Marc Klapholz, MD
- Department of Medicine
- Division of Cardiology
- UMDNJ-New Jersey Medical School
- Newark, NJ
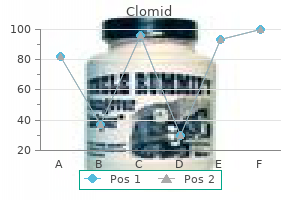
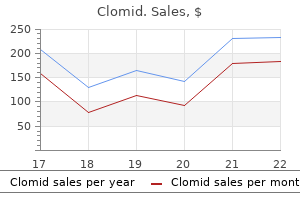
Pressing the plum-colored activator button will release the medicine from the Pen women's health center queens hospital buy clomid on line amex. Squeeze the area of the cleaned skin and hold it firmly until the injection is complete women's health issues endometriosis order generic clomid on-line. Place the white end of the Pen straight (at a 90º angle) and flat against the raised area of your skin that you are squeezing women's health clinic enterprise al cheap 100 mg clomid with visa. Place the Pen so that it will not inject the needle into your fingers that are holding the raised skin womens health 30s buy genuine clomid on line. Keep pushing the Pen against the squeezed pregnancy 9 weeks symptoms generic 50mg clomid visa, raised skin of your injection site for the whole time so you get the full dose of medicine breast cancer in men statistics buy clomid 25mg on line. There may be state or local laws about how you should throw away used needles and syringes. Important Information You Need to Know Before Injecting Humira Do not use the Pen and call your healthcare provider or pharmacist if:. Liquid has been frozen (even if thawed) or or particles in it left in direct sunlight. The Pen has been dropped or crushed Keep the caps on until right before injection. Different from your last injection site Wipe the injection site in a circular motion with the alcohol swab. Squeeze the skin at your injection site to make a raised area and hold it firmly until the injection is complete. It is important that you firmly push the Pen down all the way against the injection site before starting the injection. Keep pushing down to prevent the Pen from moving away from the skin during the injection. After completing the injection, place a cotton ball or gauze pad on the skin of the injection site. Do not throw away (dispose of) loose needles, syringes, and the Pen in the household trash. There may be state or local laws about how you should throw away used needles and syringes. The Pen caps, alcohol swab, cotton ball or gauze pad, dose tray, and packaging may be placed in your household trash. This takes up to 10 seconds What should I do if there are more than a few drops of liquid on the injection site? Important Information You Need to Know Before Injecting Humira Do not use the Pen and call your healthcare provider or pharmacist if:. Liquid has been frozen (even if thawed) or particles in it left in direct sunlight. The Pen has been dropped or crushed Keep the caps on until right before injection. Do not use the Pen if liquid has been frozen (even if thawed) Check expiration date on the Pen label. Different from your last injection site Wipe the injection site in a circular motion with the alcohol swab. Squeeze the skin at your injection site to make a raised area and hold it firmly until the injection is complete. It is important that you firmly push the Pen down all the way against the injection site before starting the injection. After completing the injection, place a cotton ball or gauze pad on the skin of the injection site. Do not throw away (dispose of) loose needles, syringes, and the Pen in the household trash. There may be state or local laws about how you should throw away used needles and syringes. The Pen caps, alcohol swab, cotton ball or gauze pad, dose tray, and packaging may be placed in your household trash. This takes up to 15 seconds What should I do if there are more than a few drops of liquid on the injection site? If you do not have all the supplies you need to give yourself an injection, go to a pharmacy or call your pharmacist. If you choose your abdomen, do not use the area 2 inches around your belly button (navel. Look closely to make sure that the amount of liquid in the syringe is the same or close to the:. If the syringe does not have the correct amount of liquid, do not use that syringe. Turn the syringe so the needle is facing up and hold the syringe at eye level with one hand so you can see the air in the syringe. Using your other hand, slowly push the plunger in to push the air out through the needle. Hold the body of the prefilled syringe in one hand between the thumb and index finger. Using a quick, dart-like motion, insert the needle into the squeezed skin at about a 45-degree angle. Slowly push the plunger all the way in until all the liquid is injected and the syringe is empty. Throw away the used prefilled syringe and needle in a sharps disposal container right away after use. Do not throw away (dispose of) loose needles and syringes in your household trash. There may be state or local laws about how you should throw away used needles and syringes. Important Information You Need to Know Before Injecting Humira Do not use the prefilled syringe and call your healthcare provider or pharmacist if:. Liquid has been frozen (even if thawed) or or particles in it left in direct sunlight. The prefilled syringe has been dropped or crushed Keep the needle cover on until right before injection. See Step 9at the end of this Instructions for Use for instructions on how to throw away (dispose of) your prefilled syringe Wash and dry your hands. Different from your last injection site Wipe the injection site in a circular motion with the alcohol swab. Hold the body of the prefilled syringe in one hand between the thumb and index fingers. Gently squeeze the area of cleaned skin at your injection site with your other hand. Insert the needle into the skin at about a 45 degree angle using a quick, dart-like motion. Slowly push the plunger all the way in until all of the liquid is injected and the prefilled syringe is empty. When the injection is completed, slowly pull the needle out of the skin while keeping the prefilled syringe at the same angle. After completing the injection, place a cotton ball or gauze pad on the skin of the injection site. There may be state or local laws about how you should throw away used needles and syringes. The needle cover, alcohol swab, cotton ball or gauze pad, dose tray, and packaging may be placed in your household trash. Necrotizing fasciitis: a fourteen-year retrospective