Thierry H. Le Jemtel, MD
- Henderson Chair Professor of Medicine
- Director, Heart Failure and Transplant Program
- Tulane University Heart and Vascular Institute
- New Orleans, Louisiana
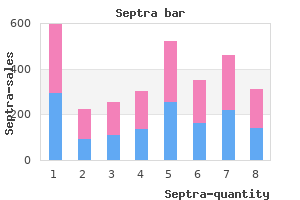
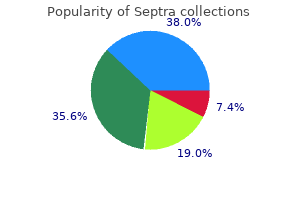
We good-quality patient-oriented evidence on this suggest the use of a simple figure (Fig shinee symptoms mp3 generic septra 480mg with amex. It remains to be seen showing the expected severity and duration of whether certain foods (especially saturated fats acne medicine used for uti discount 480mg septra amex. Also symptoms 0f pregnancy septra 480mg visa, neuroactive substances Exposure to sunlight has a beneficial effect on within the epidermis withdrawal symptoms buy discount septra on-line, such as substance P medications during breastfeeding buy 480mg septra with mastercard, have acne in the majority of cases medications 44 175 buy septra with amex, especially when been incriminated to upregulate lipid synthesis in acne is localized on the back and chest, but dete sebaceous cells and to stimulate the proliferation rioration may be noted in 20 % of patients. Before starting any therapy for acne, it is neces Stress has traditionally been the main culprit sary to advise the patient to apply topical thera in aggravating acne according to our patients. A significant association between acne In order to minimize irritation associated with severity and increased stress levels during exami the use of topical retinoids, short durations of nation periods has been reported in a prospective application should be adopted at first, with grad study of 22 patients, even after controlling for ual increments in application time as tolerated changes in diet and sleep habits. Also, patients should be advised to use a authors pointed out that the association observed gentle cleanser and a moisturizer [1 ]. Sometimes an aggravation treatment should be explained to patients or par may be experienced during the first few weeks of ents of minors. Some patients are reassured to therapy, but in most patients acne will improve by learn that isotretinoin is a naturally occurring 60 % in 4 months and by at least 80 % in 6 months endogenous compound [1, 18]. The frequent appli to 1 year for hormonal treatments, and up to 6 cation of moisturizers is usually sufficient and months for oral antibiotics [2]. They are also suggested in order to counteract the drying effect of topical retinoids, benzoyl peroxide, azelaic acid, and oral 53. Noncomedogenic and nonacnegenic cosmetics and makeup should be recommended the desire for acne treatments associated with a for acne patients [2, 17]. An explanation of the most frequent side effects New and emerging systemic antibiotics include to expect with a proposed acne treatment should lymecycline, azithromycin, anti-infiammatory be provided to the patient, together with simple dose doxycycline, and a new extended-release advice on how to handle them. A lower starting dose of isotretinoin has bacterial resistance (anti-infiammatory dose doxy been recommended in order to avoid this adverse cycline) [7]. Efficacy relies on good dosing compliance and good compliance results from convenience in use Conclusions and treatment tolerability [1, 5]. Since acne is a chronic disease, it may Once-daily use of a micronized and more bio necessitate treatment for months or years. This new formulation can be taken with dermatologists is central in considering food at a single daily dose of 0. When the relationship between doctor and patient has been built on trust and confidence, 53. The development of side effects during treatment and hence diminished patient tolerability can References lead to decreased compliance. Patient compliance: enhancing clini patients treated with low-dose isotretinoin com cian abilities and strategies. Patient concepts and mis months of isotretinoin treatment (at a dose of conceptions about acne. Changes in acne vul on severity, it may require the administration of garis as affected by examination stress. Analysis of common side effects of isotret immuno-cutaneous-endocrine network: relationship inoin. Low-dose normal to oily skin on the skin barrier of subjects with isotretinoin in the treatment of acne vulgaris. Maibach Topical keratolytic agents have long been Department of Dermatology, University of California, employed for acne treatment. In this manner, these obstruct the infundibulum and the sebaceous duct, agents modulate and correct abnormal follicu paving the way for excessive sebum secretion, lar keratinization. Available in varying concentra Under light microscopy, microcomedones tions and vehicles, they may be specifically are visualized as layers of horny cells surround indicated depending on the type, duration, and ing a sebum and bacteria core [1]. The proceeding text covers agents are thought to function by relaxing the widely available topical and oral keratolytics, cohesiveness of the stratum corneum layer, controlled trials comparing keratolytic agents, which serves as a crucial, life-sustaining bar and in vivo keratolytic protein assays. Acting through oxidation and formation alone; the combination took longer to dry and of free radicals, its