Gary W. Chune, MD
- Assistant Professor of Internal Medicine
- Division of Endocrinology, Scott & White Hospitals,
- Texas A&M Health Sciences Center
- Temple, Texas
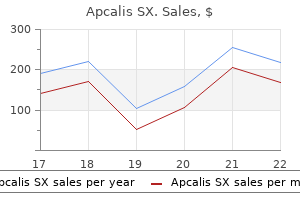
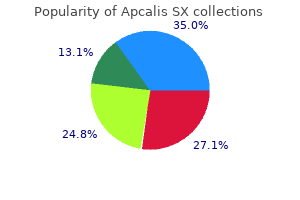
Ventriculomegaly occurs in 9?18% of infants with trisomy 21 cheap erectile dysfunction pills uk purchase apcalis sx from india, 18 impotence lower back pain discount 20mg apcalis sx otc, 13 erectile dysfunction pills cvs 20mg apcalis sx with mastercard, fragile X erectile dysfunction treatment purchase 20 mg apcalis sx, and triploid infants erectile dysfunction treatment machine generic 20mg apcalis sx overnight delivery. Toxoplasmosis may present with ventricu lomegaly and is sometimes treatable in utero with potential salvage of fetal neurologic development impotence penile rings cheap 20 mg apcalis sx. If patients are unwilling to risk pregnancy loss by amniocentesis before 24 weeks gestation, later amniocentesis at about 34 weeks gestation should be considered. Amniocentesis at this time risks only preterm emergency delivery, will usually allow chromosomal determination in time to optimize delivery management, and may facilitate management of the neonate after birth. Choroid cysts appear as single or multiple 2 to 5-mm cysts and may be unilateral or bilateral. Choroid cysts resolve in 90% of patients by 26?28 weeks gestation regardless of karyotype, and their resolution does not indicate any decreased association with aneuploidy. Aneuploid karyotypes have been reported in 8% of infants with choroid cysts (1% aneuploidy in cases of isolated cysts but 46% aneuploidy if other anomalies are present). Choroid cysts occur in 47% of infants with trisomy 18, and with lesser frequency in trisomy 21 (8%) and trisomy 13 (2%). As isolated abnormalities, the risk of trisomy 18 for choroid cysts does not exceed 1/280 until the maternal age is 40 or greater (the risk at age 40 is 1/238). Counseling for patients with fetal choroid cysts varies by maternal age and the ability to accurately detect other sonographic? The potential for falsely low risk assessments due to false negative sonographic screening should be discussed with patients during the process of their evaluation. In cases of isolated choroid plexus cysts, amniocentesis has var iously been recommended as a consideration for women 32 years and older (Guptaetal. Anencephaly should be suspected if images of the fetus show it to be closely approximated to the uterine wall and clear views of the head above the level of the lower and central face and orbits cannot be obtained. Isolatedprotrusionofonlymeningealstructuresistermedmeningocele, while involvement or the encephalon as well is termed encephalocele. Cephaloceles usually result from failure of closure of the rostral end of the neural tube during the fourth week of gestation but may also result from disruption by amniotic bands, or as a component of autosomal recessive con ditions such as Meckel-Gruber, Robert, Chemke-Knoblock, cryptophthalmus syndromes,andindyssegmentaldwar? Theyareusuallylocatedinthemid line anteriorly or posteriorly, although those associated with amniotic bands may be asymmetric and occur in atypical locations. Posterior encephaloceles sometimes present as masses in the posterior neck and should be distinguished from cystic hygroma and meningocele in the neck. Evaluation of the face in coronal and sagittal planes aids in evaluation of encephaloceles and oral clefts (Figures 4. Occipital cephaloceles often are not easily seen on views of the cerebral cross section but may be detected when the posterior fossa is evaluated. Temporal bulging of cranial structures found in the cloverleaf skull of thanatophoric dysplasia has been falsely diagnosed as an encephalocele. Cephaloceles are often accompanied by hydrocephaly (seen in 60?80% of posterior lesions and 20% of anterior lesions) or spina bi? Almost 50% of infants with isolated meningoceles have nor mal development after surgical repair of their defects, while fetuses with large amounts of brain protruding out of the skull have a very poor prognosis. Nostrils can be visualized just above and it is believed that minimization of birth trauma may improve neonatal the lips. It is present in 1/5,000 to 1/16,000 live born infants and in up to 1/250 conceptuses. Holoprosencephaly often is found in asso ciation with hydrocephaly or in combination with severe distortions of the overall cerebral sonographic architecture or with structural facial abnormal ities. Holoprosencephaly is common (present in up to 50%) in fetuses with karyotypic abnormalities such as trisomy 13, trisomy 18, triploidy, 13q-, and 18p-. Aneuploidy is found in 4% of cases of isolated holoprosencephaly but in 39% of cases if other abnormalities are present. Itoccurs more often in cases of maternal diabetes (a 200-fold increased risk) and is also a commonly observed feature of numerous syndromes, including Pallister-Hall syndrome, Kallman syndrome, Meckel-Gruber syndrome, Vasadi syndrome, and camptomelic dysplasia. The prognosis for alobar and semilobar holopros encephaly is very poor, as most infants die at birth or within 1 year of life. If a prior infant had holoprosencephaly unrelated to karyotypic abnormalities, the estimated recurrence rate is 6%, although some families appear to exhibit either autosomal recessive (25% recurrence) or dominant (50%) inheritance. The shape of the skull may offer important clues about underlying fetal disorders. Some fetuses display a cross-sectional skull shape reminiscent of a lemon (the lemon sign), which results from bilateral frontoparietal narrowing of the skull. Fetuses with excessively round skull morphology, brachycephaly, are at in creased risk of trisomy 21. Hypoplasia of the facial bones may result in proportionately narrowed ante rior skull dimensions, giving the skull a strawberry shaped appearance (straw berry skull). Although fetuses with head circumferences less than the 10th centile usually have excellent outcomes, those with more severe restriction of head size, mi crocephaly, do not. Microcepahaly is strongly associated with adverse neonatal outcomes and is a clinically useful marker for underlying aneuploidy, hered itary conditions, in utero infection, teratogen exposure, and radiation injury. Twenty percent of microcephalic fetuses have karyotypic abnormalities and trisomy 13 is the most common chromosomal abnormality found. The posterior fossa view offers a cross-sectional assessment of the cisterna magna,cerebellum,andtheposteriornuchalfold,whichcanbemeasuredfrom this plane (Figure 4. The plane of imaging is highly angle dependent, and improper tangential images may yield falsely elevated cisterna depths of 13 mm or more. The cerebellum can be nicely visualized and the nuchal thickness measured in this same plane. The cisterna magna ranges from 1 to 10 mm in depth over gestational age from 15 to 36 weeks and from 4 to 10 mm at term. Decreased cisterna magna depths may result from herniation of the brainstem down the spinal canal, whichmayoccurinassociationwithneuraltubeabnormalities. Cisternamagna depths