Darnelle L. Dorsainville, MS, CGC
- Board Certified Genetic Counselor
- Division of Genetics
- Department of Pediatrics
- Albert Einstein Medical Center
- Philadelphia, Pennsylvania
In some instances symptoms and diagnosis buy generic coversyl 4mg line, blood is aspirated through the insufflation needle before the introduction of the distending gas symptoms diverticulitis order coversyl without prescription. In such instances treatment ulcerative colitis generic 4 mg coversyl with amex, the needle should be left in place while immediate preparations are made to obtain blood products and perform laparotomy symptoms zinc deficiency adults order coversyl with paypal. The bleeding frequently will be contained in the retroperitoneal space symptoms adhd discount coversyl line, which usually delays the diagnosis; consequently treatment nail fungus purchase coversyl once a day, hypovolemic shock may develop. To avoid late recognition, the course of each great vessel must be identified before completing the procedure. Because it is difficult to assess the volume of blood filling the retroperitoneal space, immediate laparotomy is indicated if retroperitoneal bleeding is suspected. Upon entry into the peritoneal cavity, the aorta and vena cava should immediately be compressed just below the level of the renal vessels to gain at least temporary control of blood loss. Vascular or general surgery consultation may be necessary to evaluate and repair significant vascular injuries. Although most of these injuries are small and amenable to repair with suture, some are larger and require the insertion of a vascular graft. Abdominal Wall Vessel Injury the abdominal wall vessels most commonly injured during laparoscopy are the superficial inferior epigastric vessels as they branch from the femoral artery and vein and course cephalad in each lower quadrant. They are invariably damaged by the initial passage of an ancillary trocar-cannula system or by the introduction of a wider device later in the procedure. The problem may be recognized immediately by the observation of blood dripping along the cannula or out through the incision. However, the bleeding may be obstructed by the cannula until it is withdrawn at the end of the operation. The more serious injuries are those to the deep inferior epigastric vessels, which are branches of the external iliac artery and vein that course cephalad but are deep to the rectus fascia and often deep to the muscles (Fig. More laterally located are the deep circumflex iliac vessels, which are not often encountered in laparoscopic surgery. Laceration of these vessels may cause profound blood loss, particularly when the trauma is unrecognized and causes extraperitoneal bleeding. Signs of injury, in addition to blood dripping down the cannula, include the postoperative appearance of shock and abdominal wall discolorization or hematoma located near the incision. In some instances, the blood may track to a more distant site, presenting as a pararectal or vulvar mass. Delayed diagnosis may be prevented by laparoscopic evaluation of each peritoneal incision after removal of the cannula. Superficial inferior epigastric vessel trauma usually stops bleeding spontaneously; therefore, expectant management is appropriate. A straight ligature carrier can be used to repair lacerated deep inferior epigastric vessels. Alternatively, a Foley catheter may be inserted through the cannula, inflated, put on traction, and held in place with a clamp for 24 hours. Open removal or aspiration of the hematoma should not be undertaken because it may inhibit the tamponade effect and increase the risk of abscess. If the mass continues to enlarge or if signs of hypovolemia develop, the wound must be explored. Intraperitoneal Vessel Injury Hemorrhage may result from inadvertent entry into a vessel or failure of a specific occlusive technique. Transected arteries may go into spasm and bleed minutes to hours later, going unnoticed temporarily because of the limited visual field of the laparoscope. Therefore, at the end of the procedure, all areas of dissection must be carefully examined. Carbon dioxide should be vented, which decreases the intraperitoneal pressure so that blood vessels temporarily occluded by higher pressure can be recognized. Gastrointestinal Complications the stomach, the small bowel, and the colon can be injured during laparoscopy. Mechanical entry into the large or small bowel can occur 10 times more often when laparoscopy is performed in patients who have had prior intraperitoneal inflammation or abdominal surgery. Loops of intestine can adhere to the abdominal wall under the insertion site and be injured (117,118). Insufflation Needle Injuries Needle entry into the gastrointestinal tract may be more common than reported because it may go unnoticed and without further complication. Gastric entry may be identified by the increased filling pressure, asymmetric distention of the peritoneal cavity, or aspiration of gastric particulate matter through the lumen of the needle. Initially, the hollow, capacious stomach may allow the insufflation pressure to remain normal. Signs of bowel entry are the same as those for gastric injury, with the addition of feculent odor. If particulate debris is identified, the needle should be left in place, and an alternate insertion site should be identified, such as the left upper quadrant. Immediately after successful entry into the peritoneal cavity, the site of injury can be identified. Trocar or Obturator Injuries Damage caused by a sharp tipped obturator or trocar is usually more serious than needle injury. Inadvertent gastric entry usually is associated with stomach distention because of aerophagia, difficult or improper intubation, or mask induction with inhalation anesthetic. Most often the injury is created by the trocar-cannula system used for primary access. Ancillary cannulas may result in visceral injury, although placement of these cannulas under direct vision helps reduce the risk of injury. The risk of gastric perforation can be minimized with the selective use of preoperative nasogastric or oral gastric suction when left upper-quadrant entries are used or when the intubation was difficult. Open laparoscopy likely has little impact on the risk for gastrointestinal complications, particularly those related to adhesions to the anterior abdominal wall from previous surgery. If the trocar of a primary cannula penetrates the bowel, the condition is usually diagnosed when the mucosal lining of the gastrointestinal tract is visualized. However, the injury may not be recognized immediately because the cannula may not stay within the bowel or may pass through the lumen. Such injuries usually occur when a single loop of bowel is adherent to the anterior abdominal wall. The injury may not be recognized until peritonitis, abscess, enterocutaneous fistula, or death occurs (123,124). Therefore, at the end of the procedure, the removal of the primary cannula must be viewed either through the cannula or an ancillary port, a process facilitated by routine direct visualization of closure of the incision of the primary port. Trocar-related