T. Andrew Bowdle, MD, PhD
- Professor of Anesthesiology and Pharmaceutics
- Chief of the Division of Cardiothoracic Anesthesiology
- Department of Anesthesiology
- University of Washington
- Seattle, Washington
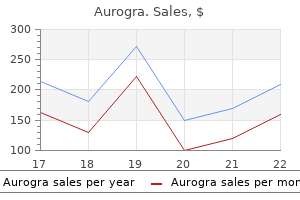
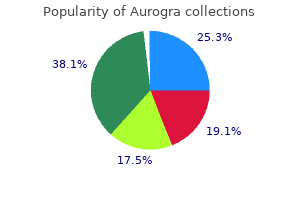
Here erectile dysfunction foods to eat generic aurogra 100mg with amex, patients believe Tactile hallucinations may also occur and may be quite that chance events erectile dysfunction protocol list buy cheap aurogra 100 mg online, rather than being innocuous and varied erectile dysfunction treatment hyderabad purchase aurogra 100mg on line. Patients may feel electric currents course over their unrelated to them what causes erectile dysfunction in diabetes cheap aurogra 100 mg with amex, in fact bear special meaning and bodies; they may complain that fluids are poured on them pertain specifically to them erectile dysfunction early age buy discount aurogra on-line. Newspaper headlines seem to at night or that they are pricked by needles from behind; in be a kind of code erectile dysfunction 20 buy 100 mg aurogra overnight delivery, which only the patient can decipher, some cases they may experience movements deep inside, informing him or her that the time is near; street lights such as crampings and twistings. For patients with delusions of reference, although their content is extremely varied, certain themes at times all things seem pregnant with meaning: there stand out, including delusions of persecution, delusions of are no more chance occurrences, no accidents, and no grandeur, delusions of reference, and a number of coincidences. These false beliefs may Schneiderian first rank symptoms may comprise delueither grow slowly in the patient or occur suddenly, as if in an sions, including thought broadcasting, thought withdrawal, enlightenment. Although some patients may entertain some thought insertion, and delusions of influence, control, or lingering doubts as to the veracity of these beliefs, for most passivity. In thought broadcasting, patients believe that they are as self-evidently true as any other belief. In such cases, patients suddenly become may see mere tangentiality or circumstantiality. In tangenbereft of thoughts and are left with blank minds; some may tiality, in response to a question, thoughts proceed off on a elaborate on the experience and speak of electrical or magtangent and patients never get around to giving an answer; netic devices that remove the thoughts. Both forms may be seen in their thoughts, feelings, or actions are somehow directly schizophrenia and, indeed, it is not uncommon to see indiinfluenced or controlled by some outside force or agency, vidual patients with the catatonic subtype of schizophrenia and that they have somehow become like robots or passive exhibit both forms at different times (Morrison 1973). Some again porous catatonia one sees immobility, catalepsy, and mutism, may elaborate on these beliefs and speak of being under the which may be joined by posturing, echolalia or echopraxia, influence of a spell or perhaps of an electrical or magnetic negativism, or automatic obedience, whereas in excited catamachine, or perhaps a distant computer. In a manneristic gesture, the patient may offer a hand to In considering the sign of disorganized speech we are conshake with the fingers splayed out, or the fingers may intercerned not with the content of speech, which may be committently writhe in a peculiar, contorted way. Overall behavior may undergo manneristic incoherent; thoughts are juxtaposed that have no conceivtransformation; one patient walked in a stiff-legged fashable connection and family members may complain that ion, rigidly swinging only one arm with each step. In other cases connection with each other than do the tossed leaves of a there may be inappropriate affect. Twenty-five in the case of a patient who, although feeling sadness at the dollars is a lot of money! Typically, patients are unconcerned with their untidy and may neglect to clean their clothes or to bathe. Some seem almost analgesic: one patient bit out part of to predict how the patient will act in any given situation. In paranoid schizoaffect when less severe, is, as discussed further in Section phrenia, more so than in any other subtype, the delusions 4. In poverty of thought, by contrast, patients speak escape, perhaps by moving to another area, or they may little, essentially because there is a wide-ranging and farturn on their supposed attackers, sometimes violently. Patients believe that they are ply, nothing comes to mind; there are no stirrings. One patient believed himself to be the anointed of hours or days in quietude, doing nothing. Catatonic schizophrenia, as the name obviously indiOf the miscellaneous symptoms seen in schizophrenia, percates, is dominated by catatonic symptoms. Patients may complain of depressive symptoms, such as schizophrenia may demonstrate only one form throughout feeling depressed, being tired or having trouble sleeping; the course of the illness, in most cases, as noted earlier, some may demonstrate some euphoria and increased energy these two forms are seen to alternate in the same patient. Indeed, at first glance these symphours on one extreme to months or years on the other. The toms may seem to dominate the clinical picture; however, transition from one form to another may be quite unpreon a closer and wider look one finds that they are transient, dictable and, at times, quite sudden; in one case a chronilasting only hours or days, are mild overall, and, relative to cally stuporous patient, without any warning, suddenly other symptoms, such as hallucinations and delusions, play jumped