of less than 3 or 4 mm suggest the possibility of open neural tube defects Falx Calvarium A B Cisterna magna Cerebellum 4. Cisterna magna depths > 11 mm in rare cases may be a normal variant and sometimes result from inappropriate imaging with excessive angulation of the ultrasound imaging plane. Forty percent of fetuses with excessively deep cisterna magna have been found to be aneuploid (most with trisomy 18). Posterior fossa cysts are present in 10% of infants with trisomy 18, 15% of those with trisomy 13, 1% of those with trisomy 21, and in 6% of infants with triploidy. The cerebellum normally has a bilobed or dumb-bell shaped appearance, but in cases of neural tube abnormalities, it may assume a fused appearance similar in shape to a banana (the banana sign). Cerebellar transverse diameter varies with gestational age and can be affected by fetal growth retardation. The cerebellar vermis can also be viewed in a similar imaging plane but may not be easily imaged in many patients. Dandy-Walker malformations are characterized by partial or complete ab sence of the cerebellar vermis and a characteristic cystic dilation of the fourth ventricle often accompanied by hydrocephaly. The Dandy-Walker anomaly is associated with a variety of underlying conditions, including autosomal reces sive conditions such as Aicardi syndrome, Meckel-Gruber syndrome, Walker Warburgsyndrome;aneuploidy(trisomy18);infectionssuchastoxoplasmosis, cytomegalovirus, and rubella; maternal diabetes, exposure to compounds such as coumadin and ethanol, agenesis of the corpus callosum, porencephaly, and schizencephaly. Increased nuchal thickness is an important marker of aneuploidy and is perhaps the only commonly observed minor sonographic? In the second and third trimesters, the nuchal fold is best measured in the same plane used to evaluate the posterior fossa. Caremustbetakentoobtainanoptimalimagingplane,becauseestimates of the nuchal fold width and cisterna magna depth vary widely if inaccurate images are created. Inadequate angulation relative to the axial plane will re sult in falsely low estimates of these characteristics, while excessive angulation will result in falsely large estimations. In practice, the best estimates of these parameters will be obtained from images that optimally image the cerebellum. Nuchal thickness greater than 6 mm at 15?23 weeks gestation are associated with trisomy 21 and other aneuploidies and are also associated with increased risk for cardiovascular malformations (Bahado-Singh et al. Unfor tunately (for purposes of aneuploidy screening), nuchal thickness gradually increases over this range of gestational ages in normal pregnancies. It is optimally imaged in a sagittal plane with the fetal head in a neutral position (not? Unfortunately, measurements of this characteristic are very prone to opera tor variation, and this technical issue has limited the general applicability of early pregnancy nuchal thickness screening. The association be tween increased nuchal translucency and aneuploidy is also valid in multiple gestations. As a result, nuchal lucency screening offers a means of antenatal aneuploidy screening in multiple gestation not offered by standard serologic methods such as maternal serum triple or quadruple marker screening, which, for the most part, are confounded by problems engendered by assessing the risk of aneuploidy in two fetuses from the same pooled maternal serum sample. In chromosomally normal infants, other potential infectious causes such as toxoplasmosis, parvovirus, and coxsackievirus B should be considered. It occurs in about 1/6,000 pregnancies and usually presents as bilateral, asymmetric, thin-walled, often multiseptate cystic masses located posterior and lateral to the high cervical vertebrae. Cystic hygromas may represent normal developmental events but usually re sult from aberrant development due to aneuploidy or early infections. They are most commonly found in association with aneuploidy (monosomy X, trisomy 21, trisomy 18). Cystichygromasduetoaneuploidyorinfectionhaveahigh propensity for fetal demise in utero. Avarietyofothertumorsoftheneckareoccasionallyencountered,including thyroid goiter, hemangiomas, teratomas, branchial cleft cysts, lipomas,? Perhaps the most important of these from an obstetric perspective is fetal thyromegaly or goiter. The en larged thyroid usually presents as a solid, bilobed, homogenous mass in the anterior neck, and hydramnios (present in 30%) may occur due to impaired fetal swallowing. Delivery at a high-risk neonatal facility is recommended be cause of the high risk of airway obstruction at birth (Stocks et al. They result from a localized proliferation of vascular tissue that rarely presents as a discrete fetal neck mass. They usually have a complex sonographic ap pearance with many small vascular channels and an almost solid appearance. Close surveillance for hydrops, skin edema, ascites, and pleural effusion should be maintained, and newer methods of fetal cardiac assessment may be considered. Falken sammer and Huhta recently described the use of the Tei-index (isovolumetric time/ejection time) and a cardiac function score, which assessed 5 factors re lated to cardiac function (presence of hydrops, venous Doppler? Using these indices and serial evaluations, it may be possible to identify early fetal cardiac dysfunction, and institute therapy before overt failure is present. They are usually uni lateral and situated in the anterolateral portion of the neck, often presenting as cystic lesions that enlarge and increase in complexity over the course of preg nancy, sometimes achieving 8?10 cm in diameter. Untreated cervical teratomas have high mortality rates (80?100%), but oper ative mortality of 9?15% is not negligible. The presence of large neck masses may limit mobility of the neck, which in turn may contradict breech delivery. Large masses may also necessitate consideration of cesarean delivery for vertex presenting infants, as has been described for goiter and hemangiomas (Stocks et al. Clefting of the upper lip is relatively easy to assess, while abnormalities of the palate are more dif? If major chro mosomal abnormalities are suspected, care should be taken to exclude the pos sibility of central facial abnormalities. Measurement of inter and intraorbital diameters and careful evaluation of the nose and mouth are recommended. Fa cial clefts not due to underlying syndromic causes occur in about 1/800 births. They occur more often in males (60?80% male predominance) and are asso ciated with advanced maternal age. They occur more commonly in Asians and Native Americans and are uncommon in blacks. The association between facial clefts and aneuploidy varies by the timing of the evaluation. Aneuploidy is found in up to 40% of antepartum evaluations for facial clefting (usually either trisomy 13 or 18) but in only 1% of newborns with facial clefts. Clefting is found in 40% of infants with trisomy 13, 10% of infants with trisomy 18, and in 1?2% of infants with either trisomy 21 or triploidy. These differences occur because of higher pregnancy wastage rates in aneuploid