1983) Androgen-related primary hepatic tumors in non-Fanconi patients. A surgical procedure that creates a functional thumb by moving the index fnger and its nerves, arteries, tendons, and muscles to the thumb position. A so-called foating thumb that lacks bones and is composed of skin and soft tissue. Children with these anomalies might have a shortened or absent thumb, radius, or both, due to incomplete growth. There are no standardized treatment procedures for congenital hand and arm abnormalities; treatments must be tailored to each child and family. The decision process is multi-factorial and requires participation from the family, physician team, and a physical or occupational therapist. Initial Evaluation Children born with limb abnormalities should be referred to an upper extremity specialist within the frst few months of life. This physician should be comfortable with and profcient in the diagnosis and management of congenital limb anomalies. It is important for physicians to encourage this type of conversation; otherwise, parents often seek health information via the Internet, which can be a source of misinformation. A physical or occupational therapist can offer adaptive devices or techniques to help the child accomplish these tasks. Furthermore, radial defciency incomplete formation of the radius?is associated with numerous syndromes, further emphasizing the need for a thorough investigation (Table 1). The most common types of thumb anomalies that occur in children have been classifed into fve types depending on the degree of underdevelopment (2): This mild defciency may go unrecognized, and many individuals with this type of defciency are not diagnosed until later in life when everyday activities such as buttoning a shirt or tying shoes have become more diffcult. This defciency is more involved and is characterized by a narrowing of the web space between the thumb and index fnger, 102 Chapter 5: Hand and Arm Abnormalities absence of the thenar (thumb) muscle at the base of the thumb, and instability of the metacarpophalangeal joint in the middle of the thumb (Figures 1A and B). A) Absent thenar muscles; B) Narrowed thumb-index web space with instability of the metacarpophalangeal joint. These abnormalities usually involve tendons that arise within the forearm and travel into the thumb. This type of defciency, known as a pouce fottant (foating thumb) or residual digit, lacks bones and muscles and is mainly comprised of skin and soft tissue (Figure 2). Figure 2 (see Figure legend on next page) 103 Fanconi Anemia: Guidelines for Diagnosis and Management Figure 2. The thumb classifcations listed above can guide treatment recommendations, as shown in Table 2 (3,4, 5). Tendon transfer improves the active motion and function of the thumb and has a negligible effect on the donor fnger (Figure 4B). A) Z-plasty of the narrowed thumb-index web space; B) tendon transfer to overcome the defcient thenar muscles; C) ligament reconstruction to stabilize the metacarpophalangeal joint instability. In cases with severe instability, fusion of the joint may be the best option to provide a stable thumb for frm grasps. The main distinction between a thumb that can be surgically reconstructed and a thumb that requires amputation is the presence or absence of a stable base. The decision to remove a hypoplastic thumb without a stable base is often a diffcult process for parents and caregivers. Discussions with the surgeon and conversations with families who have made similar decisions are often helpful to parents tasked with making this decision for their child (Video 1 in online supplementary information). An X-ray of a 2-year-old child reveals a thumb metacarpal that tapers to a point, indicative of an unstable carpometacarpal joint. The right index-long web space has widened and the index has rotated out of the palm.
Teachers and others are encouraged to consult these publications and to use them in conjunction with Identifying and Treating Attention Deficit Hyperactivity Disorder: A Resource for School and Home medications gabapentin buy epitol 100 mg line. As the documents become available medications bad for your liver purchase epitol uk, they will be listed on the Office of Special Education and Rehabilitative Services/Office of Special Education Programs Web site ( Clinical practice guideline: Diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder medicine 44 159 purchase epitol toronto. Clinical practice guideline: Treatment of the school-aged child with attention deficit/hyperactivity disorder in treatment 1 buy 100mg epitol with visa. Comprehensive evaluation of attention deficit disorder with and without hyperactivity as defined by research criteria symptoms 5 days before missed period buy epitol 100 mg with visa. Estimates of the prevalence of childhood maladjustment in a community survey in Puerto Rico treatment h pylori buy epitol 100mg fast delivery. Developing 504 classroom accommodation plans: A collaborative systematic parent-student-teacher approach. Association between attention deficit-hyperactivity disorder and learning disorders. Single and combined effects of methylphenidate and behavior therapy on the classroom performance of children with attention-deficit hyperactivity disorder. Prepared for the Office of Special Education Programs, Office of Special Education and Rehabilitative Services, U. Epidemiology and course of psychiatric disorders in school-age children: Results of a longitudinal study. Efficacy of methylphenidate for attention-deficit hyperactivity disorder in children with tic disorder. The impact of attention deficit hyperactivity disorder on social and vocational functioning in adults. Clinical efficacy of methylphenidate in conduct disorder with and without