bacteriostatic activity is supe was stickier according to subjects [12 ]. Three well proteins; this may predispose to skin dryness and designed, randomized, double-blind, vehicle desquamation [5]. In two of the trials, accumulate in the lipid-rich pilosebaceous units global improvement assessments demonstrated and subcutaneous fat [4]. Furthermore, the side-effect pro tial fetal harm or breast milk excretion, and posi file (dry skin, peeling, and erythema) of tive in the rodent photocarcinogenicity assay. It may ules/pustules and fiushing/blushing after just a also inactivate tretinoin if both are applied con few weeks [15]. Retinoids may Topical retinoids encompass a group of powerful, exert an anti-infiammatory response by inhibit comedolytic, anti-comedogenic, and anti ing the release of proinfiammatory cytokines infiammatory agents. They are powerful kerato (interleukins 12 and 8 and tumor necrosis factor) lytics, targeting both primary and secondary via downregulation of monocyte Toll-like recep prevention of comedones [6]. Both receptor families are ferent pathophysiologic factors in acne vulgaris ligand-dependent transcription factors and con [19]. This combination approach is optimal in sist of three receptor subtypes (fi, fi, and fi), patients with both infiammatory and comedonal encoded by three separate genes [21]. Retinoids also inhibit expres permeability, enhancing penetration of antimi sion of certain genes by downregulating other tran crobial agents. Between-retinoid comparisons are thought to affect cellular differentiation and demonstrated tazarotene to have the greatest effi proliferation [20]. Experimental studies, some cacy on the overall infiammatory acne severity using primary neonatal mouse epidermal kerati and global response scales [25 ] (Table 54. Malformations include targeting folliculo-infundibular delivery in the microtia/anotia, conotruncal heart defects and process [34]. Some clinical trials have demon aortic-arch abnormalities, thymic defects, and strated reduced irritation as less drug penetrates central nervous system malformations [28]. Several case reports suggest these effects may the Microsponge Delivery System found in not be limited to oral retinoid therapy, with limb 0. It is an effective comedolytic agent, which events; there were no significant differences in increases epithelial cell turnover and modulates tolerability between the treatment and control abnormal keratinization (that leads to microcom groups at week 12 [24]. These results were confirmed by cream significantly reduced infiammatory and two large studies; adverse effects were similar in non-infiammatory acne lesions compared with frequency and severity to tretinoin alone [36 ]. A large study In a split-face ultrastructural study comparing demonstrated earlier favorable global assessments 0. Maibach plugs infested with bacteria were transformed systemic antibiotics [19] (see relevant Chap. Using transmission electron microscopy, ratinization to include actions on the sebaceous it was possible to track microcomedones with gland (decreases size and secretion), anti-comedo compact, adherent stratum corneum morphing genic properties, and reduction of P. Tazarotene, a topical acetylenic retinoid indicated Surprisingly, topical tretinoin has poor percu in both psoriasis and acne vulgaris, is hydrolyzed taneous absorption and does not alter systemic by keratinocyte esterases to tazarotenic acid, its retinoid levels, which stay constant despite appli active metabolite [19]. Additionally, izes the keratinization pattern and decreases coher tretinoin may bring out the postinfiammatory ence of follicular keratinocytes, manifesting both darkening which occurs in healing acne of darker comedolytic and anti-comedogenic properties skinned patients [27]. Tazarotene also has anti-infiammatory prop tation may be explained by a fiexible chemical erties [20]. In the systemic circulation, tazarotenic structure, resulting in nonselective action and the acid is rapidly converted to inactive sulfur-oxi ability to activate numerous pathways, resulting dized forms, resulting in limited exposure [40]. Applying a A randomized, double-blind, vehicle moisturizing cream along with topical tretinoin or controlled study demonstrated that 0. They can be reduced by spac strated a significant decrease in infiammatory ing out applications and/or diminishing fre acne at 12 weeks [20]. Despite some evi ing comedone count and producing global dence to the contrary, topical tretinoin is not improvement, with no significant difference in advised during pregnancy and lactation. Although only non for systemic exposure and excretion in breast infiammatory lesions could be compared in this milk has not been adequately studied. It also inhibits production of leukotri more effective than daily tazarotene monother enes by 5 and 15-lipoxygenase pathways [21, apy in reducing comedo count and infiammatory 22]. Furthermore, adapalene may have a dose lesion count (in those with fi25 baseline infiam dependent response, with 0. Additionally, regard to scaling, erythema, dryness, immediate after 12 weeks of normal tazarotene application, and persistent burning, and immediate pruritus serum samples from 22 subjects