fetuses. The images should be evaluated to identify any bulging, sac-like protrusions, or if abnormal thickening of the skin pos terior to the spine is present, which might suggest a neural tube abnormality. Abdominal Sonography Evaluation of the abdomen should include documentation of the stomach bubble in its proper situs (and concordant with the heart in the thoracic cav ity). Inspection of the abdominal contents such as bowel lumen size, ascites, proper appearance of the umbilical cord insertion site, overall contours of the diaphragm and anterior abdominal wall, and appearance of the kidneys is rec ommended. The primary cross-sectional abdominal image should be obtained in a plane almost perpendicular to the major axis of the spine. The optimal image should include the stomach bubble and hepatic vein in an area close to (but not at) the umbilical cord insertion site and should not include cross sec tions of the heart, kidneys, bladder, or the actual umbilical cord insertion into the abdomen. This view is best localized by aligning the transducer with the spinal column, rotating the transducer 90? The stomach bubble is normally found situated on the left of the abdomen, caudad to the heart but with concordant situs. Esophagealatresia and other small bowel atresias are associated with aneuploidy (usually trisomy 21 and 18). Esophageal atresia is also associated with cardiac, gastrointestinal, and genito-urinary abnormalities. A right-sided stomach bubble suggests pos sible situs inversus or complete transposition of the great vessels (depending on cardiac situs). The size of the stomach increases with fetal swallowing activity and by ges tational age.
Cyanosis restricted to the upper half of the body is seen occasionally in patients with pulmonary hypertension erectile dysfunction due to diabetes order 20mg apcalis sx with amex, patent ductus arteriosus impotence hypertension medication purchase 20 mg apcalis sx visa, coarctation of the aorta erectile dysfunction 19 years old cheap apcalis sx 20mg mastercard, and D-transposition of the great arteries shakeology erectile dysfunction cheap apcalis sx online amex. An infant of a diabetic mother has increased risk of hypoglycemia erectile dysfunction medicine from dabur order apcalis sx 20mg with amex, polycythemia erectile dysfunction over the counter medication apcalis sx 20mg lowest price, respiratory distress syndrome, and heart disease. Infection, such as that which can occur with premature rupture of membranes, may cause shock and hypotension with resultant cyanosis. Amniotic fluid abnormalities, such as oligohydramnios (associated with hypoplastic lungs) or polyhydramnios (associated with esophageal atresia), may suggest a cause for the cyanosis. Congenital defects (eg, diaphragmatic hernia, hypoplastic lungs, lobar emphysema, cystic adenomatoid malformation, and diaphragm abnormality). Periventricular-intraventricular hemorrhage, meningitis, and primary seizure disorder can cause cyanosis. Neuromuscular disorders such as Werdnig-Hoffmann disease and congenital myotonic dystrophy can cause cyanosis. Respiratory depression secondary to maternal medications (eg, magnesium sulfate and narcotics). Choanal atresia is nasal passage obstruction caused most commonly by a bony abnormality. Other causes are laryngeal web, tracheal stenosis, goiter, and Pierre Robin syndrome. In peripheral cyanosis, the skin is bluish but the oral mucous membranes will be pink. The liver can be enlarged in congestive heart failure and hyperexpansion of the lungs. Check for apnea and periodic breathing, which may be associated with immaturity of the nervous system. Observe the infant for seizures, which can cause cyanosis if the infant is not breathing during seizures. With cyanotic heart disease, the PaO2 most likely will not increase significantly. If the PaO2 rises above 150 mm Hg, cardiac disease can generally be excluded but not always. Failure of PaO2 to rise above 150 mm Hg suggests a cyanotic cardiac malformation, whereas in lung disease the arterial oxygen saturation should improve and go above 150 mm Hg. Draw a simultaneous sample of blood from the right radial artery (preductal) and the descending aorta or the left radial artery (postductal). If there is a difference of >15% (preductal > postductal), then the shunt is significant. It is sometimes easier to place two pulse oximeters on the infant (one preductal-right hand; one postductal-left hand or either foot). To confirm the diagnosis, a spectrophotometric determination should be done by the laboratory. Transillumination of the chest (see p 169) should be done on an emergent basis if pneumothorax is suspected. It can also help diagnose heart disease by evaluating the heart size and pulmonary vascularity. The heart size may be normal or enlarged in hypoglycemia, polycythemia, shock, and sepsis. Increased arterial markings can be seen in truncus arteriosus, single ventricle, and transposition. Increased venous markings can be seen in hypoplastic left heart syndrome and total anomalous pulmonary venous return. It is very helpful in identifying patients with tricuspid atresia; it will show left axis deviation and left ventricular hypertrophy. Echocardiography should be performed immediately if cardiac disease is suspected or if the diagnosis is unclear. Ultrasonography of the head can be performed to rule out periventricular-intraventricular hemorrhage. If a tension pneumothorax is present, rapid needle decompression may be needed (see also p 293). Order stat laboratory tests (eg, blood gas levels, complete blood cell count, and chest x ray film). Treat the infant with methylene blue only if the methemoglobin level is markedly increased and the infant is in cardiopulmonary distress (tachypnea and tachycardia). Administer intravenously 1 mg/kg of a 1% solution of methylene blue in normal saline. It is important to prepare the family in advance, if possible, for the death of an infant and to be ready to answer questions after the event. Early neonatal death describes the death of a live born infant during the first 7 completed days of life. Late neonatal death refers to the death of a live born infant after 7 but before 28 completed days of life. Usually several immediate family members in addition to the parents are present at the hospital. It is good practice to ensure that there is a contact telephone number available for any sick infant. If the family members are not present, telephone contact must be made as soon as possible to alert the family that their infant is dying or has already passed away. The religious needs must be respected and the necessary support provided (eg, priest, rabbi, minister, or pastoral care). Every hospital has pastoral services, and it is useful to inform the minister in advance because some parents may request that their child be baptized before death. It is important to remember that the infant may continue with a gasp reflex for a while even without spontaneous respiration and movement. The heartbeat may be very faint; therefore, auscultation for 2-5 min is advisable. Examination of the infant by the physician to determine