from his bed, screamed incoherently, and paced only a very minor role in the overall clinical picture. Overall, the various subtypes pursue different courses with different the behavior of these patients seems at times to represent a p20. Senselessly, they may busy Course themselves, first with this and then with that, generally to no purpose and often with silly, shallow giggling. At times Schizophrenia is a chronic, lifelong disease and most they may be withdrawn and inaccessible. When delusions patients suffer considerable disability throughout their are at all prominent, they tend to be hypochondriacal in lives (McGlashan 1984; Tsuang et al. In some cases there may the disease exhibits one of two courses: an overall waxing also be disorganized speech, with marked loosening of assoand waning course or a chronic, slow progression. The waxing and waning course is characterized by exacSimple schizophrenia (Black and Boffeli 1989; Kendler erbations and partial remissions. Few thoughts, desires or inclidepressive symptoms that may occasionally accompany an nations disturb them and they may appear quite content to exacerbation of psychotic symptoms. For the most and waning course may persist throughout the life of the part they do little to attract the attention of others and may patient or, in many cases, it may give way, after anywhere pass their lives in homeless shelters. Undifferentiated schizophrenia is said to be present the chronic progressive course may be evident from the when the clinical picture of any given case does not fit well onset of the disease, as for example in the simple subtype, into any one of the foregoing subtypes. This is not uncomor may become evident only after the initial onslaught has monly the case, and it also appears that, over long periods of settled some. Over long periods of time, there is a very time, the clinical picture, which initially did fit a particular gradual progression, after which many patients eventually subtype, may gradually change and become less distinctive. This transition from a recognized specific subtype to an As noted earlier, the subtype diagnosis may enable undifferentiated presentation appears to be most common some predictions to be made as to course (Fenton and with the catatonic and disorganized subtypes; by contrast, McGlashan 1991; Kendler et al. In reactive schizophrenia, the precatatonic schizophrenia of the stuporous type may die of morbid personality tends to be normal and the onset, which aspiration pneumonia or extensive decubiti. Suicide occurs is marked by depression and perplexity, is acute and occurs in about 10 percent of patients (Tsuang 1978); overall, about generally in adult years, often following some obvious social one-third will make a suicide attempt (Allebeck et al. In phrenia it is appropriate to consider whether or not, in the process schizophrenia, by contrast, the premorbid personalnatural course of events and in the absence of treatment, ity is often abnormal and the onset is insidious, often in schizophrenia ever undergoes a full, complete, and spontachildhood or adolescence, and without any recognizable preneous remission. Certainly, in cases that exhibit a waxing and cipitants; negative symptoms tend to dominate the clinical waning course, the partial remissions may be far-reaching picture. Of course, genetics cannot explain the entire picture or one would expect a much higher concordance rate in monozygotic twins, and consequently one must look to Etiology environmental factors. Furthermore, several studies have also demonparticularly vulnerable to certain of these factors. Autopsy studies support hypothesis is that the phenotypic expression of the disease the results of neuroimaging, demonstrating a reduced volis dependent upon an interaction between the fixed neuume in the medial temporal lobe structures (Bogerts et al. Although this neurodevelopmental theory of the etiology Furthermore, although not without controversy, some of schizophrenia has much to recommend it, the case is not subcortical structures may suffer neuronal loss (Byne et al. Differential diagnosis Although the mechanism underlying these anatomic changes is not known with certainty, it is strongly susAlthough a host of disorders enters the differential diagnopected that they represent a disorder of neuronal migrasis, only certain of them play a large part, thus making the tion. In the normal course of development, neurons differential task a little less daunting. These include mood migrate along radial glial fibers from the ventricular area disorders. Furthermore, and again putative disorders known as schizophreniform disorder normally, a small number of these neurons fail to migrate and brief psychotic disorder. The findings noted above of an increased number ized by episodes of mania and depression, whereas major of interstitial neurons and neuronal disarray in the cortex depressive disorder, as noted in Section 20. As noted earlier, schizophrenia occurs in progression in which typical manic symptoms are joined by about 1 percent of the general population; however, hallucinations and delusions and, in some, disorganized among first-degree relatives the prevalence rises to about 5 speech, and if one sees the patient at this stage of mania and percent, whereas among dizygotic twins it is about 20 perif there is no history, consideration might be given to a diagcent and among monozygtic twins the concordance rate nosis of hebephrenic, catatonic or paranoid schizophrenia. In mania, mood symptoms, into a brief period of excitation; such a lysis, occurring over namely heightened mood, increased energy, and decreased seconds or minutes, simply is not seen in depression. By