attention deficit hyperactivity disorder. Synthesizing and Verifying Effective Practices For Children and Youth With Attention Deficit Disorder. Fourteen-month randomized clinical trial of treatment strategies for attention-deficit hyperactivity disorder. Effects of comorbid anxiety, poverty, session attendance, and community medication on treatment outcome in children with attention deficit/hyperactivity disorder. Empirically supported psychosocial treatments for attention deficit hyperactivity disorder. Comparing classroom and clinic measures of attention deficit disorder: Differential, idiosyncratic, and dose-response effects of methylphenidate. Comparison of diagnostic criteria for attention-deficit hyperactivity disorder in a county-wide sample. Research on the educational implications of attention deficit hyperactivity disorder. A considerable amount of literature has been published since these previous reviews were performed, necessitating an update of the corresponding practice parameters. The treatment of restless legs syndrome and periodic limb movement disorder in adults?an update for 2012: practice parameters with an evidence-based systematic review and meta-analyses. Two previous reviews symptoms with physical activity, and (4) worsening of symphave been published by the American Academy of Sleep Medicine toms in the evening or at night. Also, studies with less than 1 week of sleep quality, and quality of life, both subjectively and objectreatment time were rejected. There is some consensus in recent studies to focus on the and supplemented by pearling. A variety of other scales have been used the result of each meta-analysis is shown in a fgure with occasionally such as the Self-Rating Zung Depression Scale several components. The vertical red line indicates the average response of all studthe only objective measurements included are sleep-reies. The magnitude of the effect across all studies is given by the value of the association 3. All therapies estimate of effect (see footnote following article) is generated were searched with a start date of 11-1-1997 (6 months prior to for each outcome. Results on dopaminergic treatments between cluding study limitations, imprecision, inconsistency of results, 11-1-97 to 11-1-2001 already covered in the 2004 update were indirectness of evidence, and likeliness of publication bias. The search was performed frst on August 12, 2010, and dose-response associations, and all plausible confounders that updated again on June 29, 2011, to capture the latest literature. Also reported are the number of patients that were studied, blinding, allocation concealment, large loss to follow-up, or the overall effect that was calculated in the meta-analysis (reselective outcome reporting. Indirectness occurs One reviewer extracted the data and graded the studies and when the question being addressed is different than the availanother verifed this compiled information. The systematic reable evidence regarding population, intervention, comparator, view of the evidence was additionally reviewed by an outside or outcome. There is inconsistency when there is unexplained expert who was an author on both previous review papers (2004 heterogeneity of the results. Sections titled Values Very low: We have very little confdence in the effect estimate: the true and Trade-offs appear under each individual practice paeffect is likely to be substantially different from the estimate of effect. The Values and Trade-offs discussion elucidates the rationale leading to each recommendation. Table 4 shows a summary of the recmade by the physician, in light of the individual circumstances ommendation statements organized by strength of recommendapresented by the patient, available diagnostic tools, accessible tion, including the body of evidence level, the assessment of the treatment options, and resources. Some other studies have been published that were low level evidence (Saletu et al. An additional 8 short-term studies30-37 (3 to 12 weeks) toms over those who continued to receive pramipexole. All dosing in the day, small dose increases,46 or increased doses data can be found in the online supplement at. The body (3) the daily dose of pramipexole at the time of discontinuation of evidence level is judged to be high. This conclusion is based on an analysis of pooled data57 from four 12-week clinical trials49-51,53 of 223 patients 4. Compared to those without augValues and Trade-Offs: this recommendation is upgraded mentation, patients with augmentation were signifcantly more to standard from the previous practice parameter based on mullikely to be on higher doses of levodopa (? Ropinirole is typically well tolerated and side effects are self limited with cessation of ropinirole therapy. For those that require daily therapy for has been progress in understanding augmentation. The mean dose for the double-blinded patients was unchanged, and 9% were slightly worse. However, treatment did not improve sleep effciency the authors conclude that low-dose pergolide was well toleror subjective sleep quality with respect to placebo. Some patients alternated tramadol with levodopa or clonazepam while other patients took 4. A metaon long-term opioid therapy should be clinically or polysomanalysis was performed on these data. Two studies83,85 were 12 nographically monitored periodically for the development of weeks in duration, and 184 was only 2 weeks long. All data are presented in the three percent of the patients remained on methadone for 23 Appendix. In a randomized open clini2-period cross-over study87 reported the effect of 1200 mg/d cal trial, Happe et al. There are some concerning potential side effects which is the following: although their study was not prospectively demakes