death may be done in that same private area, with the family. Much of the equipment (eg, intravenous catheters and endotracheal tubes) may be removed from the infant unless an autopsy is anticipated. In that case, it is best to leave in place central catheters and possibly the endotracheal tube. This type of visual and physical contact is important to begin the grieving process in a healthy manner and try to relieve any future guilt. Parents and immediate family members should be in a quiet, private consultation room, and the physician should calmly explain the cause and inevitability of death. A brief outline of the normal grieving process may be discussed: shock, denial, sadness, anger, and reorganization. Staff must be aware of the additive stress on the parents looking in on a surviving twin. Family members should be asked whether they need any support for transport or funeral arrangements and whether they need a letter to the employer regarding time off from work and so on. Written permission should be obtained for the following: photography, mementos, autopsy, or biopsy. Occasionally, parents and immediate family members may have discussed organ donation before the death of the infant. If not, it can be brought up gently with the family, who will be given adequate time to reflect on it, taking into consideration the requirements for organ donation. Sometimes the parents may want to donate an organ, but this may not be possible because of the presence of infection or inadequate function of the organ before death. It is best to contact each state organ procurement organization to obtain specific information regarding organ donation. Autopsy can be a vital part of determining the cause of death and may be important in counseling the parents for future pregnancies. It is always a very sensitive issue to discuss with the parents, especially after the loss of their loved one. Parents should always be allowed adequate time to discuss this themselves and with the family if they have not already made up their minds. It is also important to note conversations with family members while the infant was dying, if not written earlier in separate notes. The physician declaring the infant dead initiates the death certificate, following strict guidelines for each county/ state. A telephone call from one of the medical team members should be arranged within the first week of death. A letter of sympathy can be sent out along with a brochure (eg, "Hello Means Good-Bye") that will help the family cope with the loss of a loved one. Another contact can be made at the end of the first month to comfort the family, share any further information, and answer questions. It is extremely important to discuss the arrangements for future counseling and refer the parents to high-risk obstetrics if appropriate. Parents should be allowed to grieve for the death of their child and should be given the opportunity to contact the physician at a later date, when they are more receptive emotionally. If consent for autopsy has been obtained, an autopsy follow-up conference after ~6-8 weeks is essential. This autopsy conference not only provides the parents with concrete information but also assists in the process of grieving. The obstetrician, pediatrician, and family physician should be notified of the death. Within the first 6-24 h of life, the most likely cause is conjunctivitis secondary to the use of ocular silver nitrate drops immediately after birth to prevent gonococcal ophthalmia. The organisms that most commonly cause conjunctivitis in the neonatal period are Neisseria gonorrhoeae and Staphylococcus aureus. Chlamydia trachomatis conjunctivitis is usually seen after the first week of life; it often presents as late as the second or third week. Pseudomonas aeruginosa infections are typically seen between the 5th and 18th days of life. Infection resulting from chlamydia may be watery early in the course and purulent later. Conjunctivitis in the neonate is either infectious (bacterial, viral, or chlamydial) or secondary to a chemical response. One study revealed that 56% of conjunctivitis cases were infectious (the most common being Chlamydia) and 44% were of uncertain origin. Other diagnoses that may mimic conjunctivitis and may need to be ruled out include foreign body, lacrimal duct obstruction, trauma to the eye, and glaucoma. Chemical conjunctivitis is usually secondary to the use of silver nitrate ocular drops. It is not seen as frequently as in the past because many nurseries now use erythromycin ophthalmic ointment, which causes less ocular irritation. The recommended topical prophylaxis with erythromycin will not prevent neonatal chlamydial conjunctivitis. Silver nitrate drops are recommended over erythromycin ophthalmic ointment if the patient population has a high number of penicillinase-producing N. It is considered a medical emergency because, left untreated, it can cause corneal perforation. It is the most frequent isolate, but it does not always cause conjunctivitis in infants who are colonized. Conjunctivitis will develop in approximately 25-50% of infants delivered vaginally to mothers with chlamydia. Remember that topical prophylaxis will not prevent neonatal chlamydial conjunctivitis. Pseudomonal conjunctivitis is usually a nosocomial infection and is becoming more common in neonatal nurseries. The organism thrives in moisture-filled environments such as respiratory equipment. It occurs most often in hospitalized premature infants or those with depressed immunity. Other bacterial infections include infections caused by Haemophilus spp, Streptococcus pneumoniae, and Enterococcus. The conjunctivitis can be superficial or may involve the deeper layers of the cornea. Herpes should be suspected if the conjunctiva is not responding to antibiotic therapy. The symptoms are persistent tearing and a mucoid discharge in the inner corner of the eye. Examine both eyes for swelling and edema of the eyelids, and check the conjunctiva for injection (congestion of blood vessels). A purulent discharge, edema, and erythema of the lids as well as injection of the conjunctiva are suggestive of bacterial conjunctivitis. A sample of the discharge should also be submitted for culture and sensitivity testing. Streptococci are gram-positive spherical cocci, and enterococci are gram-positive lancet-shaped encapsulated diplococci. If a chlamydial infection is suspected, material is gathered for Giemsa staining by scraping (not swabbing) the lower palpebral conjunctiva with a wire loop or blunt spatula to obtain epithelial cells. If chlamydial infection is present, typical cytoplasmic inclusion bodies will be seen within the epithelial cells. Rapid antigen detection assays on conjunctival scrapings can be sent to the laboratory for results. If herpes is suspected, a conjunctival scraping will show multinucleated giant cells with intracytoplasmic inclusions. Also, the conjunctiva should be swabbed and transported on special viral transport media for culture. Irrigate the eyes with sterile isotonic saline solution immediately and at frequent intervals (every 1-2 h) until clear.