contrast, in schizophrenia psychotic symptoms, such as hallucinations, delusions, or one finds that the course is marked by the presence of halludisorganized speech, and by intermittent episodes of either cinations before the onset of any mood symptoms; furthermania or depression, during which the pre-existing psymore, as noted earlier, any manic symptoms seen in chotic symptoms undergo an exacerbation. Certain point that allows a distinction from schizophrenia is that other features may also help in the differential diagnosis the mood disturbances, whether manic or depressed, are between mania and schizophrenia. The differential here rests on the ing and extroverted, and this is in marked contrast to the degree of plausibility and systematization of the delusions behavior of the excited catatonic patient, who typically and on the absence of other symptoms. By contrast, although there although both irritable manics and irritable paranoid schizmay be some plausibility and systematization to the deluophrenics are dangerous, the manic patient is recklessly so, sions seen in paranoid schizophrenia, close inspection typin contrast to the paranoid schizophrenic, who may become ically reveals some fragmentation and inconsistencies and violent only if approached in what appears, to the patient at almost always at least some hints of auditory hallucinaleast, to be a potentially hostile manner. The symptoms, however, the differential is fairly straightfordifferential here rests on the history: if the psychosis in ward providing that one has a reliable history: in depression question occurred only after many years of alcoholism characterized by hallucinations and delusions, these sympwith repeated episodes of delirium tremens, then a case toms only occur well after the typical depressive symptoms may be made for an alcoholic psychosis; in cases, however, have become well-established and severe; by contrast, in in which delusions or hallucinations occurred early on, schizophrenia, delusions and hallucinations precede the perhaps in adolescence or early adult years, and only after advent of depressive symptoms. Furthermore, the depresa relatively brief drinking career, then one would be hard sive symptoms seen in schizophrenia are generally transient pressed to explain them on the basis of alcoholism. The nature of the delusions Several personality disorders, namely those of the paraseen in depression may also be helpful. Thus, patients with depression sonality disorder are chronically distrustful and on guard, may come to believe that they have committed unpardonquick to take offense and to read malevolence into what othable sins or that their insides are drying up and dying, as is ers do, and prone to harbor deep, long-standing resentments; only fitting for such miserable sinners. In patients with paranoid schizophrenia, however, close indeed often bear no conceivable relationship to depresinspection will reveal other symptoms, such as delusions of sion, as, for example, in the case of a schizophrenic who other types. Finally, conin paranoid schizophrenia one often also sees some lack of sideration may be given to differentiating a severe depresfull systematization of the delusions, in contrast to the persive episode from a catatonic stupor. The distinction from schizophrenia rests on age, once every 4 or 2 weeks respectively. Schizotypal personality disorder is charChoosing among these agents is not straightforward. With acterized by chronic aloofness and by peculiar thoughts and regard to effectiveness, clozapine is clearly superior; however, behavior, and thus may mimic simple schizophrenia. The its side-effect profile, especially the risk of agranulocytosis, differential here rests on the overall course: in the personality limits its use to treatment-resistant cases. Of the other disorder there is no deterioration, whereas in simple schizoagents, although there is controversy here, it appears that phrenia one sees a very slow progression. This advantage, however, is severely (also known as brief reactive psychosis) are both charactertempered by the tendency of olanzapine to cause metabolic ized by symptoms that are similar to those seen in schizoderangements, including weight gain, hyperlipidemia, and phrenia; however, where they differ is in their supposed diabetes. However, there is a debate as idone stand out in that they are not associated with metabolic to whether such disorders actually exist. Overall, and all other things being equal, if a secondare patients with schizophrenia who are treated with generation agent is used, it may be reasonable to start with antipsychotics early in the course of the illness and who risperidone; however, again, it must be acknowledged that experience a complete, antipsychotic-induced remission of this is an area of great controversy. What is at issue here is generation, to prescribe, the first step is to obtain an accurate whether there are, in fact, cases in which symptoms spontreatment history, and this may require not only questioning taneously and completely undergo a lasting remission the patient but also reviewing records and interviewing famwithout treatment. If there is a history of a good response comaware of any such well-documented cases in the literature. In treatment-naive patients, or in cases in and, although most of these are rare, the reader is encourwhich prior treatments were unsatisfactory, other consideraged to gain familiarity with them. Although not without controversy, it appears that, overall, second-generation agents are more effective and better tolerated than first-generation ones, and, Treatment consequently, it may be reasonable to select a second-generation agent.