injuries to the stomach and bowel require repair as soon as they are recognized. If the injury is small, a trained operator can repair the defect under laparoscopic direction using a double layer of running 2-0 or 3-0 absorbable sutures. Extensive lesions may require resection and reanastomosis, which in most instances requires at least a small laparotomy. The preoperative use of mechanical bowel preparation in selected high-risk cases minimizes the need for laparotomy or colostomy, but recent evidence suggests that bowel surgery, if necessary, may be safely performed in unprepared bowel (125). Dissection and Thermal Injury When mechanical bowel trauma is recognized during the dissection, treatment is the same as that described for trocar injury. Should the injury involve radiofrequency electrical energy, it is important to recognize that the zone of desiccation and coagulation may exceed the area of visual damage. This is especially true if the exact mechanism of the thermal injury is unknown or if injury results from contact with a relatively large surface area electrode that would be more likely to create a large coagulation injury. Conversely, bowel injury created under direct vision with a radiofrequency needle or blade electrode is associated with little collateral coagulation effect and can be managed similar to a mechanically induced lesion. Consequently, surgical repair should be implemented considering these factors, and should include, if necessary, resection of ample margins around the injury. Thermal injury may be handled expectantly if the lesion seems superficial and confined, such as when fulguration (noncontact arcing of high-voltage current) involves bowel. In a study of 33 women with such injuries who were managed expectantly in the hospital, only 2 required laparotomy for repair of perforation (126). Urologic Injury Damage to the bladder or ureter may occur secondary to mechanical or thermal trauma incurred during laparoscopic procedures. Ideally, such injury should be prevented; otherwise, as is the case for most complications, it is preferable to identify the trauma intraoperatively. Bladder Injury Bladder injury can result from the perforation of the undrained bladder by an insufflation needle or trocar, or it may occur while the bladder is being dissected from adherent structures or from the anterior uterus (127,128). Estimates of the frequency of unintentional cystotomy associated with laparoscopic hysterectomy range from 0. A2 bladder laceration can be confirmed by injecting sterile milk or a diluted methylene blue solution through a transurethral catheter. Thermal injury to the bladder, however, may not be apparent initially and, if missed, can present as peritonitis or a fistula. Routine preoperative bladder drainage usually prevents trocar-related cystotomies. Separation of the bladder from the uterus or other adherent structures requires good visualization, appropriate retraction, and excellent surgical technique. Sharp mechanical dissection is preferred, particularly when relatively dense adhesions are present. Very small-caliber injuries to the bladder (1 to 2 mm) may be treated with bladder catheterization for 3 to 7 days. When a larger injury is identified, it can be repaired laparoscopically (127,128,131). If the laceration is near the trigone or involves the trigone, an open procedure should be used. The mechanism of injury should be taken into consideration in making this evaluation because electrical injuries often extend beyond the visible limits of the apparent defect. If a coagulation-induced thermal injury occurred, the coagulated portion should be excised. For small lesions, closure may be performed with layers of absorbable 2-0 to 30 sutures. Postoperative catheterization with either a transurethral or suprapubic catheter should be maintained for 2 to 5 days for small fundal lacerations and for 10 to 14 days for injuries to the trigone. Ureteral Injury One of the most common causes of ureteral injury during laparoscopy is electrosurgical trauma (113,132,133). Although intraoperative recognition of ureteral injury is possible, the diagnosis is usually delayed (132,133). Ureteral lacerations may be confirmed intraoperatively, visually, or following the intravenous injection of indigo carmine. Thermal injury presents up to 14 days after surgery with fever, abdominal or flank pain, and peritonitis. Leukocytosis may be present, and intravenous pyelography shows extravasation of urine or urinoma. Mechanical obstruction from staples or a suture may be recognized intraoperatively by direct visualization. Cystoscopy following the intravenous injection of indigo carmine may be used to confirm failure of the dye to pass through the ureter. Unrecognized ureteral obstruction may present a few days to 1 week after surgery with flank pain and often fever (136). Discharge or continuous incontinence is a delayed sign of ureterovaginal or vesicovaginal fistula. A vesicovaginal fistula can be confirmed by filling the bladder with methylene blue and then detecting dye on a tampon previously placed in the vagina. With a ureterovaginal fistula, the methylene blue will not pass into the vagina, but it can be detected with the intravenous injection of indigo carmine. Knowledge of the course of the ureter through the pelvis is a prerequisite to reducing the risk of injury. The ureter can usually be seen through the peritoneum of the pelvic sidewall between the pelvic brim and the attachment of the broad ligament. Because of variation from one patient to another or the presence of disease, the location of the ureter can become obscured, making it necessary to enter the retroperitoneal space. The techniques used for retroperitoneal dissection are important factors in reducing the risk of ureteric injury. Blunt and sharp dissection with scissors is preferred, although hydrodissection can be used (137). Although limited damage may heal over a ureteral stent left in place for 10 to 21 days, repair is indicated in most patients. Laparoscopic repair of ureteric lacerations and transections is performed, but most injuries require laparotomy (132,138). Incomplete or small obstructions and lacerations may be treated successfully with either a retrograde or anterograde ureteral stent. If a stent cannot be placed successfully, a percutaneous nephrostomy should be performed before operative repair is undertaken. Repair may be accomplished by excision and reanastamosis, or, more commonly, ureteric reimplantation with or without facilitating procedures such as a psoas hitch or a Boarie flap. Neurologic Injury Peripheral nerve injury is usually related either to poor positioning of the patient or to excessive pressure exerted by the surgeons. Positioning the patient in lithotomy while she is awake may decrease this risk because the patient can determine whether any undue pressure or discomfort is felt (139). In the extremities, the trauma may be direct, such as when the common peroneal nerve is compressed against a stirrup. The femoral nerve or the sciatic nerve or its branches may be overstretched and damaged by excessive flexion or external rotation of the hips.