demonstrated [45]. With its three aromatic rings, adapalene limited systemic exposure with most below the demonstrates higher stability than tretinoin in the quantifiable limit (<0. In a study Local side effects typically occur; these include comparing the chemical stability of 0. In the Bershad study approximately 100 % of adapalene remained cited above, half of patients applying tazarotene intact versus only 20 % of tretinoin [46]. Favorable tolerabil retinoids in acne treatment, it is the only one ity to adapalene may be explained by its receptor requiring sufficient contraception in women of specificity, neutral molecular structure, and lack childbearing age [22 ]. These microscopic and experimental find dryness, pruritus, and burning, occur mainly dur ings indicate keratolytic and anti-comedogenic ing the first month and decrease thereafter [10]. Cyanoacrylate strip in non infiammatory acne lesions after topical data suggest that application of adapalene 0. This anti-infiammatory activity may poten equivalent comedone and total lesion reduction and tially be mediated through inhibition of hydroxyl similar overall improvement [56]. However, treti and superoxide radical production by neutrophils noin use led to increased erythema, scaling, and [51]. Contributing to its anti-infiammatory prop irritation-induced discontinuation than did azelaic erties, in vitro, azelaic acid is an oxygen-free acid [56]. Another trial comparing 20 % azelaic radical scavenger, inhibiting hydroxylation of acid with 5. To date no published reports of response and infiammatory lesion reduction by 4 azelaic acid bacterial resistance have surfaced. Pooling together results of four tri of human keratinocytes by decreasing synthesis als, Mackrides et al. This results in alterations of epidermal kera fi50% decrease in number of lesions (good-to tinization, including reductions in the number excellent clinical response) (Table 54. Isotretinoin for first 10 Moderate and None Acne scores were significantly lower (2007) days of each month for 6 severe for all groups posttreatment. Leyden 10-week trial comparing Moderate to None All treatments had significantly reduced et al. Katsambas 6-month trial comparing Comedonal but None Similar decreases in comedone and et al. Open-labeled, prospective Non-infiammatory None All three treatments were effective in (2005) study comparing 0. Symptomatic improvement is epidermis and dermis, and 4 % is absorbed sys typically observed within 4 weeks of commenc temically (although this can double with gel for ing therapy [6 ]. These include burn are primarily dependent on dietary intake of ing, erythema, dryness, scaling, pruritus, and whole grain cereals and animal products [6]. Authors Drug Result Despite efficacy as a monotherapy, a large Bashir Aqueous Statistically significant et al. In one study, 60 % of patients using 2 % and 10 %), 2 % is the maximum strength allowed by 0. In both studies side tion was induced via 10 % coal tar distillate oint effects were minimal and well tolerated [60]. In a ment at four sites on the back; formation was study comparing medicated pads with 0. Reductions of open comedones biopsied and examined microscopically; all three and total lesions were also significant compared concentrations displayed tremendous comedo to placebo [61 ]. In the acne arena, sulfur is thought cin combination with placebo demonstrated a to be keratolytic and bacteriostatic. Salicylic acid is well absorbed as evidenced by Appearing in a variety of vehicles (lotions, numerous studies; its bioavailability in topical creams, soaps, ointments), it appears to be more application varies according to duration of contact efficacious when used in combination with other [8, 64]. The same study also demon have resulted in reduction of infiammatory lesions, strated the hydroalcoholic vehicle to have superior comedones, and seborrhea [68 ]. In clinical trials, sulfur significantly in a mineral oil/petrolatum ointment and sulfur/sodium sulfacetamide have demon compared to an ointment containing polyethyl strated superiority in reducing overall severity ene glycol, glycerol, petrolatum, and 10 % urea and infiammatory lesion count when compared to (Kerasal) [66]. Polyethylene glycol may be a more tolerable Additionally, there is no evidence of systemic vehicle than the commonly used ethyl alcohol in absorption in intact skin [68]. Later stud of the body for prolonged periods of time, salicy ies did not confirm these results despite identical late toxicity, toxic inner ear damage, and hyper treatment conditions [68, 71]. To that effects include dryness, itching, and malodorous end, these manifestations are uncommon in skin. In the context of acne, dermatological indications, including but not research has been conducted examining glycolic limited to acne vulgaris, rosacea, seborrheic acid chemical peels. Between peels, low concentrations of gly lesion reduction and equivalent non-infiammatory colic acid may be used as a daily cleanser to pre lesion reduction, while causing less dryness, vent re-occlusion of follicles [73 ]. Glycolic acid, a hydrophilic compound with keratolytic properties, is present in many peel formulations due to its desquamating efficacy.