The outcome thin on young women: An experimental disorders: Do they distinguish unipolar and of anorexia nervosa in the 20th century erectile dysfunction at the age of 24 discount 100 mg aurogra with mastercard. Evidence for a hallucinogen conditioned drug effects in the selfdependence syndrome developing soon after Strober erectile dysfunction protocol hoax aurogra 100 mg for sale, M how do erectile dysfunction pills work generic aurogra 100mg without prescription. Negative-reinforcement drinking motor and sensory conversion symptoms: A therapy in a new key: A guide to time-limited motives mediate the relation between anxiety systematic and narrative review impotence trials france buy aurogra 100 mg without prescription. Treating hypochondriasis with interpersonal Handbook of research methods in clinical Sutker erectile dysfunction age 32 buy aurogra without prescription, P erectile dysfunction treatment videos purchase aurogra 100mg mastercard. Organizational strategies with unilateral or Personality and Social Psychology Bulletin, bilateral frontal lobe injury in word learning Swaab, D. The human hypoSubstance Abuse and Mental Health transthyretin levels in depression: Correlations thalamus: Basic and clinical aspects. Part 1: Services Administration, Office of Applied with suicidal ideation and low serotonin Nuclei of the human hypothalamus. The epidemiology and classification Pharmacokinetic and pharmacodynamic National Clearinghouse for Alcohol and of bulimia nervosa. Psychological Medicine, properties of stimulants: Implications for Drug Information. The invention of Substance Abuse and Mental Health Services post-traumatic stress disorder and the social Swanson, J. British Journal of Psychiatry, nervosa, bulimia nervosa, and binge eating Swartz, H. The Treatment Non-fat-phobic anorexia nervosa in British for Adolescents with Depression Study South Asian adolescents. Are some types of psychotic neuropsychiatric disorders associated with Brunner/Mazel. Heart risk associated with Sudden gains and critical sessions in of Psychological Procedures. Training weight loss in anorexia nervosa and eating cognitive-behavioral therapy for depression. Clinical neurological abnormalities Computer and Internet applications for disorder/multiple personality disorder: the in young adults with Asperger syndrome. Inverse relationship between social support buffer stress for college services to assist recovery. Treatment of major depression patients with borderline personality disorder: with psychotherapy or psychotherapyTaylor, C. The neurobiological psychological treatment and benzodiazepine Prevalence of eating disorders among Blacks consequences of early stress and childhood in dental phobia. Widiger cognitive-behavioral treatment for social deficit schizophrenia in Nithsdale, Scotland. Journal of Behavior Therapy and Journal of Nervous and Mental Disease, 189, factor model of personality (pp. Thinarising after road traffic collisions: Patterns violently: the usefulness of an earlyversus ideal internalization: Mounting evidence for of response to cognitive-behavior therapy. Affect, cognition, and change: Re-modelling medial prefrontal cortex during autonomic depressive thought. Chinese prevention of relapse in depression: empirical Prevention & Treatment, 5, Article 32. New England Journal of Medicine, avoidant personality disorder: One spectrum Torgersen, S. Cerebral blood fiow in subject comorbid depression: A systematic review with social phobia during stressful speaking Thorn, B. Drug Mental disorders in primary care: Prevalence encouraging a brain network perspective. United Nations International Drug Control Categorical and dimensional models of Treating obsessive-compulsive disorder. A supplement to mental health: A report of study of serotonin 1B receptor (A-161T) Tuthill, R. The Harvard Twin approach to the treatment of personality tightness from no apparent cause: Lynn. A meta-analysis neuroanatomical, and neurophysiological Standards for privacy of individually of the treatment of panic disorder with or measures. Department of Health and Human to fat and normal male and female stimulus disorder. Prevalence and construct validity of compulsive disorder, panic disorder, and Van Velzen, C. The Wernicke-Korsakoff syndrome for social anxiety disorder (social phobia): A assessment of the generalization of exposureand related neurological disorders due to meta-analysis of randomized controlled trials. Dynamically spreading frontal brain imaging and pharmacotherapy in psychiatric patients. A prospective study somatization among Latino patients in healthy unrelated volunteers. Verbal Psychotherapy and the role of the and nonverbal neuropsychological test environment. Neuro-Psychopharmacology & Biological Social skills deficits in schizotypal Volkow, N. The New model on its therapeutic actions for Treatment for the initial acute phase of firstgenetics of attention deficit hyperactivity attention-deficit/hyperactivity disorder. Developmental changes in cortisol studies of major depression: Variable, Acta Psychiatrica Scandinavica Supplement, secretion in normal and at-risk youth. Attending to the omissions: A historical (hypochondriasis) in a routine clinical setting. Changes and increases the prolactin response to in the United States: Results from the in binge drinking and related problems d-fenfiuramine in women but not men. British Medical Journal, 331, college students: A comparison of California Guilford Press. New York: Basic natural experimental method for separating Medication noncompliance in schizophrenia: Books. John Lennon interview Cortical maldevelopment, antipsychotic in maternal depression and child with Rolling Stone magazine. Children with prepubertalcognitive therapy for borderline personality psychosis treated with olanzapine. Understanding Developmental psychopathology and culture: alcohol, and other drug use. Journal of Drug cross-cultural prognostic variability for Ten lessons from Thailand. Journal of Clinical cohesion, religiosity and general emotional Cambridge University Press. Affective and adoptive families of adopted individuals multidimensional meta-analysis of treatments disorders. The virtual cutting edge: tectonics in the classification of personality Westerlund, E. Columbia University College of dangerous offenders: Law, justice, and culturally based variables associated with Physicians and Surgeons, Continuing Medical therapy (pp. A videotape intervention to enhance comprehensive system for the Rorschach: A the informed consent process for medical comment on Gacono, Loving, and Bodholdt; Wilson, G. Results from an exploratory Nervous and Mental Disease, 190, trial in schizophrenia. Urban/rural and gender differentials Journal of Consultation and Liaison Sorri, A. The pain of being borderline: cytokines in chronic and treatment-resistant examination of client attitudes towards Dysphoric states specific to borderline patients with schizophrenia: Association online counseling. Hypoxic-ischemia-related schizophrenia in Swedish conscripts of 1969: Potentially inappropriate medication use in fetal/neonatal complications and risk of Historical cohort study. Reprinted permission of the American Medical principles of psychologists and code by permission of HarperCollins Association from the Journal of the of conduct.