Buy apcalis sx 20mg low cost. NoFap - Do You Still Have Erectile Dysfunction? (WATCH FULL VIDEO).
Also if severe: erosions erectile dysfunction 70 year olds discount apcalis sx online amex, haemorrhagic crusting erectile dysfunction pump demonstration buy on line apcalis sx, lesions uncomfortable (not usually painful) erectile dysfunction desi treatment buy generic apcalis sx 20 mg. Not typical targets (eg red blotches) erectile dysfunction prescription drugs apcalis sx 20 mg overnight delivery, on trunk as well as acral impotence support group cheap 20mg apcalis sx mastercard, may be blistered erectile dysfunction 9 code purchase 20 mg apcalis sx free shipping. Lesions: 2 4 cm, erythematous, tender, especially on shins but also on thighs or forearms. Differential diagnosis: all produce circumscribed hair loss, but skin itself is abnormal? Treatment: mild steroids, urea creams, salicylic acid creams, etc Granuloma Annulare? Enlarge centrifugally, with beaded rim gradually flattening until it disappears without trace within 2 years? Disorder of haematoma formation: especially in eye, brain, skin, kidney and heart? Angiofibromas: appear from 3 10, firm, discrete red/brown telangiectatic papules, 1 10 mm, cheeks and chin? Periungual fibromas: smooth skin coloured excrescences emerging from the nail folds? Classically (but not invariably) seen with epilepsy and mental retardation (?zits, fits and nit-twits? Rare sorts: Collodion Baby, Bullous and non-bullous ichthyosiform erythroderma, lamellar ichthyosis, X-linked ichthyosis, Harlequin fetus Erythroderma? Management: monitor fluid balance, rest, nutrition (shedding lots of protein), Moisturiser, careful use of steroids, methotrexate, etc. Quantity (eg # of pads per day but ask why they change 1 per hour too much), double protection needed (eg tampon and pad), soaking through, etc? Age of menarche probably not a big deal were you significantly younger or older than friends? Menses: Frequency (normal 21 35 days) and duration (normal 3 7 days), regularity (some variation normal). Teenagers will often give their period length as first day without bleeding to first day of bleeding check understanding? Ovulation is 12 16 days before the start of the next period (determined by timing of the following period, not the prior period). Use narrow speculum for nulliparous, wider speculum for multiparous, and paediatric for child or sometimes post menopausal. Contraindications: History of ectopic pregnancy, breast cancer, liver disease or enzyme inducing drugs? Epidemiology: 20% of women report sexual abuse before 16, full intercourse reported by 4%. Sexual: Did anything sexually frightening happen to you as a child or young adult, have you ever been made to participate in sexual activity that made you feel uncomfortable. If very recent then nil by-mouth and collect all urine and toilet paper until forensic examination. If withdrawal bleed following, then there is enough oestrogen to produce an endometrium? Ovarian causes are uncommon: Polycystic ovarian syndrome, tumours, premature menopause? Investigation: Pregnancy Test -ive 5 day progesterone challenge: +ive withdrawal bleed? Oligomenorrhoea: infrequent periods: common in the young and the nearly menopausal. Younger: pregnancy, dysfunctional uterine bleeding (diagnosis of exclusion, no pelvic pathology, associated with anovulatory cycles. Red brown nodules on surface of ovaries and pelvic structures, and other sites (appendix, peritoneal scars, etc). Can develop large cysts, lined by endometrial stroma and glands and containing changed blood (chocolate cysts). Fluoxetine 20 mg only when symptoms occurring (30% remission, minimal side effects)? Debated remedies include evening primrose oil, Vitamin B6 (pyridoxine) in low dose (neuropathy in high dose)? Biological hypotheses include abnormal response to ovarian hormones, mineralocorticoid effects, prostaglandins, etc. Fix either in 95% ethyl alcohol for 20 30 minutes or cytofix sprayed from 20 30 cms. Screening should be yearly for 2 years from 20 (some advocate starting earlier if > 2 years since commencing regular sex but as cancer in this age group is very uncommon, it? Complex hyperplasia with atypia: crowded, folded gland in which the lining cells are pleomorphic with loss of polarity and increased nuclear cytoplasmic ratio. Where is the back: Feel laterally (brace hand other side), then walk hands across. Score of fetal heart rate, breathing movements, fetal movement, fetal tone and amniotic fluid volume. Serum levels, maternal age and gestational age are used to calculate the risk of neural tube defects and chromosomal abnormalities? If mosaic, skin cells in fetus closer to the babies karyotype than placental cells? These people to be chosen by the Abortion supervisory committee, with a view to expeditious access by any woman seeking an abortion. Reasons for killing: to end suffering, to protect the innocent, lesser of two evils, to express societal condemnation? Fetus has the same moral status: absence of a dividing line between a baby and a fetus does not show lack of difference? Complete abortion: Products of conception expelled, bleeding stopped, cervix closed (don? Septic Abortion: as for incomplete abortion + uterine and adnexal tenderness, purulent loss, pyrexia. Maternal illness, abnormalities of the uterus (eg cervical incompetence), immunological factors? Recurrent miscarriage = loss of 3 or more consecutive pregnancies, occurs in < 1% Ectopic pregnancy? Atypical some initially have a fetus proliferation proliferating trophoblast Little invasive potential 10% invasive, Most have metastasised at Choriocarcinoma 5% diagnosis. Even if tightly controlled, 4 5% risk of congenital abnormalities (2* general population). Bleeding from an abnormal fetal vessel attached to the membranes over the internal