Bowel Injury Because patients with suspected pelvic adhesions or obvious pelvic disease are excluded as candidates for vaginal hysterectomy medications given to newborns order septra 480mg fast delivery, bowel injuries do not occur often georges marvellous medicine buy cheap septra line. Bowel injuries are associated with the performance of a posterior colporrhaphy and are usually confined to the rectum medicine 2020 buy generic septra pills. If the rectum is entered symptoms 2016 flu purchase septra 480 mg on-line, the injury is repaired with a single or double-layer closure using a small-caliber absorbable suture medicine 5658 buy septra on line amex, followed by copious irrigation 92507 treatment code discount septra 480mg amex. Postoperatively, the patient should be given a stool softener and a low-residue diet. Hemorrhage Intraoperative hemorrhage invariably is the result of failure to ligate securely a significant blood vessel, bleeding from the vaginal cuff, slippage of a previously placed ligature, or avulsion of tissue before clamping. Most intraoperative bleeding can be avoided with adequate exposure and good surgical technique. Using square knots with attention to proper knot-tying mechanisms will prevent bleeding in most cases. The use of Heaney-type sutures may minimize ligature slippage and subsequent bleeding from bulky pedicles. When bleeding does occur, blind clamping, which may endanger the ureter, should be avoided. The bleeding vessel should be identified and precisely ligated, with visualization of the ureter if necessary. If the location of the ureter is in question, it should be visualized before suturing a bleeding vessel. Perioperative Care Bladder Drainage Postoperative bladder drainage should be employed after any procedure in which spontaneous, complete voiding is not anticipated. Reasons to consider closed bladder drainage include significant local pain, additional vaginal reparative procedures, surgery for stress incontinence, the use of a vaginal pack, and patient anxiety. After vaginal hysterectomy without additional repair, most patients can void spontaneously, and catheter drainage is not required. The relative amount of pain after a vaginal hysterectomy is less than with abdominal hysterectomy and, in the absence of additional repairs or a pack, no obstructive effect should be present. If the patient does not tolerate pain well postoperatively or is extremely anxious, the transurethral insertion of a 16-Fr. This catheter may be inserted postoperatively if the patient is unable to void spontaneously on two attempts. Closed-catheter drainage after vaginal hysterectomy usually is not necessary for longer than 24 hours. The catheter is removed without clamping, and there is no need to obtain a urine specimen for culture and sensitivity. Diet Although little manipulation of the bowel occurs during vaginal hysterectomy, there is some slowing of gastrointestinal motility. This slowing rarely occurs to a degree that limits some form of oral intake soon after surgery. Most patients experience some degree of nausea after surgery, which, combined with drowsiness from analgesics, usually makes them disinterested in food on the evening after surgery. A clear liquid diet is suitable during the first night after surgery, and on the first full postoperative day, a regular diet can usually be consumed. The patient is often the best judge of what she can tolerate as her appetite returns. Laparoscopic Hysterectomy Preoperative Preparation the main limitations to a laparoscopic approach are medical or anesthetic disorders that do not allow adequate pneuomperitoneum or proper ventilation (34). Extensive and dense pelvic abdominal adhesions from previous surgery and very large uterine size are relative contraindications, although this decision can be made after assessing the peritoneal cavity (see Chapter 23). If the uterine size limits access to the uterine vessels, laparoscopic hysterectomy may not be possible. Different classifications were proposed for the types of laparoscopic hysterectomy. The Cochrane review authors recommended that if the vessels are occluded laparoscopically, or if part of the operation is performed vaginally, the procedure be called laparoscopic hysterectomy, and, if no component is performed vaginally, the procedure should be called a total laparoscopic hysterectomy (41). Hyperflexion of the hips should be avoided because this may cause femoral nerve palsy. The patient should be placed on an egg crate mattress or beanbag cushion to limit patient movement in the Trendelenburg position. Shoulder braces should not be used as they are associated with brachial plexus injury. Instrumentation the most important instrument is the one used to occlude blood vessels. A multitude of energy forms exist, including electrosurgery, lasers, and ultrasonic scalpel (see Chapter 23). Some surgeons use stapling devices, although the cost of these stapling devices is high, and an energy-occluding device is needed to access areas that a stapler cannot. The versatility of the devices with energy makes them the method of choice to occlude vessels. There are no valid clinical data showing that one instrument is safer than another. The preferred one involves bipolar energy because gynecologists are experienced with this form of energy. Surgical Technique of Laparoscopic Hysterectomy Peritoneal Access the most important technical consideration for all laparoscopic surgery is port placement (se e Chapter 23). The umbilical site typically is used in patients without a previous history of surgery or intra-abdominal infection. In cases of previous surgery where there was a midline incision or a history of a pelvic-abdominal incision, an open laparoscopy is done or an alternative site is chosen to introduce the primary cannula. The standard closed technique involves the use of pneumoperitoneum needle (Verres needle), insufflation, and primary trocar insertion. An alternative technique is the direct trocar insertion (no insufflation prior to trocar insertion). If the left upper quadrant is used, the surgeon should be aware of the closest anatomic structures to the left costal margin (see Chapter 23, Fig. Typically the cannula is introduced below the left costal margin in the midclavicular line. The closest structures to this area are the stomach and the left lobe of the liver. Therefore, an oral gastric tube should be introduced to empty the stomach before starting the procedure. The patient is kept in a horizontal (not