Insight in gestalt psychology is oriented towards problem solving in the external world erectile dysfunction pills review cheap aurogra 100mg on line, whereas insight in clinical practice is inner-directed latest erectile dysfunction medications generic aurogra 100mg fast delivery. David (1990) regards insight as composed of three distinct erectile dysfunction treatment natural generic 100 mg aurogra, overlapping dimensions erectile dysfunction causes n treatment buy aurogra paypal, namely erectile dysfunction protocol ingredients buy discount aurogra 100 mg online, the recognition of morbid psychological change erectile dysfunction with age statistics discount aurogra 100mg free shipping, the labelling of this change as deriving from mental illness and the understanding that this change requires treatment that needs to be complied with. An assessment schedule was constructed for determining the nature of insight, and quantitative loss of insight correlated with the degree of psychopathology (David et al. One of the most frustrating aspects of practising psychiatry is, from the point of view of the treating professional, the apparent inability of patients to recognize and/or admit that they are mentally ill. Patients, especially those with schizophrenia, often deny that their experiences are abnormal and that they are unwell. I do not dispute that in many of these cases one may be dealing with mere hallucinations, as which they are treated in the mentioned textbook. Furthermore Schreber continues: Science seems to deny any reality background for hallucinations In my opinion this is defnitely erroneous, at least if so generalized. These quotations from Daniel Schreber demonstrate one of the most complex aspects of the nature of insight. This is the capacity to have an attitude towards abnormal experiences in others where one can recognize them as pathological, but to deny the abnormality of the experience in oneself, and to designate it as not being evidence of mental illness. The resulting refusal to cooperate with treatment and rehabilitation causes long-term suffering for the patients and their carers. It is this capacity of patients to understand their own illness that is evaluated clinically in insight. In recent years, there has been a resurgence of interest in the concept, with attempts to defne it reliably and quantifably and to study its correlates (Kumar and Sims, 1998). In gestalt psychology, insight is conceived as a sudden, unexpected solution to a problem. In essence, in gestalt psychology, insight is by defnition related to a specifc task, a problem that stands in need of solution in the external world. Furthermore, there has been extensive debate within gestalt psychology about the nature of insight, whether it is a unique human facility that is also a specifc cognitive skill. The fact that, in gestalt psychology, insight refers to a problem in the external world distinguishes it from the concept of insight in clinical practice. In clinical practice, insight focuses on understanding of changes or happenings within an individual. Thus, for Jaspers insight becomes manifest only when the patient is able to turn away from the content of his psychic experiences towards making a judgement about it and inquiring into its causes and reasons. Freud (1981) used the term insight to denote knowledge of illness but, on the whole, in psy choanalytic therapy the development of a deeper awareness of self is considered to be the goal of treatment. David (1990) has proposed that insight is composed of the three overlapping dimensions described above. It has been suggested that parallels can be drawn between the loss of insight in psychiatric patients and the loss of awareness of disease of parts of the body in certain neurological conditions. In cortical blindness, left-sided hemiplegia following stroke and amnesic syndrome, lack of awareness of disease is well recognized. There is a difference, though, between the lack of insight seen in psychiatry and the lack of awareness seen in neurological disease. Nonetheless, even though the lack of insight in psychiatry and lack of awareness of disease in neurology are not identical, it may be that comparisons may point to possible neurobiological bases that they share in common. There are certain philosophical problems when we consider insight in patients with psychosis. People without any psychiatric illness vary in their ability to know themselves and the consequences of their personalities. Because at least some conceptualizations of psychosis rely on the lack of insight as a defning feature, discussion concerning the concept can become circular. Added to this is the fact that varying degrees of insight can occur and that non-verbalization of insight may be different from the lack of it. This works for as long as the clinician recognizes that it is merely a way of speaking, not necessarily an accurate representation of how self-monitoring takes place. Tolor and Reznikoff (1960) developed a test using hypothetical situations based on common defence mechanisms and found a correlation with intelligence. This test was used by Roback and Abramowitz (1979), who found a correlation in those with schizophrenia between greater subjective distress and better behavioural adjustment. The validity of this test for general clinical work is affected by the concept of insight being based on psychodynamic rather than psychopathological features. Using this questionnaire, they found no correlation with aspects of acute psychopathology. The Schedule for Assessment of Insight in Psychosis was published in 1992 (David et al. There were seven items with a maximum possible score of 14 and an additional item on hypothetical contradiction. The Scale to Assess Unawareness of Mental Disorder (Amador and Strauss, 1993) is a much more comprehensive scale with six general items and four subscales, from which ten summary scores can be calculated. The scale by Markova and Berrios (1991) is more directed to evaluating aspects of self-awareness and