os. Later in the pregnancy, or in a following pregnancy, IgG can cross the placenta causing Erythroblastosis Fetalis (? Test for anti-D antibodies in all Rhesus ive mothers at booking and in 2 trimester. Hard to diagnose regular uterine contractions are normal, cervical changes in labour can be subtle? Ritgen Manoeuvre upward pressure on chin through perineum from below, downward pressure on occiput (stop anterior tear)? External Rotation/Restitution occiput goes back to original position (transverse) now realigned again with shoulder. Gentle traction on chord with supra-pubic pressure (stops uterus coming down) or fundal massage and maternal bearing down without traction? Can manually deliver (place hand into uterus and separate) if no haemorrhage then wait for anaesthesia? Passage disproportion between the size of the pelvis and the fetus (eg scarred cervix)? C-section if < 1000 gm (body comes through at 7 8 cm dilated and head gets stuck = entrapment of after-coming head) or > 3600 or 4000 gm. Only approx 1% of babies infected but approx 50% mortality if infected Perinatal Asphyxia? Death associated with pregnancy or trophoblastic disease up to 3 months after the event (required to be reported to Medical Officer of Health)? Lochia: red for day 1 3, yellow next 10 days, white until 6 weeks Reproductive and Obstetrics 373? Puerperal Pyrexia = temperature of at least 38 C on any 2 of the first 14 days after abortion or delivery, exclusive of the first 24 hours? Genitals: Check boys for undescended testes (cryptorchidism) 2%, especially if premature, spontaneous descent unlikely beyond 3 months, surgery at 9 12 months. Signs of post-natal depression or adjustment disorder: poor sleep or appetite, feeling low? Complete a screening survey such as the Edinburgh Postnatal Depression Questionnaire. Complete breast feeding provides 98% protection for the first 6 months (provided they continue to have amenorrhoea). If the mother is concerned about the baby being unsettled afterwards, prophylactic oral paracetamol can also be offered. Necrotic fat cells surrounded by an inflammatory infiltrate, with later calcification and scarring. Histology: Chronic inflammation and fibrosis around ducts loaded with lipid and macrophage rich material? Preductal mastitis: periareolar inflammation, abscess formation, unilateral, single duct, etc? Histology: epithelium may be flattened, cuboidal, columnar, piled up or show apocrine metaplasia. Benign proliferation of small ductules in a fibrous stroma, but histologically circumscribed? Apocrine Metaplasia: Benign metaplastic change to tall cells with eosinophilic cytoplasm resembling those of secretory glands (eg lactation, sweat, etc)? Duct (and sometimes lobular) epithelial hyperplasia Generally Benign Breast Tumours Fibroadenoma? Comedocarcinoma: solid intraductal proliferation, central necrosis, microcalcifications on mammogram? Classified by nuclear grade (low, intermediate and high) and the presence or absence of necrosis. Medullary: Big, bulky and soft, plentiful lymphocytes, better prognosis than other types? However, lots of unnecessary interventions, and for a majority (>70%) whose cancer is diagnosed, the outcome is unchanged (but will live with 2 years extra knowledge of condition)? Cervical secretions in women not on the pill, and which change during the cycle, are part of normal discharge. Desquamating vaginal cells with healthy lactobacilli are major part of normal discharge pH < 4. Replacement of lactobacilli with small coccobacilli (Gardnerella) or motile curved rods (Mobilunus). Urethritis, unexplained cystitis, mucopurulent cervicitis, pelvic pain, irregular bleeding? Seborrhoeic dermatitis: a fungus, red, sharply defined area covered with honey coloured scales? Maori admission rates for schizophrenia are similar to pakeha, readmission rates are higher? Maori more likely to be referred to mental health services by welfare or law agencies than by a doctor (opposite for Pakeha)? Therapeutic alliance is with whole family, not just patient th th 410 4 and 5 Year Notes? Community based delivery: psych hospitals were very expensive and only cared for small proportion of people with mental illness? Precipitating Factors: Factors that occur shortly before the onset of the disorders and are likely to have caused it. Physical: hypothyroidism, drugs, drugs of abuse, head injury (either direct disturbance or due to associated stress)? Psychological: eg loss of self-esteem owing to relationship or financial catastrophe? Perpetuating factors: Factors that prolong the course of the disorder: eg secondary demoralisation? Most common psychiatric illnesses in physical illness are mood disorders and acute organic mental disorders? Physical distress can cause psychological ill-health (as can the medicines for physical disease)? Physical and psychological disorders may exist simultaneously and independently (especially in the elderly)? Can cause (eg head, neck, lower back, abdomen, genitalia) or arise from psychological disturbance (eg facial pain antidepressant therapy can be effective). Name, date of interview, age, sex, race, country of birth, occupation, date of hospital admission, marital status? What sort of problems are troubling you/were troubling you when you came to hospital? Ask about visions, sensations, noises that are unusual or not shared by other people? Suicidibility or other dangerous behaviour: See Suicide Assessment and Management, page 416? Changed sleep, energy/motivation, concentration, appetite/weight (look for a 5% change over several weeks), sex? Impulse-Control Screen: Screen for gambling (comorbidity of gambling with other pscyh symptoms is common)? Get idea of family atmosphere during childhood: personalities of parents and relationships have lasting influence on subsequent relationships.