Trendelenburg) position until proper peritoneal access is confirmed. The angle of insertion of the primary trocar will depend on the size of the patient. Typically for nonobese or overweight patients a 45-degree angle from the horizontal is used and with obese patients a 60 to 80-degree angle or open technique is used. Proper placement of accessory ports is critical to allow the steps of a laparoscopic hysterectomy. The authors typically use three lateral accessory ports and do not use a suprapubic port. Lateral ports offer the surgeon an ergonomic approach in which both hands can be used comfortably. The most important step when placing lateral ports is to avoid the inferior epigastric vessels, which are branches of the external iliac artery and vein. These vessels (typically two veins and an artery) are seen through the peritoneum medial to the insertion of the round ligament in the deep inguinal ring. Ports are placed approximately 8 cm from the midline and 8 cm above the pubic symphysis. Laparoscopic hysterectomy requires traction and countertraction to identify the vascular pedicles and the ureter, which is accomplished with the uterine manipulator. The incision is carried anteriorly to create a bladder peritoneal flap by sharp dissection of the loose areolar cervicovesical tissue. The retroperitoneal space is opened and the ureter identified on the medial leaf of the broad ligament (Fig. The ovarian vessels (infundibulopelvic ligament) or the utero-ovarian ligaments are coagulated and transected, depending on whether the ovaries will be removed (Fig. The uterine artery is skeletonized by cutting the posterior peritoneum up to the uterosacral ligament, coagulated, and transected. The anterior dissection should be completed so that the bladder is completely off the anterior fornix area of the vagina (Fig. The uterus can be pulled out though the vagina or can be morcellated first, and then removed either vaginally or laparoscopically, whichever is easier. Intravenous indigo carmine is given and the integrity of the bladder and ureters confirmed with cystoscopy, if desired, by the surgeon. At the end of the procedure, the secondary ports should be removed under direct visualization to ensure that there is no bleeding. The fascia should be closed at port sites that are 8 mm or greater and smaller ports that have prolonged manipulation to avoid possible herniation. The patient is kept in the short stay unit and discharged within 24 hours if there are no complications. Side docking allows access to the perineum and vagina so that the assistant can comfortably manipulate the uterus. A robot-assisted hysterectomy goes through the same steps as a laparoscopic hysterectomy. A right-handed surgeon should have the monopolar scissors or harmonic scalpel through a right robotic port and a vessel-sealing device such as a bipolar instrument through a left-sided robotic port. If a fourth robotic arm is used, the additional port is placed on the right side for right-handed surgeons. Observational studies showed that outcomes for robotic-assisted hysterectomy can be similar to laparoscopic hysterectomy but with less blood loss and possibly fewer conversions to laparotomy (55,56). The learning curve to stabilize operative times for skilled laparoscopic surgeons is about 50 cases (57). Although these case series demonstrated equivalent operative times, an analysis of the Premier hospital database of over 36,000 laparoscopic or robotic hysterectomies demonstrated longer surgical times and higher costs with the robot-assisted procedures compared with conventional laparoscopy with little difference in perioperative and postoperative outcomes (58). Robotic-assisted laparoscopic hysterectomy is associated with delayed vaginal cuff dehiscence around 7 to 8 weeks after hysterectomy, although one case series showed an increased frequency with conventional laparoscopy (59,60). Laparoendoscopic Single-Site Surgery Another modification of laparoscopic hysterectomy is the introduction of laparoendoscopic single-site surgery or single-port surgery. Because some surgeons use one of the multiple ports at one site, laparoendoscopic single-site surgery is probably the best term. The role of single-site access to hysterectomy is unclear, and there are only case reports (61). Specifically designed umbilical port systems that admit multiple instrument access have enabled the development of this technique. The availability of flexible instruments and flexible tip laparoscopes allows the surgeon to perform a hysterectomy by reducing instrument crowding and clashing at the umbilicus. Intraoperative Complications: Laparoscopic Hysterectomy the intraoperative complications of a laparoscopic hysterectomy are similar to an open hysterectomy. Because there is an increased frequency of injury to the ureter and bladder, a cystoscopic evaluation after injection of intravenous indigo carmine dye is recommended (62). Intraoperative bleeding during a laparoscopic procedure is handled by use of a bipolar instrument. If it is not apparent where the bleeding is occurring, the procedure should be converted to an open one. Perioperative Care Many surgeons remove the bladder catheter at the end of the laparoscopic hysterectomy. Postoperative Complications of Hysterectomy A comprehensive discussion of postoperative complications after gynecologic surgery is presented in Chapter 22. Wound Infections Wound infections occur after 4% to 6% of abdominal hysterectomies (33). Measures believed to reduce the incidence of wound infections include a preoperative shower, no removal of hair, or if hair removal is necessary, removal of hair with clippers in the operating room, use of adhesive drapes and prophylactic antibiotics, and delayed primary closure (see Chapter 22). Incisional Pain Incisional pain can occur at trocar sites, especially if located in the region of the ilioinguinal or iliohypogastric nerves. Pfannenstiel incisions can be a source of chronic pain at the incision site as a result of nerve entrapment (63). Hemorrhage Immediately after hysterectomy, hemorrhage may become apparent in one of two ways. Bleeding from the vagina may first be noted by the nursing staff or physician within the first few hours after surgery. Second, the patient may be noted to have little bleeding from the vagina but deteriorating vital signs manifested by low blood pressure and rapid pulse, falling hematocrit level, and flank or abdominal pain.
Buy generic septra on-line. Causes Symptoms and Treatment of Pneumonia.