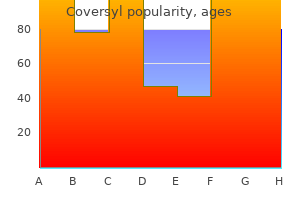
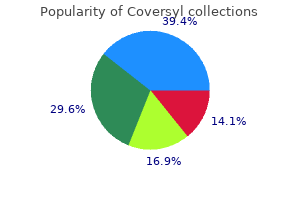
In persons whose audiogram curves exhibit an abrupt drop treatment zone guiseley buy coversyl pills in toronto, the average of the best two frequencies may give better correlation treatments purchase 8mg coversyl with mastercard. These individuals have difficulty in group conversation or when listening against a background of noise medications 2015 order coversyl overnight. An observation (or history) of appreciable improvement in hearing (even though transient) following the introduction of air is recorded symptoms zyrtec overdose cheap 8 mg coversyl amex. The use of an impedance meter for tympanometry and reflex measurements can be of great value medicine natural cheap coversyl online visa. Flight safety under these conditions is not impaired as long as it is made certain in each case that intelligibility of speech and perception of signals under background noise medications definitions coversyl 4mg low price, as well as hearing on the ground for briefing and check-list procedures is satisfactory (Annex 1, 6. Such a test can be performed under different conditions for reproducing or simulating flight deck noise: white noise, tape recordings in flight, flight simulators or flight tests may be used. A high noise level is not 10 Siegle otoscope: an otoscope with a bulb attachment by which the air pressure in the external auditory canal can varied. Voice communications between crew members in the cockpit including instructions and routine check-list operations must be clearly understood, also during approach, landing and emergency operations. It is complicated by acoustically significant differences in the use of earphones or overhead speakers for listening to R/T signals. Earphones are often not designed for hearing protection, thus little sound attenuation is provided. Whether earphones or loudspeakers are used on the flight deck, the signal-to-ambient noise ratio can be varied through volume control. An applicant who fails to pass the pure-tone audiometry test should not be declared unfit because of hearing loss, if his speech and signal perception have been demonstrated to be within acceptable limits at the appropriate masking noise level. The volume of the test material should be controllable by the applicant in a manner representative of the aircraft communication equipment. Head-shadow effects, brought about by the head in certain positions, cause poorer discrimination during monaural reception and might affect efficient communication between crew members and should be taken into account. The question of whether the affected individual is a pilot-in-command or co-pilot is relevant because of the seating arrangements. Monaural hearing in both private pilots and professional flight crews should therefore always be investigated and evaluated in accordance with best medical practice as well as assessed under 6. It should be noted that under the provisions of Annex 6, multi-crew aircraft are required to have intercom and radio equipment which can be effectively used in these cases. Here the auditory signals are picked up by a microphone placed beside the poor ear and shunted across, either electrically or acoustically, to the good ear. A non-occluding-type ear mould is used in the good ear which permits the direct reception of auditory stimuli in that ear. Persons fitted with this arrangement report a decided improvement in their ability to understand speech directed to their bad ear as well as some improvement in their ability to understand speech in noisy situations. The vast majority of individuals with sensorineural hearing impairment can gain significant improvement through the use of a wearable hearing aid. There are, however, quite a number of flight crew who can benefit, particularly socially, by an aid. When an applicant can communicate better with the hearing aid than without it, consideration should be given for its use for aviation duties on the ground. These carbon-type aids were responsible for the prevalent notion that only persons with conductive hearing loss could benefit from hearing aids. There was still much doubt concerning the efficiency of a hearing aid for the person with sensorineural hearing loss. The development of the transistor and the transistor hearing aids opened up a new era in design and fitting. By testing appropriately powered aids with frequency response characteristics deemed suitable for the particular hearing loss involved, it is often possible to demonstrate clear-cut and significant improvements in performance. In many instances, it may be necessary to test hearing-aid use in each ear separately and binaurally to determine the most appropriate fitting. Arguments against the use of hearing aids for licensing purposes centre around their delicate nature, their relatively low reliability, and their suboptimal acoustic performance. However, personal hearing aids are not normally required in flight because of the mandatory aircraft intercom and radio equipment. The best aids presently available provide a maximum of approximately 70 per cent of normal speech perception in environments of even relatively low ambient noise. The point is made that the use of hearing aids is by no means functionally analogous to the use of correcting lenses for a refractive error. Impairment of the sense of smell may cause the first faint odour of gas, oil or smoke to go unnoticed. A malfunctioning nose can cause serious problems in regard to aeration of the sinuses and the Eustachian tube with resultant middle ear pathology. In some cases, where the mucosa of the septum and the turbinates are swollen, it is impossible to examine it carefully unless a shrinking agent, such as neosynephrine or xylometazolin solution is used. Most examinees do not object to a flat pledget of cotton (soaked) placed in each nostril. The same is true with pressure over the anterior surface of the frontal or deep digital pressure over the floor of the frontal. This can be done by placing the finger under the superior bony rim of the orbit and having the examinee flex the head. It should be pointed out, however, that this technique may be misleading on account of the numbers of false positives and negatives found. This investigation can be done easily and requires only a dark room and any type of bright light. To examine the frontal sinuses place the light under the superior bony orbital rim and shield the light from your eyes. If one is clear and one fails to transmit light (remains dark) then the condition should be examined further. The maxillary