less to clinical defnition of insight with regard to illness. They found that patients failed to acknowledge negative symptoms and failed to view positive symptoms as evidence of mental illness. From earlier impressionistic assessments of a global nature, measurement of insight has more recently progressed to the use of operationalized defnitions and standardized instruments. Although the different instruments might be measuring different aspects of a complex phenomenon, there is at least the freedom to choose one to suit specifc clinical or research aims. There is an inverse correlation between insight, the severity of psychopathology and positive affective disturbance (Sanz et al. They speculated whether the mechanisms underlying the production of positive symptoms and disturbed insight were independent and whether the latter was more resistant to the effective use of neuroleptic medication. Overall, it does appear that the relationship between poor insight and aspects of psychopathology is not linear but complicated by other factors, including compliance with treatment. Insight and Cognitive Impairment It has often been speculated that poor insight may have a neurological basis. This item had been shown by factor analytical studies to be a member of the component composed of symptoms of cognitive impairment such as cognitive disorganization, poor attention, stereotyped thinking and poor abstract thinking. However, using a different methodology, Kemp and David (1996) failed to show a relationship between insight and neuropsychological defcits. It is possible that chronicity of the illness could be an additional variable, which predisposes to cognitive impairment. However, the study did not use any of the standard rating scales to measure insight. Additionally, it is becoming clearer that insight correlates with indices of cognitive functions including measures of error monitoring, empathy and theory of mind (Pegaro et al. However, on balance, the exact nature and extent of these relationships is still unresolved. As in other clinical situations, the relationship may not be a straightforward one, as other variables, such as the chronicity of illness, treatment factors, and gender may all be involved. Firstly, greater insight seems to predict hopelessness, depression and suicide (Ampalam et al. Awareness of the adverse social implications of mental illness may be the mediating factor between insight and depression (Thomas et al. Amador and Strauss (1993) also found their measures of insight to be correlated with the course of the illness. The relationship between poor insight and poor compliance with treatment has been shown by Bartko et al. The balance of evidence seems to be that higher levels of awareness of having an illness are associated with better medication compliance and clinical outcome (Amador et al. However, there is a risk of circularity of logic, in that some of the measures of insight are based on defnitions of insight that include non-compliance. Moreover, compliance with prescribed treatment is a much more complex phenomenon affected by social factors and beliefs about health and sickness (Bebbington, 1995). It is also possible that the relationship between compliance and different aspects of insight may be different. It is interesting that patients may comply with treatment, even though they do not believe themselves to be ill, if the social milieu is conducive (McEvoy et al. The role of health beliefs and illness representation in determining compliance with treatment is recognized, but how these interact with insight to infuence treatment compliance has yet to be studied. The domains of illness representation are identity (the label of the disease), causes (explanatory models), timeline (onset and anticipated duration), control (belief that self can infuence outcome) and consequences (functional as well as other consequences) (Brownlee et al. What is obvious is that insight is not the only determinant of care-seeking and treatment adherence. This was further studied by Lysaker and Bell (1995) on a sample of patients with a diagnosis of schizophrenia or schizoaffective disorder. In their study reported in 1995, patients enrolled in vocational rehabilitative programmes were found to have improved insight after fve months. This improvement was greater for patients with comparatively few cognitive defcits, echoing their earlier fndings regarding a relationship with cognitive impairments. It does seem an interesting suggestion that vocational rehabilitation can favourably affect insight in the absence of cognitive impairment. However, as in schizophrenia, poor insight was correlated with involuntary admission. They found a qualitative difference between mania and schizophrenia, in that patients with schizophrenia but not mania had reduced awareness of features of their illness. However, although the manic patients were aware of their symptoms, they did not agree that these emanated from a mental illness. The former found that severely manic patients were similar to patients with schizophrenia on scores of insight, whereas depressed and schizoaffective patients had more insight. In conclusion, it seems to be that both schizophrenia and bipolar disorder patients have impaired insight and the mediating factors may be severity of symptoms and cognitive impairment, especially working memory impairment (Varga et al. Medical anthropologists have criticized the concept of insight for failing to recognize that people can have various culturally shaped frameworks to explain their illnesses, all possibly valid. Johnson and Orrell (1995) have reviewed work by social scientists on cultural and social variations in lay perceptions of mental illness and argue that these would infuence insight. Social and cultural backgrounds infuence perceptions of stigma from mental illness and the congruence of the patients with Western medical views of mental illness. The ability to relabel mental phenomena as abnormal may be less infuenced by social factors when compared