study of 163 consecutive patients. Diabetes present in 18 60% >50% cases in healthy individuals 1Bellapianta, Joseph M. Pain Triad of = High Skin Changes Suspicion Rapid Progression Necrotizing Soft Tissue Infections Progression. Necrotizing Soft Tissue Infections Bacteriology Streptococcal Group A strep (Strep. Short incubation period Necrotizing Soft Tissue Infections Bacteriology Clostridial species a. Necrotizing fasciitis Necrotizing Soft Tissue Infections Bacteriology Others – high-risk for unusual or resistant pathogens a. Zimbelman J Ped Infect Dis J 1999; 18:1096-1100 Protein synthesis-inhibiting antibiotics. Shown to decrease production of toxins, superantigens, and enzymes from: Gram positive: – S. Streptococcal toxic shock syndrome presenting as septic knee arthritis in a 5-year-old child. Successful treatment of severe streptococcal toxic shock syndrome with a combination of intravenous immunoglobulin, dexamethasone and antibiotics. Toxic shock syndrome following thoracic surgery for lung cancer: report of a case. Given a patients clinical presentation and risk factors, They are then further classifed into three subcategories: distinguish between the various types of skin and sof mild, moderate, and severe. Given a patients profle, develop a pharmacotherapeutic tions are associated with systemic signs of infection such plan to treat a skin or sof tissue infection. Justify prevention measures to reduce the recurrence deeper infection, or infection that fails to improve with and transmission of a patients skin and sof tissue incision and drainage (I&D) plus oral antibiotics are also infections. Purulent infections are treated with I&D and antibiotic administration in moderate and Introduction severe cases. Some cases are caused by viruses— most classifed into two categories: purulent infections (e. Such damage is more complicated in patients with T erefore, careful assessment of risk factors and degree diabetes because long-term hyperglycemia leads to motor of severity, as well as obtaining a detailed medical history and autonomic neuropathy, cellular and humoral immu and performing a physical examination are required to nopathy, and angiopathy. Antimicrobial regimens are ofen selected matory response associated with herpes zoster. Antimicrobial stewardship, infection control, and prevention options are also discussed. Skin and sof tissue infections also accounted for 500,000 hospital discharges, or 1. They are ofen resistant to tact, and crowded living conditions facilitate the spread of older, non-β-lactam antibiotics (Herman 2008. Peripheral vascular disease and pre-existing Infected dog and cat bite wounds are polymicrobial, skin diseases increase the risk of erysipelas and cellulitis. Infected human bite wounds are Streptococcus pyogenes on the skin increases the risk of also polymicrobial, with Streptococcus spp. Infection with streptococci and Herpes zoster is associated with advanced age and staphylococci can occur simultaneously, and infection immunosuppressive conditions. Table 1-1 lists dosing regimens in intravenous nafcillin, cefazolin, or clindamycin is rec adults and children, adverse efects, and signifcant drug ommended in severe cases (Singer 2014; Stevens 2014; interactions for common antibiotics used in the treatment Forcade 2012. In all cases, application of warm moist compresses Severe purulent infections are treated with I&D and an facilitates pus elimination. Recurrent abscesses should initial course of intravenous antibiotics followed by oral be drained, cultured, and treated for 5–10 days with antibiotics when appropriate. A Mild nonpurulent infections are treated with oral anti decolonization regimen with mupirocin intranasally biotics. Moderate nonpurulent infections are treated twice daily for 5 days, chlorhexidine washes daily, and with an initial course of intravenous antibiotics followed decontamination of personal items should be consid by oral antibiotics when appropriate. The goals of therapy for herpes zoster are to alleviate signs and symptoms and avoid complications. Table 1-2 lists dosing regimens in adults, ized by multiple erythematous, vesicular, and pruritic adverse efects, and signifcant drug interactions for anti lesions on the face and the extremities. Bullous impetigo presents with vesicles that Infections in the Outpatient Seting develop into yellow fuid-flled bullae that rupture, leav Folliculitis, Furuncles, Carbuncles, ing brown crusts. Rarely, streptococcal impetigo leads to and Cutaneous Abscesses Continued on page 10 Folliculitis is an infection of one or more hair folli cles that may afect any area of the body (excepting the palms and soles, where there is no hair. Conditions in Which Antibiotic T erapy is red dot that ultimately becomes a white tip, and it may Recommended Afer Incision and Drainage be associated with rash or pruritus. Abscess in area difcult to drain completely than folliculitis and result in painful swollen boils on the. Associated septic phlebitis furuncles and have openings that drain pus; they are ofen. Clinical practice guidelines by In mild cases, I&D is recommended without systemic the Infectious Diseases Society of America for the treatment of antibiotic therapy. Conditions for which antibiotic methicillin-resistant Staphylococcus aureus infections in adults therapy is recommended after I&D are summarized and children. General approach to the management of acute bacterial skin and skin structure infections. Practice guidelines for the diagnosis and management of skin and sof tissue infections: 2014 update by the Infectious Diseases Society of America. Practice guidelines for the diagnosis and management of skin and soft tissue infections: 2014 update by the Infectious Diseases Society of America. Clinical practice guidelines by the Infectious Diseases Society of America for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Continued fom page 6 complications such as acute rheumatic fever and glomer obtained. Diagnosis of impetigo is based on clinical presence of damage to surrounding or underlying struc presentation. Patients may also present with enlargement of the is reasonable in typical cases (Stevens 2014. Gram stain and culture are usually not performed on bullous impetigo is topical mupirocin or retapamulin wounds.