sinuses are transilluminated in a similar manner, placing the light in the mouth, near the hard palate, with lips tightly closed. If the frontal and maxillary sinuses are all transilluminated clearly, do not assume that the examinee cannot have sinus trouble. The reason for this is that no one can transilluminate the sphenoid or ethmoid sinuses. The aviation examiner must, however, be alert, examine carefully, counsel and advise the examinee. There may be marked nasal obstruction, thick yellow discharge, cough and a slight temperature. Complications can occur in the paranasal sinuses, the Eustachian tube, the middle ear, larynx, trachea and bronchi. The common cold can be the direct cause of aerotitis media, inner ear barotrauma and of aerosinusitis. A careful pulmonary examination must be done where a definite allergic rhinitis is noted. Like aerotitis it is caused by pressure differences between the sinus and the ambient air. Any obstruction to drainage of the sinuses results in absorption of the oxygen, stagnation of the secretion in the sinus, followed by bacterial growth and the formation of pus. Like aerotitis, aerosinusitis usually develops during descent from higher altitudes. Aerosinusitis in the sphenoid gives rise to headache in the back of the head, whereas aerosinusitis located in the other sinuses gives pain near the sinus involved. One can assume that a pilot with the above symptoms is taking some form of medication. A husky, rough or croaking type of voice requires a thorough examination of the larynx. If further investigation is required, the pilot should be assessed as temporarily unfit. An acute laryngitis with hoarseness is frequently seen and will usually subside when the allied infection clears up. Smoking and excessive use of alcohol as well as tuberculosis and cancer are frequent aetiological factors. If a cancer is found, the pilot must receive proper treatment before being considered for certification. If treated with radiation, special attention must be paid to any post-radiation swelling in the larynx the following half year. Frequent moistening of the mouth becomes necessary, especially in the dry air of airliners. Distortion of the hair cells in the vestibular system sets up a chain of reflexes which produce postural, proprioceptive and oculomotor responses. They may accept these as normal or believe them to be symptoms of abnormality in themselves or in their aircraft. Whether they report disorientation, even under direct questioning, is influenced by: a) their recognition that they were disoriented; b) their ability to assess potential dangers in such episodes and their willingness to report them; c) social and economic pressures: 1) will their admission have desired consequences. When no true vertigo is present, the aetiology must be sought somewhere other than in the vestibular apparatus. One of these is rapid changes in altitude, which may produce pressure-induced vertigo, mainly during descent due to blockage and clearing of the middle ear. In general, pilots should be warned that disregarding the signs of a common cold and flying with an upper respiratory infection may result in acute incapacitation caused by pain in the ears or sinuses and, in some cases, an additional non-reversible vertigo and hearing loss which may lead to permanent grounding. The examiner should have the results of the cardiopulmonary evaluation; blood pressure determinations may lead to a diagnosis of orthostatic hypotension as the cause of dizziness. In patients with true vertigo and perceptive hearing loss, two sites of involvement must be suspected: the end organ and the eighth cranial nerve. Pure-tone audiometry, while able to distinguish conductive and sensorineural hearing losses, will not aid in this localization. The test is postivie when a patient, standing with feet approximated, becomes unsteady, or much more unsteady with eyes closed. Dix, English physician, and Charles Skinner Hallpike, English neuro-otologist (both 20th century). In the caloric test, the lateral semi-circular canal is stimulated by introducing fluid into the external auditory canal. If the fluid temperature differs from body temperature, the temperature difference will be conducted to a sector of the lateral semi-circular canal. Endolymph in this sector will differ in density from the remainder of the endolymph. If the plane of the semi-circular canal is aligned with gravity, this density difference will cause the endolymph to fall if the fluid is colder, or to rise if the fluid is warmer than body temperature. Since the caloric stimulus can produce a convection current which will rotate the endolymph in either direction, each ear can be tested independently. When cold (C) water is used, the resultant nystagmus is to the opposite (O) side; when warm (W) water is used, the nystagmus is to the same (S) side. One refers to nystagmus to the right or left according to the direction of the fast component. The speed of the slow component of the nystagmus and its direction are the parameters. A directional preponderance of less than 25 per cent is within accepted normal limits. This procedure is somewhat complicated and time-consuming for the non-specialist medical examiner. The test is an aviation relevant replacement of caloric testing and is the preferred test in several aviation medical centres in Contracting States. An observation of nystagmus reaction can easily vary from one observer to the next. This has made a comparison of results unsatisfactory unless the tests were consistently performed by the same person. Factors such as amplitude of nystagmus, maximum frequency and speed of the nystagmus beat could not be obtained with any accuracy. The movements of the eye which occur with nystagmus, cause the corneal-retinal potential to be displaced laterally, causing a recordable change in the potential at the outer canthus. The subject is placed recumbent with the head elevated 30 degrees, thus placing the horizontal canal in a position for maximum stimulation. Active electrodes are placed lateral to the outer canthus of the eye with the ground placed on the forehead; the eyes are closed to prevent fixation. The hot and cold caloric stimuli are applied and the induced nystagmus is automatically recorded by the electronic apparatus. The examiner should, however, know that these tests are available at aviation medical centres or in well-equipped otology clinics and audiology centres. In these it appears to concentrate where there are increased numbers of lymphocytes and monocytes in the fluid, as in genital inflammatory conditions.