A yellow colour (acid production) indicates a positive reaction and usually occurs mostly within 24?48 h erectile dysfunction treatment fort lauderdale order cheap apcalis sx. An enhanced zone of haemolysis at the intersection of the test strain with each of the cultures is a positive reaction impotence mental block order cheapest apcalis sx and apcalis sx. Expression of results: Presence or absence of Listeria monocytogenes in the test portion are reported in grams or the millilitres of the sample tested erectile dysfunction hypnosis generic apcalis sx 20 mg overnight delivery. Performance criteria erectile dysfunction medication samples cheap apcalis sx 20mg without prescription, quality assurance: To check the quality of the enrichment and identification media on selective growth a dilution of the reference culture of recently isolates strains of Listeria and negative control strains in a control flask of the selective primary enrichment 51 Manual on Laboratory Testing of Fisheries Products December 2016 medium is introduced erectile dysfunction medicine in dubai generic apcalis sx 20mg with mastercard. Add 10-100 Listeria monocytogenes cells or negative control strains per flask and proceed with the control flasks as for the test cultures to demonstrate that the positive control is recovered erectile dysfunction products purchase apcalis sx with a mastercard. The International Standards provides information on the control strains that can be used. Putative Listeria isolates on selective agars from standard or screen positive enrichments are purified on non-selective agars and confirmed by conventional identification tests or by a battery of such tests in kit form. Histamine fish poisoning results from the consumption of inadequately preserved and improperly refrigerated fish. Marine biotoxins in a range of fishery products, originating from phytoplankton d. Sulphite salts that are used as a means of controlling melanosis in raw crustaceans such as shrimp and lobster. For these risks to public health legal maximum limits are set by European Regulations. Batches of fishery products in which the levels of contaminants or residues exceed the maximum limits as indicated, shall be regarded as unfit for human consumption. This section describes the testing methods which must be followed if the results are to be considered valid, and accepted as evidence of compliance. The methods set out also include reference to sampling plans and instructions for sample preparation are specified. Where no specific methods for the determination of contaminants in foodstuffs are prescribed, laboratories may select any validated method of analysis. Heavy metal content should be recorded with information regarding species, size/age of fish, catch location, and season, to allow the operator to build up a picture of the distribution. Sampling plans are also provided as well as the minimum number of incremental samples to be taken from the lot or sub-lot. The weight of an incremental sample should be at least 100 grams or 100 millilitres, resulting in an aggregate sample of at least about 1 kg or 1 litre. Sampling should be performed by an authorised person, and 10 incremental samples per lot should be taken. Any changes that would affect the levels of contaminants, adversely affect the analytical determination, or make the aggregate samples unrepresentative, should be avoided and precautions taken. As far as possible, incremental samples should be taken at various places distributed throughout the lot or sublot. Each sample should be placed in a clean, inert container offering adequate protection from contamination, from loss of analytes by adsorption to the internal wall of the container, and from 54 Manual on Laboratory Testing of Fisheries Products December 2016 damage in transit. All necessary precautions should be taken to avoid any change in composition of the sample which might arise during transportation or storage. A record should be kept of each sampling, identification, date and place of sampling, together with any additional information likely to be of assistance to the analyst. The fish sample taken for analysis should reflect the portion to be consumed, normally the muscle, separated from any skin and bone. Clean water should be used to wash the sample prior to analysis and blending of the sample such that a representative subsample can be taken. The analyst cuts off the contaminated front of the fish samples and takes 100 g of each incremental sample. A final rinse with de-ionised water is recommended, rinsing water being removed from the samples (soft tissue etc. The fish is cut with a ceramic knife, and care is taken during cutting not to damage the abdominal wall, to avoid contamination of the muscles with the guts. Skin and bones are discarded and only the muscles without skin and bones are homogenised. Fish fillets are used in their entirety, while fish species normally intended for eating with bones and skin. For canned fish, separate fish and other parts of the product if possible, and homogenise the content of the can. The aggregated sample is made up by uniting all incremental samples and should be at least 1 kg, finely ground (where relevant), and thoroughly mixed, using a process that has been demonstrated to achieve complete homogenisation. The analyst should ensure that samples do not become contaminated during sample preparation. Wherever possible, apparatus and equipment coming into contact with the sample should not contain the metals to be determined, and be made of inert materials. For operations, such as cutting and weighing, special equipment such as ceramic knives, porcelain or quartz spatula, agate grinders, should be used. Principle: the sample is oxidized by wet ashing in a microwave digester, using hydrogen peroxide and nitric acid. Lead and cadmium are determined by graphite absorption spectrometry, following dilution of the sample extract. General considerations and specific requirements 56 Manual on Laboratory Testing of Fisheries Products December 2016 the manufacturer for the particular system in use (generally between 20 min and 30 min). After cooling, the sample is measured and made up to volume (minimum 25 ml) with distilled water. Metal content is calculated from a calibration curve, using a minimum of three calibration standards, of which at least two should be addition standards (a standard in the presence of sample matrix at the same concentration as in the test sample). The criteria for performing the method follow standard provisions, using a validated procedure for which performance data are available from published reports of inter-laboratory testing. The veracity of the procedure is confirmed by testing a certified reference material. The specificity is confirmed by the absence of interfering materials, when testing samples and reagents without residues are present. Performance criteria for methods of analysis for lead and cadmium are provided for applicability, limit of detection, limit of quantification, precision, recovery and specificity. Scope: the method is specifically for the determination of residues of mercury in foodstuffs. Digestion time may be up to 3 h, but this is significantly reduced in a microwave system (maximum normally 30 min). With pressure digestion, common conditions are for the sample to be heated to 150?C over a period of 60 min, then the temperature raised to 300?C in 40 min, and kept at 300?C for a