Testosterone given alone can suppress sperm production to very low levels while maintaining normal libido and sexual performance medications versed purchase septra 480mg overnight delivery. Over many years investigators have studied long-acting testosterone salts for male contraception (276) treatment in statistics discount 480 mg septra with visa. Ethnicity is an important predictor of efficacy of sperm suppression with testosterone therapy treatment xeroderma pigmentosum generic 480mg septra overnight delivery. In Caucasian populations testosterone was combined with progestins to further suppress gonadotropin and improve efficacy medicine 319 pill cheap septra online mastercard. Side effects that were more common in the medicated group than placebo included acne treatment pneumonia order 480 mg septra fast delivery, night sweats symptoms 5dpiui generic septra 480mg with mastercard, libido changes (usually increased), and weight gain. Theoretical risks include atherogenesis and prostate cancer but long-term trials will be needed to determine if risk is real. Sterilization Surgical sterilization is the most common method of fertility control used by couples, with more than 180 million couples having tubal sterilization or vasectomy (4,281) Laparoscopic and hysteroscopic techniques for women and vasectomy for men are safe and readily available throughout the United States. Age younger than 30 years when sterilized, conflict within the marriage, and divorce and remarriage are predictors of sterilization regret, which may lead to a request for reversal of sterilization (281). Female Sterilization Hysterectomy is no longer considered for sterilization because morbidity and mortality are too high in comparison with tubal sterilization. Vaginal tubal sterilization, which was associated with occasional pelvic abscess, is rarely performed in the United States. Tubal sterilization at the time of laparotomy for a cesarean delivery or other abdominal operation Postpartum minilaparotomy soon after vaginal delivery Interval minilaparotomy Laparoscopy Hysteroscopy Postpartum tubal sterilization at the time of cesarean delivery adds no risk other than a slight prolongation of operating time; cesarean birth poses more risk than vaginal birth, and planned sterilization should not influence the decision to perform a cesarean delivery. The uterus is enlarged, and the fallopian tubes lie in the midabdomen, easily accessible through a small, 3 to 4-cm subumbilical incision. Interval minilaparotomy, first described by Uchida, was rediscovered and popularized in the early 1970s in response to an increased demand for sterilization procedures and a simpler alternative to laparoscopy (282). Still widely practiced in lower resource settings, it is uncommon in the United States because of widespread availability of the endoscopic techniques. Surgical Technique the procedure usually elected for tubal sterilization by laparotomy is the Pomeroy or modified Pomeroy technique (Fig. In the classic Pomeroy procedure, a loop of tube is excised after ligating the base of the loop with a single absorbable suture. A modification of the procedure is excision of the midportion of the tube after ligation of the segment with two separate absorbable sutures. This modified procedure has several names: partial salpingectomy, Parkland Hospital technique, separate sutures technique, and modified Pomeroy. In the Madlener technique, now abandoned because of too many failures, a loop of tube is crushed by cross-clamping its base, ligated with permanent suture, and then excised. Pomeroy and partial salpingectomy procedures have failure rates of 1 to 4 per 1,000 cases (281). In contrast, pregnancy is almost unheard of after tubal sterilization by the Irving or Uchida methods. In the Irving method, the midportion of the tube is excised, and the proximal stump of each tube is turned back and led into a small stab wound in the wall of the uterus and sutured in place, creating a blind loop. With the Uchida method, a saline-epinephrine solution (1:1,000) is injected beneath the mucosa of the midportion of the tube, separating the mucosa from the underlying tube. The mucosa is incised along the antimesenteric border of the tube, and a tubal segment is excised under traction so that the ligated proximal stump will retract beneath the mucosa when released. The mucosa is then closed with sutures, burying the proximal stump and separating it from the distal stump. Laparoscopy Laparoscopy is the most common method of interval sterilization in the United States. In the standard laparoscopy technique, the abdomen is inflated with a gas (carbon dioxide) through a special needle inserted at the lower margin of the umbilicus (281). A hollow sheath containing a pointed trocar is then pushed through the abdominal wall at the same location, the trocar is removed, and the laparoscope is inserted into the abdominal cavity through the sheath to visualize the pelvic organs. A second, smaller trocar is inserted in the suprapubic region to allow the insertion of special grasping forceps. Alternatively, an operating laparoscope that has a channel for the instruments can be used; thus, the procedure can be performed through a single small incision. Laparoscopic sterilization is usually performed in the hospital under general anesthesia but can be performed under local anesthesia with conscious sedation. Open Laparoscopy Standard laparoscopy carries with it a small but definite risk for injury to major blood vessels with insertion of the sharp trocar. With the alternative technique of open laparoscopy, neither needle nor sharp trocar is used; instead, the peritoneal cavity is opened directly through an incision at the lower edge of the umbilicus. A special funnel shaped sleeve, the Hassan cannula, is inserted, and the laparoscope is introduced through it. Techniques for Tubal Closure at Laparoscopy Sterilization is accomplished by any of four techniques: bipolar electrical coagulation, application of a small Silastic rubber band (Falope ring), the plastic and metal Hulka clip, or the Filshie clip. The Filshie clip, first introduced into the United States in 1996 is used extensively in the United Kingdom and Canada (283). Because of its lower pregnancy rate, the Filshie clip has largely supplanted the Hulka clip (284). In the bipolar electrocoagulation technique, the midisthmic portion of the tube and adjacent mesosalpinx are grasped with special bipolar forceps, and radiofrequency electric current is applied to three adjacent areas, coagulating 3 cm of tube (Fig. The radiofrequency generator must deliver at least 25 watts into a 100-ohm resistance at the probe tips to