Risk of complication from each type of procedure provides insight into the proper options for the patient treatment whiplash discount generic coversyl uk. The trial included conversion to laparotomy for the laparoscopic and vaginal groups as a major complication treatment quadricep strain buy coversyl 4mg visa. If you include conversion to laparotomy as a major complication treatment xerostomia 8 mg coversyl overnight delivery, the number treated relative to those harmed was 20 for the laparoscopic group compared with the abdominal group treatment improvement protocol generic coversyl 8mg without a prescription. If you exclude conversion to laparotomy as a complication symptoms testicular cancer purchase cheapest coversyl, then the complication rates are similar between all groups symptoms webmd quality 8mg coversyl. All six ureter injuries reported in this series occurred in the laparoscopic group. The overall lower urinary tract complication rate is three times higher with the laparoscopic group compared with vaginal or abdominal procedures. A minor complication, mostly postoperative fever or infection, occurred in approximately 25% of each group. Perioperative Checklist It is important to systematically go through a checklist of perioperative measures to effectively reduce potential complications (Table 24. If excessive blood loss is expected, intraoperative blood salvage techniques should be considered. All patients undergoing hysterectomy for benign disorders are at moderate risk for venous thromboembolism and require prophylaxis (18). Unfractionated heparin (5,000 U every 12 hours) or low molecular weight heparin. Patients on oral contraceptives up to the time of hysterectomy should be considered for pharmacologic treatment. Mechanical bowel preparation for prevention of infection complications from bowel injury is no longer recommended (46). Was the appropriate antibiotic selected according to American College of Obstetricians and Gynecologists guidelinesfi Document that prophylactic antibiotics will be discontinued within 24 hours after surgery. Technique Abdominal Hysterectomy General Preparation To reduce the colony count of skin bacteria, the patient is asked to shower. Hair surrounding the incision area may be removed at the time of surgery or before surgery using a depilatory agent. Hair clipping is preferable to shaving because it decreases the incidence of incisional infection, and if shaving is done, it should be performed in the operating room just prior to the surgery (34). Patient Positioning For most abdominal cases, the patient is placed in the dorsal supine position for the operation. After the patient is anesthetized adequately, her legs are placed in the stirrups and a pelvic examination is performed to validate the in-office pelvic examination findings. A Foley catheter is placed in the bladder, and the vagina is cleansed with an iodine solution. Skin Preparation Several methods for skin cleaning can be recommended, including a 5-minute iodine solution scrub followed by application of iodine solution, iodine solution scrub followed by alcohol with application of an iodine-impregnated occlusive drape, or an iodine-alcohol combination with or without application of an iodine-impregnated occlusive drape. Surgical Technique Incision the choice of incision should be determined by the following considerations: Simplicity of the incision Need for exposure Potential need for enlarging the incision Strength of the healed wound Cosmesis of the healed incision Location of previous surgical scars> the skin is opened with a scalpel, and the incision is carried down through the subcutaneous tissue and fascia. With traction applied to the lateral edges of the incision, the fascia is divided. This technique minimizes the possibility of inadvertent enterotomy, entering the abdominal cavity. Abdominal Exploration Cytologic sampling of the peritoneal cavity, if needed, should be performed before abdominal exploration. The liver, gallbladder, stomach, kidneys, para-aortic lymph nodes, and large and small bowel should be examined and palpated. Retractor Choice and Placement A variety of retractors were designed for pelvic surgery. The Bookwalter retractor has a variety of adjustable blades that can be helpful, particularly in obese patients. Elevation of the Uterus the uterus is elevated by placing broad ligament clamps at each cornu so that it crosses the round ligament. With the proximal portion held by the broad ligament clamp, the distal portion of the round ligament is ligated with a suture ligature or simply transected with Bovie cautery (Fig. The distal portion can be grasped with forceps, and the round ligament is cut to separate the anterior and posterior leaves of the broad ligament. The anterior leaf of the broad ligament is incised with Metzenbaum scissors or electrocautery along the vesicouterine fold, separating the peritoneal reflection of the bladder from the lower uterine segment (Fig. Care must be taken to remain lateral to both the infundibulopelvic ligament and iliac vessels. The external iliac artery courses along the medial aspect of the psoas muscle and is identified by bluntly dissecting the loose alveolar tissue overlying it. By following the artery cephalad to the bifurcation of the common iliac artery, the ureter is identified crossing the common iliac artery. The ureter should be left attached to the medial leaf of the broad ligament to protect its blood supply (Fig. With the ureter under direct visualization, a window is created in the peritoneum of the posterior leaf of the broad ligament under the utero-ovarian ligament and fallopian tube. The tube and utero-ovarian ligament are clamped on each side with a curved Heaney or Ballantine clamp, cut, and ligated with both a free-tie and a suture ligature. The medial clamp at the uterine cornu should control back bleeding; if it does not, the clamp should be repositioned to do so (Fig. This opening allows proper exposure of the uterine artery, the ovarian vessels, and the ureter. In this manner, the ureter is released from its proximity to the uterine vessels and uterine vessels. Alternatively, free ties can be passed around the uterine vessels, two cephalad and one caudad, before they are cut. An avascular plane, which exists between the lower uterine segment and the bladder, allows for this mobilization. Tonsil clamps may be placed on the bladder edge to provide countertraction and easier dissection (Fig. Care is taken to place the tip of the clamp adjacent to the uterus at this anatomic narrowing. A relatively avascular tissue plane exists in this area, allowing mobilization of the rectum inferiorly out of the operative field. This step is repeated