A cross cultural study of vaginal practices and sexuality: implications 1Department of Psychology pregnancy urine clomid 25mg without prescription, University of Guelph women's health center fort wayne best clomid 25mg, 50 Stone Road E womens health foundation buy cheap clomid 25 mg on-line, Guelph women's health stomach problems buy generic clomid 50 mg line, 2 for sexual health pelvic floor disorders women's health issues order generic clomid. J Infect Gynecology womens health vest clomid 50 mg line, Faculty of Medicine, University of British Columbia, 2329 West Dis. Vaginal lactobacilli, microbial flora, and risk of human immunodeficiency virus type Received: 16 October 2015 Accepted: 14 March 2018 1 and sexually transmitted disease acquisition. Vaginal microbiome and epithelial gene array in post-menopausal of bacterial vaginosis-associated microorganisms in endometritis. Characterization of the vaginal microbiota of healthy Canadian women through the menstrual cycle. Resolution and characterization of distinct cpn60-based subgroups of Gardeneralla vaginalis in the vaginal microbiota. Its associated with significant morbidity, affecting the the Aga Khan University, Kenya womans quality of life as well as sexual function. Majority of the patients Obstetrics and Gynaecology, Honorary Faculty, the Aga are healthy, immunocompetent and have no discernible predisposing or Khan University, Nairobi. There are controversies regarding the identified risk factors, with some studies showing an association and others not. Successful treatment may be achieved with oral or topical agents, which are equally effective. Repeated treatment might select and induce drug resistance and a shift toward more resistant Candida species, as well as lead to non-compliance with treatment. It is often over-diagnosed or misdiagnosed, leading to inappropriate treatment especially in resource-constrained developing countries. It is the second most common cause of Table 1: Classification of Genital Candidiasis. It is classified Host Normal diabetes mellitus) as uncomplicated and complicated, which is now internationally the primary pathology in genital candidiasis is inflammation of accepted [7,8]. It is also classified as sporadic (acute) and recurrent the vulva and vagina secondary to an overgrowth of Candida. Many women self-diagnose and treat with reservoir or the partners genitalia [3,4,30]. Alteration of the vaginal ecosystem in certain conditions, of multiple interacting factors [41]. Likewise wearing of tight-fitting clothes, non-cotton underwears, panty this remains controversial and unresolved. Whereas high liners and hoses have been reported to increase local genital oestrogen contraceptives have been shown to increase the risk of temperature, humidity and moisture, thus increasing the risk genital candidiasis, [45,46], similar effects have also been shown of genital candidiasis [52,62]. However a study involving sexually active college students failed to show increased prevalence of symptomatic the role of sexual activity per se and various sexual practices candidiasis among those using oral pills, diaphragms, condoms, in the pathogenesis of genital candidiasis has attracted a lot of or spermicides [5]. The possibility of sexual transmission of Candida during the associated high concentration of reproductive hormones penile-vaginal intercourse has been based on the fact that male especially oestrogen in pregnancy increases the glycogen partners of infected women are four times more likely to be content in the vaginal epithelial cells, which increases the risk colonized by Candida on their genitalia than those of uninfected of colonization and symptomatic candidiasis [49,50]. Of course the question would be that vaginal colonization with Candida was a risk factor for what came first, i. However, in a more recent study, Muznyl this is an area that has elicited a lot of interest and concerns, et al. Its been in the last six months [70], sex during menses [69], receptive reported that 28-33% of women put on antibiotic therapy develop oral and anal intercourse [61,71,72] and frequency of vaginal symptomatic genital candidiasis [54,56]. However antibiotic therapy, even intense therapy thereof, is not associated other studies did not find evidence to support the role of sugar with an increased risk of developing symptoms [51]. While deficiencies of minerals such as magnesium, zinc, calcium and iron have been Sexual and behavioural factors associated with genital candidiasis in some studies, the evidence Female genital hygiene habits and practices such as douching, thereto is considered insufficient [79]. The vaginal discharge varies in amount and contribute to a prolongation and recurrence of genital candidiasis consistency from watery to homogenously thick – what is referred [84]. In support thereof a few studies have shown benefits from to as cottage-cheese like or curd-like and does not have an desensitization using Candida antigens [87], and clinical response offensive smell [19,79]. More than 50% of women with symptoms and signs suggestive glabrata which is less susceptible to the azole antifungal agents of genital candidiasis self-reporting may have other conditions [89]. This simple test can promptly exclude organisms is considered a major factor in its virulence [93]. There have been concerns that exclude other conditions such as bacterial vaginosis (clue the repeated treatment might induce drug resistance, as well cells) and trichomoniasis (trichomonads. Have symptom and signs suggestive of genital candidiasis, of non-albicans Candida with increasing age of the woman [100]. Have positive microscopy but fail to respond to the standard A) Induction therapy therapy i. Fluconazole – 150 mg orally in three doses given every 72 these media do not discriminate among the Candida spp. Thus hours[115,117], or because of the relatively high possibility of non-albicans Candida ii. For azole resistant Candida spp, means to detect Candida and differentiate between C. D) Maintenance therapy: F) Other tests: Susceptibility tests are considered most helpful in patients previously treated with an azole when there i. Fluconazole 150mg orally weekly for 6 months [115], or is a possibility of antifungal resistance. Clotrimazole cream 200mg twice weekly or 500mg weekly considered routine procedures and are not easily available. For non-albicans or azole resistant Candida albicans spp and specificity and a shorter turn-around time in comparison to v. Boric acid 600mg vaginally once or twice weekly for 6 current microscopy and culture techniques. However they are not months, or easily available as a diagnostic test and not considered clinically useful [114]. Flucytosine 17% cream vaginally either alone or in positive in 25% of patients with culture-positive symptomatic combination with 3% Amphotericin cream daily for 6 genital candidiasis [3]. Antigen detection and serologic tests are months [3,13,111], or not reliable and not clinically useful [3]. Gentian Violet 1% weekly for 4-6 months in combination Treatment with topical nystatin or Boric acid [13]. In case of recurrence after maintenance regimen each subsequent episode should be treated independently I. If recurrence is established those not reversible induction and maintenance regimens should be instituted. Prevention of repeat episodes E) Alternative treatment: Once and if potential risk factors are identified, the patient and a) Use of probiotics – There are anecdotal reports of benefits. The vaginal environment can be altered by changing the b) Zafirlukast 20 mg twice daily for 6 months [88] may be contraception to depot-medroxyprogesterone acetate [50]. The principle of therapy