further 60 min. In a microwave system, digestion is started at low power, and the power then raised in stages, with 5-min holding periods, to 1000 W and held for a further 10 min. For operating procedures, consult the manual for the specific hydride generator in use. Pressure digestion 58 Manual on Laboratory Testing of Fisheries Products December 2016 As an analytical quality control reference samples having reliable known mercury contents should be analysed in parallel with testing samples at all steps in the method. Calculate the mass fraction of mercury, w, in milligrams per kilogram of sample by using the equation: w= a x V V1 x m x 1000 Where a is the absolute mass of mercury, in nanograms found in the test solution used; V I the volume of the digestion solution after being made up in millilitres; V1 is the volume of test solution used in millilitres, and m is the initial sample mass in grams. If necessary, subtract the result of the blank solution from the content of mercury. The criteria for performing the method follow standard provisions using a validated procedure where performance data are available from published reports of inter-laboratory testing. Precision, repeatability and reproducibility of the method should be established and confirmed by an interlaboratory comparison, with results provided by the standard. Performance criteria for methods of analysis for lead, cadmium, mercury are provided for calculation of applicability, limit of detection, limit of quantification, precision, recovery and specificity. Laboratories should participate in appropriate proficiency testing schemes, and apply quality control, such as quality control charts. Journal of the Association of Official Analytical Chemists International 79(1): 43?49 and Duflos G. Relevance of matrix effect in determination of biogenic amines in plaice (Pleuronectes platessa) and whiting (Merlangus merlangus). The normal sampling plan for histamine from fishery products consists of nine samples to be taken, in which the average histamine content must be 100mg/kg or less. No more than 2 samples may have levels between 100mg and 200mg/kg, and no sample may have a level above 200mg/kg. These limits apply to fish from the following families only: Scombridae: tuna, mackerel, bonito, etc. A consignment of fishery products comprising a fish species susceptible to the production of histamine, should not be placed on the market if the level of histamine in nine samples selected at random from the consignment, exceeds the minimum levels specified below. Fish from these families, which have undergone enzyme-ripening treatment in brine, are permitted higher histamine levels, but not more than twice the above values. Maximum level of histamine in fish sauce produced by fermentation of fishery products is established at 400 mg/kg, and a new single sample sampling plan should be applied for histamine in fish sauce placed on the market during its shelf-life. If the single samples are found to contain more than 400 mg/kg the whole batch should be deemed unsafe. For preparation of the test sample, 200g should be available from the eatable part of the laboratory sample. A final rinse with de-ionised water is recommended, and rinsing water removed from the samples (soft tissue etc. Care should be taken during cutting so as not to damage the abdominal wall to avoid contamination of the muscles with the guts. For canned fish, separate fish and other parts of the product if possible, and homogenise the contents of the can. Add 10 ml perchloric acid previously cooled to 2?C, then add 100 l of 1,3-diaminopropane solution and blend for 1 minute. Swirl and place the tube in the 60 Manual on Laboratory Testing of Fisheries Products December 2016 dark for 15 min. Add 500 l toluene, swirl again and keep in the freezer at -18?C for at least 30 min. Collect all the non-frozen, organic substance in a new tube, and evaporate the solvent under nitrogen flow at room temperature. Standard derivatization: Add 1 ml of each of the dilute working standards to separate, labelled 5 ml volumetric flasks, and then proceed as above, without the addition of the 1 ml of sample extract. The procedure is suitable for the determination of histamine in fresh, frozen, canned, and smoked fish. Histamine is separated on a reversed phase C18 column using a water/acetonitrile gradient. Calibration curve: A five-point calibration curve is constructed, plotting histamine content (x axis) against response (y axis). Validation samples: Treat replicate samples of homogenized fish tissue with (i) 0. It is recommended to use validated tests and to verify them for the use at the laboratory in official controls. In the Guide to Food Safety Hazards in Caribbean Fishery Products, a selection of some of the commercial testing systems available for rapid testing of histamine in fishery products is provided. Reference: Foodstuffs Determination of Sulfite Part 1: Optimized Monier-Williams Method. Scope: the procedure allows for the determination of sulphite as sulphur dioxide in a wide range of foodstuffs at concentrations greater than 10 mg/kg. Principle: Sulphite residues are converted to sulphur dioxide by refluxing with hydrochloric acid. The sulphur dioxide is distilled, in a flow of nitrogen, and trapped in hydrogen peroxide solution. The sulphuric acid thus produced is determined by titration with sodium hydroxide solution. Equipment: a) Distillation apparatus for optimized Monier-Williams method (commercially available) b) Burette, 10 ml capacity, designed to maintain carbon dioxide free atmosphere over the contents (sodium hydroxide) c) Chilled water circulator d) Heating mantle, 1 litre capacity e) Gas regulator for nitrogen supply, with oxygen absorbing trap Reagents: a) Hydrochloric acid, 4 mol/litre b) Hydrogen peroxide solution c) Sodium hydroxide solution, 0. Sample Preparation: Homogenize 50g of sample with 100 ml of the ethanol/water mixture, until the sample is reduced sufficiently to pass through the neck of a round-bottomed flask. Method: Assemble the apparatus (see Figure 1), add 400 ml of water to the round-bottomed flask through the dropping funnel, and close the funnel tap. Apply nitrogen to the system at a rate of 200 ml/s and allow the system to purge for 15 min. Open the tap of the dropping funnel to allow the acid to enter the distillation flask, using pressure (if necessary), applied through the adapter attached to the funnel. Do not drain the acid entirely as this acts as a liquid barrier to prevent the escape of any liberated sulphur dioxide. Ensure that the coolant is flowing through the condenser, then apply heat to the distillation flask and boil the contents at a steady rate for 105?110 min. Disconnect the receiver flask/tube, and immediately titrate with the standardized sodium hydroxide solution, using the methyl red indicator until an endpoint is reached where the yellow colour lasts for longer than 20 s. Expression of results: Calculation: the concentration of sulphur dioxide, in mg/kg, is calculated using: mg/kg = 32. Quality assurance: Prepare a reagent blank and run the test again, titrating the distillate and correcting the sample test result as appropriate. There are no validated rapid methods suitable for dockside, nor commercial testing of lots of fish for any of these toxins. The sites and collection frequency may change depending upon the prevalence of algal toxins but any changes must be notified beforehand.