with beliefs about the causation of mental illness. Although there are very few studies in this area, evidence seems to be emerging that social and cultural factors are important in the diagnosis of poor insight. For example, differences in the ethnic background of the psychiatrist and the patient appear to infuence the judgement of the former about insight (Johnson and Orrell, 1996). It has been suggested that refusal to take prescribed medication, implying poor insight, is a wilful preference for the experience of psychotic phenomenology over drug-induced normality. The second formulation suggests that patients deny illness at a psychological level to help them cope with normal life as they recover from a psychosis. A third explanation has suggested that poor insight may have something to do with cognitive impairment, drawing on similarities with neurological conditions such as anosognosia. And, a fourth explanation is that disruption of neural mechanisms and networks underlying selfand other-monitoring are involved. In a recent study, schizophrenia patients demonstrated less activation in the posterior cingulate cortex in the selfand other-refection conditions and less activation in the precuneus in the other-refection condition compared with healthy controls. Better insight was associated with greater response in the inferior frontal gyrus, anterior insula, and inferior parietal lobule during self-refection.
Inability to achieve orgasm (in men erectile dysfunction treatment in vadodara order generic aurogra, to ejaculate) following a period of sexual excitement judged adequate in intensity and duration to produce such a response erectile dysfunction causes mental order aurogra 100 mg online. Ejaculation occurs with minimal sexual stimulation or before erectile dysfunction treatment aids cheap aurogra 100mg free shipping, on what causes erectile dysfunction in 30s order cheap aurogra online, or shortly after penetration and before the individual wishes it erectile dysfunction jacksonville best aurogra 100 mg. Fear or anxiety in anticipation of vaginal penetration erectile dysfunction 60 aurogra 100mg fast delivery, with tensing or tightening of the pelvic floor muscles. Common Nursing Diagnoses and Interventions for Paraphilic Disorders And Sexual Dysfunctions (Interventions are applicable to various health-care settings, such as inpatient and partial hospitalization, community outpatient clinic, home health, and private practice. Client will identify stressors that may contribute to loss of sexual function within 1 week. Client will discuss pathophysiology of disease process that contributes to sexual dysfunction within 1 week. Client will verbalize willingness to seek professional assistance from a sex therapist in order to learn alternative ways of achieving sexual satisfaction with partner by (time is individually determined). Long-term Goal Client will resume sexual activity at level satisfactory to self and partner by (time is individually determined). This establishes a database from which to work and provides a foundation for goal setting. Help the client determine time dimension associated with the onset of the problem and discuss what was happening in his or her life situation at that time. Depression and fatigue decrease desire and enthusiasm for participation in sexual activity. Encourage the client to discuss the disease process that may be contributing to sexual dysfunction. Ensure that the client is aware that alternative methods of achieving sexual satisfaction exist and can be learned through sex counseling if he or she and the partner desire to do so. Client may be unaware that satisfactory changes can be made in his or her sex life. Increasing knowledge and correcting misconceptions can decrease feelings of powerlessness and anxiety and facilitate problem resolution. Complex problems are likely to require assistance from an individual who is specially trained to treat problems related to sexuality. Support from a trusted nurse can provide the impetus for them to pursue the help they need. Client is able to correlate physical or psychosocial factors that interfere with sexual functioning. Client is able to communicate with partner about their sexual relationship without discomfort. Client and partner verbalize willingness and desire to seek assistance from a professional sex therapist. Client verbalizes resumption of sexual activity at level satisfactory to self and partner. Client will verbalize aspects about sexuality that he or she would like to change. Client and partner will communicate with each other ways in which each believes their sexual relationship could be improved. Knowledge of what client perceives as the problem is essential for providing the type of assistance he or she may need. The relationship with his or her partner may deteriorate as individual eventually gains sexual satisfaction only from variant practices. Note cultural, social, ethnic, racial, and religious factors that may contribute to conflicts regarding variant sexual practices. The client may be unaware of the influence these factors exert in creating feelings of discomfort, shame, and guilt regarding sexual attitudes and behavior. The client is more likely to share this information if he or she does not fear being judged by the nurse. Assist the therapist in a plan of behavior modification to help the client who desires to decrease variant sexual behaviors. Individuals with paraphilic disorders are treated by specialists who have experience in modifying variant sexual behaviors. Nurses can intervene by providing assistance with implementation of the plan for behavior modification. If altered sexuality patterns are related to illness or medical treatment, provide information to the client and partner regarding the correlation between the illness and the sexual alteration. Explain possible modifications in usual sexual patterns that client and partner may try in an effort to achieve a satisfying sexual experience in spite of the limitation. The client and his