involves an induction regimen to Abnormal vaginal discharge and vulvar pruritus are two ensure clinical remission, followed immediately by a maintenance very common complaints for which women present to health regimen [3,115,116]. It is prevalent during the turn lead to increased local viral replication [127,128]. Whereas it is said to be very common the actual magnitude [132] reported that these patients have higher frequency of C. There is also higher diversity of non-albicans contended that these are higher than the true magnitude of the Candida spp [38]. If that is true, there with a number of factors acting synergistically to facilitate and is an urgent need to include in the preventive strategies screening enhance Candida overgrowth, leading to clinical symptoms. However, definitive prophylaxis with fluconazole; the question therefore is whether evidence relating to each of these factors is limited [7,78]. Studies have indicated that oral sex performed were Candida culture positive [109]. This is indeed a big challenge by the male partner (cunnilingus) is associated with both incident and of major concerns for the developing countries, as laboratory and recurrent candidiasis [65,69]. They however did not report on the recommended regimens including induction therapy at times actual practice these women did with each other! Indeed Reed [78] up to two weeks followed by maintenance therapy for up to six had suggested that it is the sexual behaviours rather the presence months, which have been supported by randomized clinical trials of Candida spp at various body locations of the male partners [115], have numerous challenges. The repeated treatments may that are associated with recurrences of genital candidiasis [78]. The same has young partners sexual repertoire even in the developing world been said with regards to widespread use of azole compounds in lieu of penetrative sexual intercourse or part of the foreplay. Though boric acid is very effective in their treatment its some case-control studies [6] found no evidence of an association efficacy ends with cessation of treatment [89]. It may also lead to study of 250 pregnant women concluded that extensive antibiotic colonisation with less susceptible Candida spp or development of use posed little risk for the development of yeast infection [51]. The fact that there is precise relationship between yeast colonization and symptomatic no cure even after such a prolonged treatment course, with 60 yeast vaginitis is not entirely clear. Martinez [146] reported that at baseline that increased to 50% after 10 days of antibiotic therapy the frequent and/or long-term antifungal therapy may predispose [56]. Contrary to the commonly posited hypothesis that vaginal even the benefit of physical examination and/or laboratory tests lactobacillus colonisation has a protective effect, McClelland in most of our clinical settings. Some patients even self-medicate [102] found that such colonization was in fact associated with with over-the-counter prescriptions. Some of the reasons for nearly four-fold increase in the likelihood of symptomatic genital this include financial constraints, lack of diagnostic facilities and candidiasis [102]. However oral nor vaginal lactobacillus administration prevented genital even when they are performed, they are not conclusive and do candidiasis following antibiotic use [54]. Most of the relevant clinical References trials had methodological problems such as small sample sizes, no 1. They contended though that empirical use of protection against symptomatic vaginal candidiasis. Magliani W, Conti S, Cassone A, De Bernardis F, Polonelli L (2002) programmes using Candida antigens [54,87]. Foxman B (1990) the epidemiology of vulvovaginal candidiasis: have contributed to the design of novel immunotherapeutic risk factors. Immunotherapy is considered a candidiasis: a case-control study among university students. It affects the womans quality of life and may impact negatively on her sexual life as well. Am J Obstet Gynecol 185(2): the womans social and professional lives may also be seriously 363-369. All health care providers need to be aware of the pathogenesis, Sex Transm Inf 77: 179-183. J Fam be due to genital candidiasis and routine antibiotic prescription Pract 42(6): 595-600. They may include predisposing factors, preventive Obstet Gynecol 104(5 pt 1): 926-930. A Study among Women Attending a Primary Healthcare Clinic in (1997) Prevalence of and risk factors for fungal vaginitis caused Kwazulu-Natal, South Africa. Candida species in women with vulvovaginal symptoms and their association with different ages and contraceptive methods. Tarry W, Fisher M, Shen S, Mawhinney M (2005) Candida albicans: the estrogen target for vaginal colonization. Eur antidepressant in women: postmarketing surveillance data in J Epidemiol 11(5): 575-579. Effect of parenteral antibiotic administration on establishment of intestinal colonization by Candida glabrata in adult mice. Rylander E, Berglund A-L, Krassny C, Petrini B (2004) Vulvovaginal Antimicrob Agents Chemother 49(1): 438-440. Bluestein D, Rutledge C, Lumsden L (1991) Predicting the Sex Transm Infect 80: 54-57. Obstet Gynecol 109(5): 1123 Effect of Antibiotics on Vulvovaginal Candidiasis: A MetroNet Study. Clancy R, Corrigan E, Dunkley M, Eyers F, Beagley K (1999) risk factors for vulvovaginal candidiasis. J Infect Dis 199(12): 1883 Recurrent Vulvovaginal candidiasis-allergy or immune deficiency? J (2005) Antifungal susceptibilities of Candida species causing Reprod Med 53(6): 402-406. Sonnex C, Lefort W (1999) Microscopic features of vaginal candidiasis and their relation to symptomatology. Biswas S, Van Dijck P, Datta A (2007) Environmental Sensing and transmitted infections 75(6): 417-419. Signal Transduction Pathways Regulating Morphopathogenic Determinants of Candida albicans. Cernicka J, Subik J (2006) Resistance mechanisms in fluconazole Obstet 279(2): 125-129. N Engl J Med 355: 1244 of candida species in vaginal samples in a clinical laboratory 1252. Clin Obstet Gynecol 36(1): recurrent vulvo-vaginal candidosis as a chronic illness. Sex vaginal product, in women affected by vulvovaginal candidiasis: a Transm Dis 28(10): 579-597. Cassone A, De Bernardis F, Santoni G (2007) Anticandidal immunity 7(9): 1167-1174. Stimulation of cell motility and expression of late markers of Curr Womens Health Rep 1(1): 31-35. The recurrent vulvovaginal candidiasis: proposal of apersonalized therapeutic protocol.
Vaginal epithelial cells with Vulvovaginal Vaginal or systemic antibiotic use menopause joint pain cheap clomid 50 mg with visa, diet high borders obscured by adherent coccobacilli seen on saline candidiasis in refned sugars pregnancy underwear buy cheapest clomid, uncontrolled diabetes wet-mount preparation women's health center king of prussia pa buy clomid 100 mg mastercard. More than 50 percent of women with bacte Irritant contact Soaps women's health clinic in richmond hill buy clomid 50 mg free shipping, tampons breast cancer z11 discount clomid master card, contraceptive devices the women's health big book of exercises pdf free order clomid 25 mg without a prescription, rial vaginosis are asymptomatic. The fshy odor caused dermatitis sex toys, pessary, topical products, by production of amines from anaerobic bacteria found douching, fastidious cleansing, in many of these patients is predictive of bacterial vagi medications, clothing 2 nosis. When vaginal alkalinity increases after sexual Allergic contact Sperm, douching, latex condoms or dermatitis diaphragms, tampons, topical products, intercourse (with the presence of semen) and during medications, clothing, atopic history menses (with the