the balance of benefts versus harms uncertain. CalculaValues and Trade-Offs: this is a new recommendation tions indicated that 123. Twenty-four pregabalin and 19 plaGabapentin enacarbil therapy is generally well tolerated with cebo patients completed the trial. The dropouts for lack of treatment effect the last complete review where there were 2 small studies of 112 97 were higher in the placebo group (61% vs. This is a new treatment reactions, including fatalities, have followed the parenteral since the last review, and the evidence base is 5 studies107-111 for administration of iron dextran injection. No limitations were noted with the studies, recommends administering a test dose prior to the frst theraand the results were consistent. The parenteral infusion sleep satisfaction, and QoL supported the effcacy of rotigotine. Moreover, parenteral iron therapy with iron sucrose, iron tiveness up to approximately 3 mg/d. For example, clonazepam Transdermal rotigotine was withdrawn from the market because could still be considered as an adjunctive medication in treatof drug crystallization that resulted in suboptimal absorption. With the exceprisk of neural tube defects and other major birth defects, such tion of nausea and dizziness in one patient, none of the adverse as craniofacial defects and cardiovascular malformations, in baevents were rated as severe. There is insuffcient evidence at this time to support the use of talipexole, peribedil, and alpha-dihydroergocryptine in the 4. A higher odds ratio was found with had an acute therapeutic effect on insomnia, which is a different the concomitant use of tramadol and dopamine-blocking agents. No adverse events were reported during ropinirole treatThere is insuffcient evidence at present to evaluate the use of ment. All patients self-rated a satisfactory or good alleviation tient groups for a recommendation to be made. Melatonin to circumvent this limitation is to include cognitive behavioral improved Zerssen well-being (a self-rating mood scale) in 7 of therapies or psychotherapy as part of the treatment regimens. Where dopamine meets opioids: a meta-analysis of tio, relative risk reduction, standardized mean difference, or the placebo effect in restless legs syndrome treatment studies. Gambling and increased the committee would also like to thank Christopher Earley, sexual desire with dopaminergic medications in restless legs syndrome. Dopamine dysregulation syndrome: an overview of its epidemiology, mechanisms and management. Effect of pramipexole of restless legs syndrome and periodic limb movement disorder. Effcacy and safety of pramipextion of sleep disorders, 2nd Edition: Diagnostic and coding manual. Restless legs syndrome: diagnostic in restless legs syndrome: A six-week, multicenter, randomized, doublecriteria, special considerations, and epidemiology. Cochrane Handbook for Systematic Reviews of pexole for the symptomatic treatment of restless legs syndrome: polysomInterventions Version 5. In: the Cochrane nographic evaluation of periodic leg movements and sleep disturbance. Grading and quality of evidence and in restless legs syndrome: experience from two clinical trials. Effcacy and safety of pramipexole Results from a multi-center, randomized, active controlled trial. Mov Disin idiopathic restless legs syndrome: a polysomnographic dose-fnding ord 2007;22:696-703. A 10-year, longitudinal assesscaused by ergotand nonergot-derived dopamine agonists. Mov Disord ment of dopamine agonists and methadone in the treatment of restless legs 2009;24:129-33. Ropinirole for restless legs synheart disease and the use of cabergoline for the treatment of prolactinoma. Assessment of cardiac valve dysis effective in the treatment of restless legs syndrome. Neurology domized, double-blind, placebo-controlled, short-term trial of ropinirole 2006;67:1225-9. Ropinirole decreases periodic leg bo-controlled study of the treatment of periodic limb movements in sleep movements and improves sleep parameters in patients with restless legs using carbidopa/levodopa and propoxyphene. Patientand physician-rated idiopathic restless legs syndrome in a randomized double-blind trial of measures demonstrate the effectiveness of Ropinirole in the treatment of oxycodone versus placebo. One-year treatment with the treatment of patients with primary restless legs syndrome. Sleep standard and sustained-release levodopa: Appropriate long-term treat2009;32:159-68. Progressive development placebo-controlled study to assess the effcacy and tolerability of gabapof augmentation during long-term treatment with levodopa in restless entin enacarbil in subjects with restless legs syndrome. Clin Neuropharmacol effective single-drug treatment for restless legs syndrome: Clinical and 2011;34:8-16. One year open-label term maintenance treatment of restless legs syndrome with gabapentin safety and effcacy trial with rotigotine transdermal patch in moderate enacarbil: a randomized controlled study. Treatment of moderate to ropinirole in the treatment of idiopathic restless legs syndrome. Neurosevere restless legs syndrome: 2-year safety and effcacy of rotigotine psychobiology 2003;48:82-6. Treatment of restless legs syndrome with gabapentin: A done on pharmacokinetics, safety and tolerability of the dopamine agonist double-blind, cross-over study. Transdermal lisuride: short-term effcacy and tolerability study dose-ranging study of pregabalin in patients with restless legs syndrome. Treatment of restment of restless legs syndrome: First studies with monotherapy in de novo less legs syndrome with pregabalin: a double-blind, placebo-controlled patients and in combination with levodopa in advanced disease. Treatment of the restless legs syndrome with carbamazepine: a Disord 2000;16:579-81.