on each side until the junction of the cervix and vagina is reached (Fig. Curved Heaney clamps are placed bilaterally, incorporating the uterosacral ligament and upper vagina just below the cervix. The pedicles are sutured with a Heaney stitch, incorporating the uterosacral and cardinal ligament at the angle of the vagina (Fig. Meticulous hemostasis in the pelvis, particularly of the vascular pedicles, should be ensured. Ureteral position and integrity are checked to ensure that they are intact and do not appear dilated. Research using animal models suggests that reapproximation may increase tissue trauma and promote adhesion formation (47). Fascia can be closed with an interrupted or continuous 0 or 1 monofilament absorbable suture. A prospective randomized trial did not show any advantage of interrupted versus continuous fascial closure (48). Bites should be taken about 1 cm from the cut edge of the fascia and about 1 cm apart to prevent wound dehiscence. Skin Closure the subcutaneous tissue should be irrigated, with careful hemostasis. Wound disruption seems to be decreased with closure of the subcutaneous fat layer in women with 2 cm or more fat (49). Intraoperative Complications Every surgeon must be prepared to recognize and repair operative injuries, because despite a high level of attention to detail, injuries and complications, recognized and unrecognized, can still occur. Ureteral Injuries Injury to the pelvic ureter is one of the most formidable complications of hysterectomy (50). It is always essential to be aware of the proximity of the ureter to the other pelvic structures. Most ureteral injuries can be avoided by opening the retroperitoneum and directly identifying the ureter. The use of ureteral catheters as a substitute for direct visualization is often of little help in patients with extensive fibrosis or scarring resulting from endometriosis, pelvic inflammatory disease, or ovarian cancer. In these instances, a false sense of security may increase an already high risk for ureteral injury. The use of ureteral catheters are associated with hematuria and acute urinary retention, although their complications are usually transitory in nature. Direct visualization is accomplished by opening the retroperitoneum lateral to the external iliac artery. Blunt dissection of the loose areolar tissue is performed to visualize the artery directly. The artery may be traced cephalad to the bifurcation of the internal and external iliac arteries. The ureter crosses the common iliac artery at its bifurcation and may be followed throughout its course in the pelvis. Prompt consultation is necessary if the surgeon is not trained in ureteral repair. If a ureteral obstruction is suspected, confirmation may be obtained by intravenous injection of 1 ampule of indigo carmine dye and performance of a cystoscopic evaluation. The integrity of the ureters should be confirmed by the presence or absence of bilateral spill of tinted urine. Bladder Injury Because of the close anatomic relationship of the bladder, uterus, and upper vagina, the bladder is the segment of the lower urinary tract that is most vulnerable to injury. Bladder injury may occur on opening the peritoneum or, more frequently, during the dissection of the bladder off the cervix and upper vagina. Unless there is involvement of the bladder trigone, a bladder laceration is easily repaired. In the nonirradiated bladder, a oneor two-layer closure with a small-caliber braided absorbable suture such as a 3-0 polyglycolic acid is adequate. If the bladder is not compromised, drainage should be continued at least until gross hematuria clears, which may occur as soon as 48 hours postoperatively. A more conservative practice is to continue drainage for 3 to 14 days depending on the type of injury (50). If the trigone is involved, a surgeon trained in complicated urologic repair should be consulted, because reimplantation of the ureter may be necessary. Bowel Injury Small bowel injuries are the most common intestinal injuries in gynecologic surgery. Small defects of the serosa or muscularis may be repaired using a single layer of continuous or interrupted 3-0 braided absorbable suture. Although single-layer closure of the small bowel has proved adequate, it is safer to close defects involving the lumen in two layers using a 3-0 braided absorbable suture. Because the bacterial flora of the ascending colon is similar to that of the small bowel, injuries can be repaired in a similar manner. The transverse colon rarely is injured in normal gynecologic procedures because it is well outside the operative field. However, the descending colon and the rectosigmoid colon are intimately involved with the pelvic structures and are at significant risk for injury during gynecologic surgery. Injuries not involving the mucosa may be repaired with a single running layer of 2-0 or 3-0 braided absorbable suture. If the laceration involves the mucosa, it may be closed as with small bowel injuries. Hemorrhage Significant arterial bleeding usually arises from the uterine arteries or the ovarian vessels near the insertion of the infundibulopelvic ligaments. Blind clamping of these vessels presents a risk for ureteral injury; therefore, the ureters should be identified in the retroperitoneal space and traced to the area of bleeding to avoid inadvertent ligation. It is best to apply a pressure pack to tamponade the bleeding and slowly remove the pack in an effort to visualize, isolate, and individually clamp the bleeding vessels. Venous bleeding is less dramatic but often is more difficult to manage, particularly in the presence of extensive adhesions and fibroids. This type of bleeding can be controlled with pressure alone or with suture ligation. Bleeding from peritoneal edges or denuded surfaces may be controlled with pressure, application of topical agents such as thrombin or collagen, or Bovie cautery. A variety of laser techniques are used to control bleeding, such as the use of the Argon beam laser. An indwelling bladder catheter should be used for the first few postoperative hours until the patient is able to ambulate and urinate. If retropubic urethropexy was performed, a suprapubic catheter, which allows postvoid residual levels to be checked without repetitive catheterizations, can be considered. This catheter may be removed when satisfactory postvoid residual levels of less than 100 mL are obtained. Diet As soon as the patient is alert, diet is resumed, offering solid foods as tolerated with return of appetite. This dietary regimen assumes minimal intraoperative bowel manipulation and dissection. Early postoperative feeding was shown to be safe and to speed return of bowel function and recovery.