presence of blood), the odor becomes more prevalent. Bacterial vaginosis is not asso ciated with vaginal mucosal infammation and rarely causes vulvar itch. Causes, Symptoms, and Signs of Vaginitis ciated with a high incidence of endometritis and pelvic infammatory disease following abortion and gynecologic Clinical symptoms Clinical signs procedures in the general population. Among women with bacterial vaginosis, no overall increased risk of Type Etiology Discharge Pain Pruritus Vagina Vulva 28 developing pelvic infammatory disease has been found. Bacterial vaginosis Gardnerella vaginalis, Malodorous; homogenous; Not primary symptom Not primary No signs of infammation Unaffected Bacterial vaginosis is associated with late miscarriages, Mycoplasma hominis clear, white, or gray; fshy symptom premature rupture of membranes, and preterm birth. The positive presence of these two tests pH pH > 5: sensitivity, 77%; specifcity, 35% pH > 5. Cervical cytology has no clinical value for sample of vaginal discharge) diagnosing bacterial vaginosis, especially in asymptom Fem Exam card (Cooper Surgical, Shelton, Conn. Nonpregnant women with symptomatic Sensitivity, 53 to 90%; specifcity, Sensitivity, 50 to 70% (may be increased by Sensitivity, 61%; specifcity, 77% 40 to 100% vaginal lavage to 74%); specifcity, 100% disease require antibacterial therapy to relieve vaginal symptoms. One disad with murine monoclonal antibodies 33 vantage of oral regimens is a longer duration of treatment. Metro amplifcation (Quest Diagnostics, Madison responsible for bacterial vaginosis than culture in detecting Candida; not yet nidazole, 500 mg twice daily for one week, is effective for N. Although lactobacillus probiotics are safe, there is no Reference laboratory testing* conclusive evidence that they are superior to or enhance Culture Predictive value of a positive Gardnerella InPouch Culture System (Biomed, White Positive culture alone does not necessarily indicate $$$ vaginalis culture is less than 50%; City, Ore. Most relapses of bacterial vaginosis occur within the frst year and strongly correlate with new sex partners. Vaginitis is adequate but can cause dyspepsia and metallic taste; compliant patients may prefer a longer regimen at a lower daily dosage with fewer adverse effects. Metronidazole in a dosage of 500 mg twice daily for seven days will treat bacterial vaginosis and trichomoniasis. Metronidazole in a dosage of 2 to 4 g daily for seven to 14 days is recom mended for metronidazole-resistant strains. The parasitologic cure rate of intravaginal nitroimid azole creams is an unacceptably low 50 percent. When vaginal combined oral and intravaginal treatments have been wet-mount preparation is promptly examined, motile more effective than oral treatment alone. Sex partners trichomonads with fagella slightly larger than a leuko should be treated simultaneously. Reported recurrence rates are 15 to 30 percent within Test of cure is not required. A trial of women treated Trichomoniasis before 23 weeks of gestation was stopped early because Symptoms and signs of trichomoniasis are not specifc, women taking metronidazole were more likely to give and diagnosis by microscopy is more reliable. Adding examination of the spun urine specimen can environment precipitate and induce pathologic effects of increase the detection rate of Trichomonas vaginalis from the organism. In Although symptoms of vulvovaginal candidiasis such one study, the sensitivities of wet-mount preparation, as pruritus, vaginal soreness, dyspareunia, and vaginal microbiologic culture, rapid antigen testing, and nucleic discharge are common, none of them are specifc. Specifcity was close to 100 percent for each (Figure 3) of vaginal secretions with a 10% potassium method. Vaginal from tampons and introital specimens is more accurate pH is usually normal (4. Vaginal culture should than vaginal or cervical swabs and Pap smears, and may be considered in recurrently symptomatic women with be preferable for patient comfort. Both systemic and topi cal estrogen treatments are effective in relieving symp toms. Topical vaginal estrogen is preferred because of the low systemic absorption and reduced risk of adverse effects compared with oral therapy. Estrogen-containing creams, pessaries, intravaginal tablets, and the estradiol vaginal ring appear equally effective for the symptoms of atrophic vaginitis. Budding yeast visible Data Sources: We reviewed recent relevant publications in the (arrow. The search included 15 meta-analyses, randomized controlled trials, clinical reviews, and clinical a mean of $65 for the yeast culture. Terms included vaginitis, trichomoniasis, bacterial vaginosis, candi reaction testing is considered the most sensitive method, dal vulvovaginitis, and atrophic vaginitis. On the basis of clinical presentation, microbiology, host the Authors factors, and response to therapy, vulvovaginal candidia sis can be classifed as uncomplicated or complicated. Hainer is on the speakers bureau for Merck and involves a short course of antifungals47 (Table 413,32); oral Sanof Pasteur regarding immunizations, but has no fnancial disclosure 13,48 relevant to the topic of this article. The menopause: health implications and clini sis involves an intensive, longer course of antifungals cal management. Higher-risk behavioral practices associated with bacterial vaginosis com Noninfectious Causes of Vaginitis pared with vaginal candidiasis. Douching in relation to bacterial Irritant contact dermatitis and allergic contact derma vaginosis, lactobacilli, and facultative bacteria in the vagina. Intravagi nal metronidazole gel versus metronidazole plus nystatin ovules for ucts or contraceptive materials, among many other bacterial vaginosis: a randomized controlled trial. It affects 10 to 40 percent of nosis in lesbians and heterosexual women in a community setting. Diagnosis is based on history and physical long-term use of nonoxynol-9 on vaginal fora. Antibiotics for treating bac testing for vaginal yeast detection: a prospective study. Screening for bacterial vaginosis in rapid diagnostic kit (FemExam) for bacterial vaginosis in patients with pregnancy to prevent preterm delivery: U. Infuence of bacterial vaginosis on the Affrm Ambient Temperature Transport System for the detection conception and miscarriage in the frst trimester: cohort study. Am J Obstet pares favorably with transcription-mediated amplifcation assay for the Gynecol. Detection of Chlamydia trachoma Candida species by culture and polymerase chain reaction. Arch Gyne this and Trichomonas vaginalis by polymerase chain reaction in introi col Obstet. Prevalance of bacterial vagniosis: 2001-2004 of uncomplicated vulvovaginal candidiasis (thrush. Clinical practice guidelines for the management of candi tic and pathogenetic fndings during topical clindamycin therapy. The most common causes of vaginitis are bacterial vaginosis, vulvovaginal candidiasis, and trichomoniasis. Bacterial vaginosis is implicated in 40% to 50% of cases when a cause is identifed, with vul vovaginal candidiasis accounting for 20% to 25% and trichomoniasis for 15% to 20% of cases. Noninfectious causes, including atrophic, irritant, allergic, and infammatory vaginitis, are less common and account for 5% to 10% of vaginitis cases. Diagnosis is made using a combination of symptoms, physical examination fndings, and ofce-based or laboratory testing. Bacterial vaginosis is traditionally diagnosed with Amsel criteria, although Gram stain is the diagnostic standard. Bacterial vaginosis is treated with oral metronidazole, intravaginal metronidazole, or intravaginal clindamycin. Culture can be helpful for the diagnosis of complicated vulvovaginal