or her partner may be unaware of alternate possibilities for achieving sexual satisfaction, or anxiety associated with the limitation may interfere with rational problem solving. Explain to client that sexuality is a normal human response and does not relate exclusively to the sex organs or sexual behavior. Client is able to verbalize fears about abnormality and inappropriateness of sexual behaviors. Client expresses desire to change variant sexual behavior and cooperates with plan of behavior modification. Client and partner verbalize modifications in sexual activities in response to limitations imposed by illness or medical treatment. Client expresses satisfaction with own sexuality pattern or satisfying sexual relationship with another. Adolescents rarely have the desire or motivation to alter their cross-gender roles, and disruptive behaviors are not Sexual Disorders and Gender Dysphoria 243 uncommon. Some adults seek therapy to learn how to cope with their altered sexual identity, whereas others have direct and immediate request for hormonal therapy and surgical sex reassignment. The true transgendered individual intensely desires to have the genitalia and physical appearance of the assigned gender changed to conform to his or her gender identity. This change requires a great deal more than surgical alteration of physical features. In most cases, the individual must undergo extensive psychological testing and counseling, as well as live in the role of the desired gender for up to 2 years before surgery. Treatment of children with gender dysphoria may be initiated when the behaviors cause signifcant distress and when the client desires it. One type of treatment suggests that they should be encouraged to become satisfed with their assigned gender. Behavior modifcation therapy serves to help the child embrace the games and activities of his or her assigned gender and promotes development of friendships with same gender peers. Another treatment model suggests that children who have problems with gender identity are dysphoric only because of their image within the culture. Some professionals are recommending pubertal delay for adolescents aged 12 to 16 years who have suffered with extreme lifelong gender dysphoria, and who have supportive parents that encourage the child to pursue a desired change in gender (Gibson & Catlin, 2010). A gonadotropin-releasing hormone agonist is administered, which suppresses pubertal changes. The treatment is reversible if the adolescent decides later not to pursue the gender change. When the medication is withdrawn, external sexual development proceeds, and the individual has avoided permanent surgical intervention. However, issues associated with mental health concerns, such as depression, anxiety, social isolation, anger, self-esteem, and parental confict, must be addressed, even if the client elects not to proceed with the behavior modifcation approach. Studies of genetics and physiological alterations have been conducted in an attempt to determine whether or not a biological predisposition to problems with gender identity exists. It appears that family dynamics may play an influential role in the etiology of gender disorders. In a 2003 study, Zucker and associates found a high rate of psychopathology and family dysfunction in children with gender dysphoria. Maternal depression and bipolar disorder was frequently demonstrated, whereas fathers often exhibited depression and substance use disorders. The authors recommended that parental conficts and psychopathology must be given careful consideration as an aspect in childhood gender dysphoria. This theory suggests that gender identity problems begin during the struggle of the Oedipal/Electra conflict. Strong desire to participate only in the stereotypical games and pastimes of the opposite gender. Stated conviction that one has the typical feelings and reactions of the opposite gender. Persistent discomfort with or sense of inappropriateness in the assigned gender role. Common Nursing Diagnoses and Interventions for Gender Dysphoria (Interventions are applicable to various health-care settings, such as inpatient and partial hospitalization, community outpatient clinic, home health, and private practice. Client will verbalize knowledge of behaviors that are appropriate and culturally acceptable for assigned gender. Client will verbalize desire for congruence between personal feelings and behavior and assigned gender. Client will demonstrate behaviors that are appropriate and culturally acceptable for assigned gender. Client will express personal satisfaction and feelings of being comfortable in assigned gender. Trust and unconditional acceptance are essential to the establishment of a therapeutic nurse-client relationship. Be aware of own feelings and attitudes toward this client and his or her behavior. The nurse must not allow negative attitudes to interfere with the effectiveness of interventions. It is important to know how the client perceives the problem before attempting to correct misperceptions. Discuss with the client the types of behaviors that are more culturally acceptable. Practice these behaviors through roleplaying or with play therapy strategies. Positive reinforcement or social attention may be given for use of appropriate behaviors. To preserve selfesteem and enhance self-worth, the child must know that he or she is accepted unconditionally as a unique and worthwhile individual. Client demonstrates behaviors that are culturally appropriate for assigned gender. Client demonstrates development of a close relationship with the parent of the same gender. Long-term Goal Client will interact with others using culturally acceptable behaviors. Once client feels comfortable with the new behaviors in role playing or one-to-one nurse-client interactions, the new behaviors may be tried in group situations. Presence of a trusted individual provides security for the client in a new situation.
Buy aurogra with a mastercard. Erectile Dysfunction: The Deadly Lie & Simple Cure.