Of reported outbreaks medications knee best buy coversyl, 60% involved the intestinal tract medications names cheap coversyl 8 mg on line, 18% were dermatologic medicine used for anxiety order coversyl 4 mg, and 18% involved the respiratory tract medicine used to induce labor buy coversyl 4mg fast delivery. Recommendations for prevention of diseases transmitted by animals have been updated in the Diseases Transmitted by Animals (Zoonoses) section to include a mnemonic for appropriate pet selection from the Black Pine Animal Park symptoms 10 days before period buy coversyl 8mg. Updates on epidemic strains symptoms 5 days post embryo transfer buy coversyl with mastercard, outbreaks in specifc situations, guidelines for outbreak management and disease prevention, and diagnostic testing have been added. Valganciclovir administered orally to young infants provides a therapeutic option for treatment of infants with symptomatic congenital cytomegalovirus infection involving the central nervous system. Recommendations have been updated to include new vaccines, an algorithm recommending an approach to immunization of children with egg allergy has been added, and the current status of antiviral recommendations has been updated. The postexposure prophylaxis regimen of rabies vaccine has been reduced from 5 to 4 doses given at 0, 3, 7, and 14 days following exposure. Changes to management of newborn infants include use of lumbar puncture in infants who have signs of sepsis, change in use of intrapartum prophylaxis and inclusion of a revised algorithm for management of newborn infants with possible risk of early-onset group B streptococcal disease. Isoniazid and rifapentine, a long-acting rifamycin, have been added, but because evaluation in children younger than 13 years of age has been limited, this therapeutic option is not recommended for this age group. The Drugs for Parasitic Infections section is reproduced with permission from the 2010 edition of the Medical Letter. The advent of population-based postlicensure studies of new vaccines facilitates detection of rare adverse events temporally associated with immunization that were undetected during prelicensure clinical trials. Physicians must regularly update their knowledge about specifc vaccines, including information about their recommended use, safety, and effectiveness. Each edition of the Red Book provides recommendations for immunization of infants, children, and adolescents. Whereas immunization recommendations represent the best approach to disease prevention on a population basis, in rare circumstances, individual considerations may warrant a different approach. Comparison of 20th Century Annual Morbidity and Current Morbidity: Vaccine-Preventable Diseasesa 20th Century 2010 Reported Percent Disease Annual Morbidityb Casesc Decrease Smallpox 29 005 0 100 Diphtheria 21 053 0 100 Measles 530 217 63 >99 Mumps 162 344 2612 98 Pertussis 200 752 27 550 86 Polio (paralytic) 16 316 0 100 Rubella 47 745 5 >99 Congenital rubella syndrome 152 0 100 Tetanus 580 26 96 Haemophilus infuenzae 20 000 246d 99 a National Center for Immunization and Respiratory Diseases. Health care professionals should be familiar with the label for each product they administer. Most manufacturers maintain Web sites with current information concerning new vaccine releases and changes in labeling. Annual course offerings include the Immunization Update, Vaccines for International Travel, Infuenza, and a 9-module introductory course on the Epidemiology and Prevention of Vaccine-Preventable Diseases. The course schedule, slide sets, and written materials can be accessed online ( Appendix I (p 883) provides a list of reliable immunization information resources, including facts concerning vaccine effcacy, clinical applications, schedules, and unbiased information about safety. Two resources comprehensively address concerns of practicing physicians: the National Network for Immunization Information ( Information regarding global health matters can be obtained from the World Health Organization ( The schedulers, which can be downloaded, allow the user to determine vaccines needed by age and are useful for viewing missed or skipped vaccines quickly according to the recommended childhood and adult immunization schedules. Questions should be encouraged, and adequate time should be allowed so that information is understood ( This applies in all settings, including clinics, offces, hospitals (eg, for the birth dose of hepatitis B vaccine), and pharmacies. Health care professionals also should be aware of local confdentiality laws involving adolescents. Health care professionals always should provide factual information and use language appropriate for parents and other care providers. Pediatricians and nurses should discuss benefts and risks of each vaccine, because a parent who is reluctant to accept administration of 1 vaccine may be willing to accept others. Active Immunization Active immunization involves administration of all or part of a microorganism or a modifed product of a microorganism (eg, a toxoid, a purifed antigen, or an antigen produced by genetic engineering) to evoke an immunologic response that mimics that of natural infection but usually presents little or no risk to the recipient. Some immunizing agents provide nearly complete and lifelong protection against disease, some provide partial protection, and some must be readministered at regular intervals to maintain protection. Vaccines incorporating an intact infectious agent may contain live-attenuated, inactivated, or genetically engineered subunits. Among currently licensed vaccines in the United States, there are 2 live-attenuated bacterial vaccines (oral typhoid and bacille-Calmette Guerin vaccines) and several live-attenuated viral vaccines. Although active replication (with bacterial or viral replication) ensues after administration of these vaccines, infection is modifed, and little or no adverse host effect is expected. Maintenance of long-lasting immunity with inactivated viral or bacterial vaccines and toxoid vaccines may require periodic administration of booster doses. Although inactivated vaccines may not elicit the range of immunologic response provided by live-attenuated agents, effcacy of licensed inactivated vaccines is high. Bacterial polysaccharide conjugate vaccines (eg, Haemophilus infuenzae type b and pneumococcal conjugate vaccines) reduce nasopharyngeal colonization through exudated IgG. Viruses and bacteria in inactivated vaccines cannot replicate in or be excreted by the vaccine recipient as infectious agents and, thus, do not present the same safety concerns for immunosuppressed vaccinees or contacts of vaccinees as might live-attenuated vaccines. Adherence to recommended guidelines is critical to the success of immunization practices. Some vaccines consist of a single antigen that is a highly defned constituent (eg, tetanus or diphtheria toxoid). Carrier proteins of proven immunologic potential (eg, tetanus toxoid, nontoxic variant of diphtheria toxin, meningococcal outer membrane protein complex), when chemically bound to less immunogenic polysaccharide antigens (eg, H infuenzae type b, meningococcal and pneumococcal polysaccharides), enhance the type and magnitude of immune responses, particularly in children younger than 2 years of age, who have immature immune systems. Some vaccine products use a complex tissueculture fuid, which may contain proteins or other constituents derived from the medium and biological system in which the vaccine is produced (eg, egg antigens, gelatin, or cell culture-derived antigens). Vaccine Handling and Storage Vaccines should be transported