ensure coagulation of the complete thickness of the fallopian tube and not just the outer layer; otherwise, the sterilization will fail (285). A loop of tube is pulled back into the probe, and the outer cylinder is advanced (Fig. If the tube cannot be pulled easily into the applicator, the operator should stop and change to electrical coagulation rather than persist and risk lacerating the tube with the Falope ring applicator. The banded tube must be inspected at close range through the laparoscope to demonstrate that the full thickness of the tube was pulled through the Falope ring. The Hulka clip is placed across the midisthmus, ensuring that the applicator is at right angles to the tube and that the tube is completely contained within the clip before the clip is closed. The Filshie clip is placed at right angles across the midisthmus, taking care that the anvil of the posterior jaw can be visualized through the mesosalpinx beyond the tube to ensure that the complete thickness of the tube is completely within the jaws of the clip before it is closed (Fig. The Falope ring and Hulka and Filshie clips cannot be applied if the tube is thickened from previous salpingitis. This can be prevented by bathing the tubes with a few milliliters of 2% lidocaine just before ring placement. Failures of the Falope ring or the clips generally result from misapplication, and pregnancy, if it occurs, is usually intrauterine. After bipolar sterilization, pregnancy may result from tuboperitoneal fistula and is ectopic in more than 50% of cases. If inadequate electrical energy is used, a thin band of fallopian tube remains that contains the intact lumen and allows intrauterine pregnancy to occur. Thermocoagulation, the use of heat probes rather than electrical current, is employed extensively in Germany for laparoscopic tubal sterilization but is little used in the United States. The most common significant complication was unintended laparotomy for sterilization after intra abdominal adhesions were found. In another series, 2,827 laparoscopic sterilizations were performed with the Silastic band using local anesthesia and intravenous sedation (286). Risk of death with female sterilization was 1 to 2 per 100,000 sterilizations in the last national study that was based on data from 1979 to 1980 (281). Almost half of the deaths were from complications of general anesthesia, usually related to the use of mask ventilation. When general anesthesia is used for laparoscopy, endotracheal intubation is mandatory because the pneumoperitoneum increases the risk of aspiration. International data from the Association for Voluntary Surgical Contraception show a similar record of safety from third world programs: 4. Contraception should be continued until the day of surgery, and a sensitive pregnancy test should be routinely performed on the day of surgery. Because implantation does not occur until 6 days after conception, a woman could conceive just before the procedure and there would be no way to detect it. Scheduling sterilization early in the menstrual cycle obviates the problem but adds to the logistic difficulty. Another cause of failure is the presence of anatomic abnormalities, usually adhesions surrounding and obscuring one or both tubes. An experienced laparoscopic surgeon with appropriate instruments usually can lyse the adhesions, restore normal anatomic relations, and positively identify the tube. In some circumstances successful sterilization will not be possible by laparoscopy, and the surgeon must know before surgery whether the patient is prepared to undergo laparotomy, if necessary, to accomplish sterilization. The true failure rates for 10 years obtained by the life-table method are given in Table 10. Pregnancies resulting from sterilization during the luteal phase of the cycle in which the surgery was performed were excluded. The most effective methods at 10 years were unipolar coagulation at laparoscopy and postpartum partial salpingectomy, generally a modified Pomeroy procedure. The Filshie clip was not evaluated because it was not in use in the United States at the time. Younger women had higher risk for failure, as would be expected because of their greater fecundity. The important difference was in the application technique of the electric energy to the tubes. Women whose bipolar procedure involved coagulation at three sites or more had low 5-year failure rates (3. Family Health International reported large randomized multicenter trials of the different means of tubal sterilization. A total of 2,126 women were studied, of which 878 had either clip placed by minilaparotomy and 1,248 had either clip placed by laparoscopy. This same group compared the Filshie clip with the Silastic tubal ring in a similar study with a total of 2,746 women, of which 915 had the devices placed at minilaparotomy and 1,831 at laparoscopy (290). Pregnancy rates at 12 months were the same for the Filshie clip and the tubal ring: 1. The Filshie clip was expelled spontaneously from the vagina by three women during the 12 months of follow-up. Both methods can be provided in an office setting, with only local anesthesia or conscious sedation and both offer the prospect of greater safety, lower cost, and greater long-term effectiveness than the best laparoscopy methods. To insert the device, a hysteroscope is introduced into the uterine cavity, which is distended with saline. Once in place, an outer sheath is retracted, releasing the outer coils, which expand to anchor the device in the interstitial portion of the tube. The delivery wire is detached and removed and the procedure repeated for the other tube. When properly placed, three to eight of the end coils of the microinsert are visible inside the uterine cavity. A nonsteroidal anti-inflammatory drug is given 1 to 2 hours before the procedure to decrease tubal spasm. Over time fibrous tissue grows into both devices, occluding the tubes permanently. The patient with transcervical sterilization should continue to use a reliable method of contraception until successful occlusion is documented. These consisted of vasovagal responses, cramping, nausea, and vaginal spotting (297). Possible but uncommon risks of the hysteroscopic tubal sterilization methods include perforation by the device at insertion and expulsion of the device. Other potential combinations with transcervical sterilization are related to the hysteroscopy procedure, not the tubal occlusion process. These include hypervolemia, injury to surrounding organs, bleeding, and infection and occur in less than 1% of cases. An additional 20 women had second-look hysteroscopy because of persistent abnormal vaginal bleeding.