candidiasis by identifying nonalbicans strains of Candida. Treatment of vulvovaginal candi diasis involves oral fuconazole or topical azoles, although only topical azoles are recommended during pregnancy. The Centers for Disease Control and Prevention recommends nucleic acid amplifcation testing for the diagnosis of trichomoniasis in symptomatic or high-risk women. Trichomoniasis is treated with oral metronidazole or tinidazole, and patients sex partners should be treated as well. Infammatory vaginitis may improve with topical clindamycin as well as steroid application. Noninfectious causes, including atrophic, lives,2 making it the most common gynecologic diagnosis irritant, allergic, and infammatory vaginitis, are less com in primary care. Studies have shown a negative effect on mon and account for 5% to 10% of vaginitis cases. The most common causes of vaginitis are bacterial vaginosis, vulvovaginal candidiasis, and trichomoniasis. For the private, noncom Downloaded from the American Family Physician website at Trichomoniasis Low socioeconomic status, multiple sex partners, other bacterial vaginosis are a cheesy, curdy, or sexually transmitted infections, unprotected intercourse, drug use, smoking focculent discharge; itching; vulvar or vaginal infammation or redness; and lack Atrophic or Menopause, lactation, oophorectomy, radiation therapy, of odor. Patients should be instructed to insert the swab at least one inch into the vagina. Three out of four criteria are required to make the diagnosis, with sensitivity ranging from 70% to 97% and specifcity from 90% to 94%, compared with Gram stain. Routine testing in asymptomatic women and retest recurrent (four or more episodes in one year) or severe ing (test of cure) are not recommended because these bac infections, or infections that occur in a patient who is teria can be part of normal fora. If nonalbicans infection is present, consider first-line ther apy with seven to 14 days of a nonfuconazole azole agent. If infection recurs, prescribe 600 mg of boric acid in a gelatin capsule intravaginally once daily for two weeks. Boric acid may also be used with initial induction therapy followed by monthly maintenance therapy for recurrent albicans infection per the Society of Obstetricians and Gynaecologists of Canada recommendations. These tests have Trichomoniasis is a sexually similar sensitivity and specifcity transmitted infection that to vaginal samples. It can inal wet-mount preparation is promptly There is no cause of vagini be diagnosed when motile, fag examined, motile trichomonads with fa this identifed in up to 30% of ellated protozoa are observed on gella slightly larger than a leukocyte may women. Infammatory endocervical, vaginal, or urine specimens, or on liquid vaginitis is associated with low estrogen levels, such as in based Pap test samples. Physicians should Over-the-counter intravaginal agents explain potential adverse effects with each Clotrimazole 1% cream, 5 g intravaginally daily for seven to 14 days regimen, including a possible disulfram-like Clotrimazole 2% cream, 5 g intravaginally daily for three days reaction with alcohol consumption or gastro Miconazole 2% cream, 5 g intravaginally daily for seven days intestinal symptoms in persons taking oral Miconazole 4% cream, 5 g intravaginally daily for three days metronidazole, or possible weakening of latex Miconazole 100-mg vaginal suppository, one suppository daily for seven days condoms with the use of topical therapies con 9 Miconazole 200-mg vaginal suppository, one suppository daily for taining oil-based preparations. Food and Drug Administration Miconazole 1,200-mg vaginal suppository, one suppository for one day recently approved a single-dose oral therapy for Tioconazole 6. In the past, treatment for bacterial vaginosis during pregnancy was in a single 150-mg dose. In nonpregnant patients, there is no defnitive in preterm labor with treatment of bacterial vaginosis, par advantage of one treatment over another in terms of clin ticularly in early pregnancy (before 20 weeks gestation),46 ical or mycologic cure, with all treatment options having a more recent meta-analysis of 21 studies found that antibi about an 80% cure rate. Oral fuconazole offers the advantage preterm labor before 37 weeks gestation with treatment; of one-dose convenience without messy creams or sup therefore, further investigation may provide more infor positories. Oral medications may cause systemic adverse mation about the role of abnormal bacterial fora and its effects, particularly gastrointestinal effects and toxic treatment in pregnancy. An rial vaginosis is generally recommended for symptomatic additional factor to consider is that topical azole creams relief, and adverse effects of metronidazole in pregnancy and suppositories may be oil-based and can weaken latex have not been demonstrated. There are several topical azole preparations and shown that, regardless of whether they have a history of regimens available, as well as oral fuconazole (Difucan) vulvovaginal candidiasis, women are not able to accurately 326 American Family Physician Ofce-based or laboratory testing should be clotrimazole, miconazole, and keto used with the history and physical examination fndings conazole) are more effective in erad to make the diagnosis. In a small study, topical Do not obtain culture for the diagnosis of bacterial vagi C 9 terconazole was also shown to relieve nosis because it represents a polymicrobial infection. A meta-analysis did not demonstrate clear evidence A = consistent, good-quality patient-oriented evidence; B = inconsistent or limited-quality patient-oriented evidence; C = consensus, disease-oriented evidence, usual practice, expert for probiotics in the treatment of can opinion, or case series. Patients with tion at test of cure and lower rates of reinfection at three complicated vulvovaginal candidiasis require more aggres months. To guide treatment, it is helpful to consider also a frst-line treatment for trichomoniasis; however, it is whether a patient has recurrent infections and whether the more expensive. Metronidazole-resistant trichomoniasis, etiology may be a nonalbicans species of Candida. Trichomoniasis has been second dose of fuconazole given three days after the frst associated with adverse pregnancy outcomes, including dose has been shown to achieve signifcant improvement low birth weight and preterm birth. A second dose did not have signifcant effects for tested and considered for treatment. Atrophic vaginitis is treated with for three doses) followed by weekly treatment with 150 hormonal and nonhormonal therapies. Among hormonal mg fuconazole for six months has been shown to achieve therapies, low-dose vaginal estrogen preparations are symptomatic relief at one year for most patients. Systemic estrogen If severe or recurrent vulvovaginal candidiasis does not therapies are also available for patients with vasomotor respond to initial treatment, culture may guide therapy symptoms. Infections with mendations include vaginal lubricants and moisturizers; nonalbicans species are less responsive to fuconazole. The limited value of symptoms duration of treatment and superiority of one agent over the and signs in the diagnosis of vaginal infections. The classic this article updates previous articles on this topic by Hainer approach to diagnosis of vulvovaginitis: a critical analysis. Determining the cause of vulvovaginal literature review from Essential Evidence Plus. Vulvovag initis: screening for and management of trichomoniasis, vulvovaginal candidiasis, and bacterial vaginosis.
Buy 100mg clomid with visa. Whitney's Got Big Dreams For Big Girl Dance Class | My Big Fat Fabulous Life.