and stored at recommended temperatures. Some products may show physical evidence of altered integrity, and others may retain their normal appearance despite a loss of potency. The following guidelines are suggested as part of a quality-control system for safe handling and storage of vaccines in an offce or clinic setting. Assign a backup person to assume these responsibilities during times of illness or vacation. The details of proper storage conditions should be posted on or near each refrigerator or freezer used for vaccine storage or should be readily available to staff. Receptionists, mail clerks, and other staff members who may receive shipments also should be educated. Use plug guards and warning signs to prevent accidental dislodging of the wall plug. The current temperature log should be posted on the door to remind staff to monitor and record temperatures. All reconstituted vaccines should be refrigerated during the interval in which they may be used. Offce personnel need to be aware of alternate storage sites and trained in the correct techniques to store and transport vaccines to avoid warming vaccines that need to be refrigerated or frozen and to avoid freezing vaccines that should be refrigerated. Changing needles between drawing a vaccine into a syringe and injecting it into the child is not necessary. Facilities and personnel should be available for treating immediate allergic reactions. This vaccine is licensed for healthy, nonpregnant people 2 through 49 years of age. However, if clinical judgment indicates that nasal congestion might impede delivery of the vaccine to the nasopharyngeal mucosa, vaccine deferral should be considered until resolution of the illness. The recommended route is based on studies designed to demonstrate maximum safety and immunogenicity. Ordinarily, the upper, outer aspect of the buttocks should not be used for active immunization, because the gluteal region is covered by a signifcant layer of subcutaneous fat and because of the possibility of damaging the sciatic nerve. The site selected should be well 1 For a review on intramuscular injections, see Centers for Disease Control and Prevention. Aspiration before injection of vaccines or toxoids (ie, pulling back on the syringe plunger after needle insertion, before injection) is not recommended, because no large blood vessels are located at the preferred injection sites, and the process of aspiration has been demonstrated to increase pain. Techniques for minimizing pain can be divided into physical, psychological, and pharmacologic. Stroking or rocking a child after an injection decreases crying and other pain behaviors. With parenterally administered live-virus vaccines, the inhibitory effect of residual specifc maternal antibody determines the optimal age of administration. An additional factor in selecting an immunization schedule is the need to achieve a uniform and regular response. For example, live-virus rubella vaccine evokes a predictable response at high rates after a single dose. With many inactivated or component vaccines, a primary series of doses is necessary to achieve an optimal initial response in recipients. For example, some people respond only to 1 or 2 types of poliovirus after a single dose of poliovirus vaccine, so multiple doses are given to produce antibody against all 3 types, thereby ensuring complete protection for the person and maximum response rates for the population. No minimum interval is required between administration of different inactivated vaccines. The recommended childhood (0 through 6 years of age), adolescent (7 through 18 years of age), and catch-up immunization schedules in Fig 1. The use of a combination vaccine generally is preferred over separate injections of its equivalent component vaccines. Considerations should include provider assessment, patient preference, and the potential for adverse events. The provider assess ment should include the number of injections, vaccine availability, the likelihood of improved coverage, the likelihood of patient return, and storage and cost considerations. Web-based childhood immunization schedulers using the current vaccine recommendations are available for parents, caregivers, and health care profes sionals to make instant immunization schedules for children, adolescents, and adults (see Immunization Schedulers, p 5, or For children in whom early or rapid immunization is urgent or for children not immunized on schedule, simultaneous immunization with multiple products allows for more rapid protection. In many instances, the guidelines will be applicable to children in other countries, but individual pediatricians and recommending committees in each country are responsible for determining the appropriateness of the recommendations for their setting. Studies have demonstrated that the recommended age and interval between doses of the same antigen(s) provide optimal protection. In these cases, an accelerated schedule using minimum age or interval criteria can be used. Vaccines should not be administered at intervals less than the recommended minimum or at an earlier age than the recommended minimum (eg, accelerated schedules). A third dose of a measles-containing vaccine is indicated at 4 through 6 years of age but can be administered as early as 4 weeks after the second dose (see Measles, p 489). Although immunizations should not be scheduled at an interval or age less than the minimums listed in Fig 1. If the child is known to the clinician, rescheduling the child for immunization closer to the recommended interval is preferred. If the parent or child is not known to the clinician or follow-up cannot be ensured (eg, habitually misses appointments), administration of the vaccine at that visit rather than rescheduling the child for a later visit is preferable. Vaccine doses administered 4 days or fewer before the minimum interval or age can be counted as valid. This 4-day recommendation does not apply to rabies vaccine because of the unique schedule for this vaccine. Doses administered 5 days or more before the minimum interval or age should not be counted as valid doses and should be repeated as age appropriate. Immune response to one vaccine generally does not interfere with responses to other vaccines. When vaccines are administered simultaneously, 1 separate syringes and separate sites should be used, and injections into the same extremity should be separated by at least 1 inch so that any local reactions can be differentiated. Some vaccines administered simultaneously may be more reactogenic than others (see disease-specifc chapters). Health care professionals who provide immunizations should stock combination and monovalent vaccines needed to immunize children against all diseases for which vaccines are recommended, but all available types or brand-name products do not need to be stocked. It is recognized that the decision of health care professionals to implement use of new combination vaccines involve complex economic and logistical considerations. When patients have received the recommended immunizations for some of the components in a combination vaccine, administering the extra antigen(s) in the combination vaccine is permissible if they are not contraindicated and doing so will reduce the number of injections required. Lapsed Immunizations A lapse in the immunization schedule does not require reinitiation of the entire series or addition of doses to the series for any vaccine in the recommended schedule. If a dose of vaccine is missed, subsequent immunizations should be given at the next visit as if the usual interval had elapsed.
Coversyl 4mg generic. Comprehensive Care Flu Prevention.