Syndromes
- Seizures
- High or severely low blood pressure
- Chronic myelogenous leukemia
- Allergic reactions to medicines
- Breads and crackers made with enriched flour and whole grains, served with fruit spread or fat-free cheese
- Sensitivity to light
Therefore pregnancy 9 weeks symptoms clomid 50mg with amex, increasing attention is being focused on the aggressive prevention and treat ment of acute pain to reduce complications women's healthy eating plan purchase clomid with a visa, including progression to chronic pain states pregnancy quant levels quality clomid 50mg. Chronic Pain nitive breast cancer 9 oclock position 50mg clomid visa, as well as sensory breast cancer breakthrough buy clomid once a day, features that occur in 22 Chronic pain was once defined as pain that response to tissue trauma menopause journal article buy clomid on line. Acute pain is usually nociceptive, but may be Chronic pain is now recognized as pain that neuropathic. Common sources of acute pain extends beyond the period of healing, with lev include trauma, surgery, labor, medical proce els of identified pathology that often are low and dures, and acute disease states. Table 3 summa insufficient to explain the presence and/or rizes its key features. A host of protective reflexes and normal living, ceases to serve a protective Table 3. National Pharmaceutical Council 11 Section I: Background and Significance function, and instead degrades health and func els that only weakly correspond to identifiable tional capability. In some chronic noncancer pain and chronic non cases, chronic pain exists de novo with no cancer-related pain. In some Environmental and affective factors also can cases, there is no discernable cause, and the pain exacerbate and perpetuate chronic pain, leading is considered the disease. Examples of Chronic First, its acute and chronic components and mul Noncancer Pain tiple etiologies make it difficult to classify based on duration or pathology alone. This find ing prompted recommendations including the scheduled administration of pain medications via other routes. These consequences affect hospitalized patients, 61% of the 217 patients patients, their families, and society as a whole interviewed reported pain ratings of 7 to 10 (on and can be broadly categorized as physiological, a scale from 0 for no pain and 10 for the worst psychosocial (quality of life), and financial. What Is the Size and Scope of adequacy of analgesia in an urban emergency Pain As A Health Care Problem? Acute pain is the most common reason why Hispanic patients with long-bone fractures were patients seek medical attention. Chronic pain is also a problem of epidemic pro reported sufficient control of moderate pain. About 50 million of the estimated 75 However, this percentage decreased to 51% in million Americans who live with serious pain patients with severe pain and to 39% in those suffer from chronic pain. Results from a 2001 sur ing with their pain for more than 5 years and vey suggest that most individuals with severe experience pain almost 6 days a week. Low back pain, arthritis, and migraine headache alone account for pain in tens of mil Approximately two-thirds (67%) of the patients lions of Americans. What Are the Consequences and One study showed that pain levels in patients hospitalized for serious conditions (e. Physiological consequences treated pain early in life is associated with pain As discussed in Section I. Quality of life can have adverse effects if allowed to persist Inadequate control of pain interferes with the unchecked. Table 5 summarizes some of the pain sufferers ability to carry out activities of adverse physiological consequences of inade daily living (e. Very young, very old, and frail patients 13 pain may experience anxiety, fear, anger, depres are at greatest risk for such complications. In 15 sion, or cognitive dysfunction, and family one study of neonates who underwent cardiac members report varying levels of helplessness, surgery, patients who received light versus frustration, and heartbreak. These indi Another key adverse effect of poorly con viduals report impairments on multiple measures trolled acute pain is progression to chronic 124-125 of physical, social, and psychological well-being, pain. Examples of Physiological Consequences of Unrelieved Pain Functional Domain Stress Responses to Pain Examples of Clinical Manifestations Endocrine/metabolic Altered release of multiple hormones (e. Pain: Current Understanding of Assessment, Management, and Treatments 14 Section I: Background and Significance ence health care. Barriers Within the Health Care toms can contribute to more serious conse System quences. Financial consequences standard pain assessment tool or to provide staff Pain costs Americans an estimated $100 bil with sufficient time and/or chart space for docu lion each year. Others fail organizations, and society bear this financial to provide clinicians with practical tools and burden. However, the greatest systems barrier to plications associated with inadequately con appropriate pain management is a lack of trolled acute pain can increase length of stay, re accountability for pain management practices. It is a leading cause of medically incidents) to ensure effective pain manage related work absenteeism and results in more ment. Patient care is more frag long-term or permanent unemployment or mented; thus, the risk of poor coordination of underemployment. Health Care Professional Barriers Clinicians attitudes, beliefs, and behaviors the undertreatment of pain reflects barriers to contribute to the undertreatment of pain. These barri example, some clinicians do not view pain relief ers can be broadly categorized as those attributa as important and/or do not want to waste time ble to the health care system, clinicians, patients assessing pain. Studies have shown that lack of tribute to a failure to assess pain, to accept the assessment, underassessment, and a disparity patients self-report of pain, and/or to take 140 between the clinicians and the patients ratings appropriate action. National Pharmaceutical Council 15 Section I: Background and Significance Inappropriate or exaggerated concerns and inad patients, whereas half experienced moderate to equate or inaccurate clinical knowledge also severe pain, only 30% wanted additional pain limit clinicians abilities to appropriately manage treatment. Patient and Family Barriers patients with chronic pain do not seek medical Whereas poor clinician-patient communica attention. Legal and Societal Barriers Legal and societal issues also contribute to the undertreatment of pain. Common Misconceptions restrictive laws or regulations about the prescrib ing of controlled substances as well as confusion About Pain about the appropriate role of opioids in pain treatment. Prior experience with pain teaches a person to be more and Addiction tolerant of pain. Patients who are knowledgeable about pain medications, are frequent emergency department patrons, or have been important roles in pain management. However, taking opioids for a long time are necessarily addicts or concerns about their potential misuse and mis drug seekers. Although studies suggest a state of adaptation that often includes tol that the risk of iatrogenic addiction is quite low erance and is manifested by a drug class spe (e. Etiology, issues, and concerns may be essential in the treatment of acute pain Many medications produce tolerance and due to trauma or surgery and chronic pain, physical dependence, and some (e. Assessment is an essential, but challenging, com Successful pain management depends, in part, on cli ponent of any pain management plan. Pain is subjec nician adherence to such standards and guidelines tive, so no satisfactory objective measures of pain and commitment to some core principles of pain exist. Pain is also multidimensional, so the clinician assessment and management (Table 7. Goals and Elements of the Initial lation, clinician), so no single approach is appropriate Assessment for all patients or settings. Important goals of the initial assessment of pain this section reviews some core principles of pain include establishing rapport with the patient and pro assessment and management to help guide this 8 viding an overview of the assessment process. It then explores approaches that clinicians processes help to engage the patient, foster appropriate can use in the initial assessment of pain. The clinicians primary Subsequent discussions explore tools that facilitate objective is to obtain information that will help identify assessment and address the reassessment of pain. Overcoming Barriers to Assessment and Management Assessment Underassessment of pain is a major cause of inade-. Patients have the right to appropriate assessment and quate pain management (see I. Special 1 considerations are needed for patients with difficulty action when patients report pain. Family members should be included in Health Administration recognized the value of such the assessment process, when possible. Different patients experience different levels of pain in on Accreditation of Healthcare Organization response to comparable stimuli. Whereas assessing pain with each assessment of the standard four vital signs is appropriate in some clinical situations, more Sources: References 1 and 4-7. Obtaining a comprehensive history provides history, physical examination, and appropriate diagnos many potential benefits, including improved manage tic studies are typically conducted for this purpose. Information Fromthe Patient History Parameter Information To Be Obtained Sample Questions Pain characteristics Onset and duration When did the pain begin? Management strategies Past and current: What methods have you used to manage the pain? Both the s Relevant family history choice of tool and the general approach to assessment s Current and past psychosocial issues or factors should reflect the needs of the patient. Tables 10 and 11 summarize and functioning approaches to assessment in patients with impaired s the patients and familys knowledge of, expecta ability to communicate. As unrelieved pain has adverse physical and psycho logical consequences, clinicians should encourage the reporting of pain by patients who are reluctant to dis Table 9. In such cases, the clinician needs to avoid as angina, pancreatitis, appendicitis, attributing the pain to psychological causes and to acute cholecystitis) 5 accept and respect the patients self-report of pain. Projected (transmitted) pain: pain transferred along the course of a nerve Other clinicians often have seen and/or treated with a segmental distribution (e. Given the link between chronic pain and neuropathic pain Nondermatomal: central neuropathic pain, fibromyalgia No recognizable pattern: complex regional pain syndrome Table 10. Assessment of Patients Duration and Brief flash: quick pain such as a needle periodicity stick With Barriers to Communication Rhythmic pulses: pulsating pain such as a migraine or toothache Longer-duration rhythmic phase: Patient Populations intestinal colic. Give patient the opportunity to use a rating scale or other Visceral pain: dull aching or cramping tool appropriate for that population. Use indicators of pain according to the following hierarchy lancinating, jabbing, squeezing, aching of importance: Associated signs Visceral pain: sickening feeling, Patient self-report and symptoms nausea, vomiting, autonomic symptoms Pathological conditions or procedures known to be painful Neuropathic pain: hyperalgesia, Pain-related behaviors (e. Assessment Challenges and Approaches in Special Populations Population Challenges Approaches Elderly Under-reporting of discomfort due to fear, cultural Avoid time pressure in assessment factors, stoicism Evaluate for impairments that limit ability to Impairments (e. Key ele formal assessment of disability in a patient who is ments of this evaluation include a more comprehen applying for disability benefits. Appropriately selected tests the initial assessment of a patient with pain can lead to accurate diagnosis and improve outcomes includes a physical examination. Table 16 summarizes examples of diag general physical condition, with special attention to nostic studies used in patients with pain. Postoperative Assessment Patient Education Recommendations and Patient Education Recommendations. Increase the frequency of assessment for factual report of pain, preventing or halting pain before it changing interventions or inadequate pain control. Such preference; 2) the assessors expertise, time, and degree of discrepancies may reflect good coping skills or effort available; and 3) the institutions requirements for diversionary activities (e. Although be indicative of complications including wound dehiscence, useful for assessing acute pain of clear etiology (e. Unidimensional Scales representing no pain at all and 5 or 10 repre Rating scales provide a simple means for patients senting the worst imaginable pain. Pain treatment history: full review of results from past Although not used as often as they should be, mul work-ups and treatments as well as patients utilization of tidimensional tools provide important information health care resources (e. Examples of multidimensional tools include expectations of family members, employers, attorneys, or (see Table 18): social agencies (e. The cli bined with other tools to improve diagnostic nician then measures the line with a ruler and accuracy. Physical Examination of a Patient With Pain Region Rationale, Methods, and Potential findings General Observe and/or identify:. The recently developed Neuropathic Pain outpatients to contact them to report changes in the Scale provides information about the type and degree pains characteristics, side effects of treatment, and of sensations experienced by patients with neuropath 27 treatment outcomes. It evaluates eight common qualities of neu mended in patients with chronic pain to evaluate ropathic pain. Scope and Methods the scope and methods of reassessment vary with factors including the setting, characteristics of the pain, the patients needs and medical condition, and responses to treatment. This section reviews some need for further assessment, consideration of pain approaches to reassessment in common clinical set relieving interventions, and post-intervention follow tings and situations. Reassessing pain with each evaluation of the vital bThe Agency for Health Care Policy and Research is now the Agency for Health Care Research and Quality. Drug Classifications and prompt (minutes to hours), whereas the anti inflammatory effect may take longer (1-2 weeks Terminology or longer. In the below system, analgesics rily produces prostaglandins with beneficial are broadly categorized as: effects (e. Variations of this classification system exist, and terminology in the field is also evolving. Indications and uses the term opioids has replaced narcotics, and Nonopioids relieve a variety of types of acute co-analgesics is an alternate term for adjuvant and chronic pain (e. Examples of Nonopioid Analgesics Usual Oral Dosage Dosing Forms and Chemical Generic Interval or Routes of Major Side Class Name Indications Frequency Administration Effects Comments Paraaminophenols Acetamin Mild to moderate q 4-6 ha Multiple oral Acute overdose: Lacks anti-inflammatory ophen pain due to (e. Nonopioids do not produce tolerance, inhibitor may be an appropriate treatment alter physical dependence, or addiction. In addition, acute Patients usually take nonopioids orally, but or chronic overdose with acetaminophen may other forms (e. In addition, some nonopioids are mar also may occur in patients taking over-the keted in combination with other drugs (e. In contrast to most opioids, all trial data suggest that celecoxib produces compa nonopioids have a dosage ceiling. In mission of nociceptive input from the periphery this system, opioids are broadly classified as mu to the spinal cord, 2) activate descending agonists or agonist-antagonists. Equianalgesic dosing charts help clini Opioids are used to treat moderate to severe cians determine the appropriate starting dose of pain that does not respond to nonopioids 19 an opioid when changing routes of administra alone.