In a small study medicine 5113 v cheap septra online master card, sexually functional surgically menopausal women receiving no hormonal therapy viewed erotic videos during functional magnetic resonance imaging symptoms xxy generic 480 mg septra free shipping. The women failed to show the brain activation typical of premenopausal women and also typical of themselves when they were treated with both testosterone and estrogen treatment shingles purchase septra 480 mg line, and yet treatment modalities septra 480mg mastercard, they reported sexual arousal from the erotic videos without medicine q10 purchase 480mg septra visa, and with symptoms 13dpo 480mg septra with amex, hormonal supplementation (22). Accompanying the subjective excitement and erotic feelings of arousal are a number of physical changes. With sexual stimulation, brain activity in the hypothalamus and other areas influencing the genital response are activated, triggering the autonomic nervous system to allow increased blood flow to the vagina. Vasodilatation of the arterioles in the submucosal vaginal plexus increases transudation of interstitial fluid, which moves from capillaries between the epithelial intercellular spaces and into the vaginal lumen. Simultaneously, the autonomic nervous system allows relaxation of the smooth muscle cells surrounding blood spaces (sinusoids) in the extensive clitoral tissue and labia, causing clitoral swelling and vasodilatation in the labia. Recent immunohistologic studies indicate nerves containing nitric oxide are present in the genital skin covering the clitoris and labia (5). With arousal, the vagina lengthens, distends, and dilates, and the uterus elevates out of the pelvis. The breasts become more engorged, the skin more mottled, and the nipples more erect. The neurobiology of arousal is incompletely understood but the genital vasocongestive responses appear to be highly automated, occurring within seconds of an erotic stimulus (23). The parasympathetic and sympathetic nervous systems and the somatic system function less independently than was previously believed. Communication was identified between the cavernous nerves to the clitoris, containing nitric oxide, and the distal portion of the (somatic) dorsal nerve of the clitoris from the pudendal nerve (5). Nitric oxide is thought to be the major neurotransmitter involved in vulvar engorgement (5,25). Even in women without any sexual dysfunction, there is highly variable correlation between the degree of subjective sexual excitement and the increase in congestion around the vagina (23,26). This poor correlation was shown repeatedly over the past 30 years based on psychophysiologic studies using the vaginal photoplethysmograph. Congestion in response to a sexual video is reduced in women with disruption of the autonomic nerve supplying the vulva and vagina. Otherwise healthy women experiencing chronic lack of arousal (including lack of subjective excitement and lack of any awareness of genital congestion) show increases in vaginal congestion from erotic stimuli that are similar those in control women (23,26). With the so-called cervico-motor reflex, cervical touch (in the laboratory with a balloon-tipped catheter to replicate penile pressure) leads to a reduction in pressure in the upper portion of the vagina and an increase in pressure in the middle and lower portions. Simultaneously, an increase in electromyographic activity in the levator ani and puborectalis muscles was recorded. A further reflex demonstrated in laboratory studies shows reduced uterine tone in response to mechanical or electrical stimulation of the glans of the clitoris. Background activity of the uterine muscle was abolished by clitoral stimulation if either the glans clitoris or the uterus was anesthetized. This reflex may underlie the known increase in size and the elevation of the uterus with sexual arousal (28). Orgasm Orgasms is a brain event, typically triggered by genital stimulation that can occur during sleep or from stimulation of other body parts including the breast and nipple or by fantasy, occasionally by medication, and in spinal cord injured women by vibrostimulation of the cervix. In able-body women, it involves a myotonic response of smooth and striated muscle associated with feelings of sudden release of the sexual tension built up during arousal. Some women may subjectively perceive uterine contractions during orgasm and some may report a difference in their perception of orgasm after hysterectomy, but this is not objectively documented. An objective quantitative measure was established that shows strong correspondence with the subjective experience of orgasm. Analysis of rectal pressure data while volunteers imitated orgasm, tried to achieve orgasm and failed, or experienced orgasm showed a significant and important difference in this analysis between orgasm and both control tasks (29). Brain imaging studies of women during orgasm showed brain activations and deactivations similar but not identical to those found in men (30). This area is activated when experiences are particularly hedonic, with further activation increasing satiation and deactivated with feelings of satiety. The latter is deactivated during the genital stimulation and arousal and remains deactivated during orgasm. The subjective description of orgasm is very much in keeping with this depiction (31). The majority of women most easily experience orgasm from direct clitoral stimulation. More direct contact with the clitoris is possible from contact of pubis to pubis after the man has ejaculated and penile size is reduced, if the man maintains contact. The bodies are more closely approximated and the woman can move her pelvis on his at a rate that is most conducive to her orgasm. Breast stimulation, kissing, and clitoral stimulation during intercourse are other commons means of experiencing orgasm. Women are potentially multiorgasmic, capable of experiencing a number of orgasms close together during one sex response cycle and of resuming sexual activity without any refractory period. Resolution Following the sudden release of sexual tension brought about by orgasm, women experience a feeling of relaxation and well-being. The gradual lessening of pelvic engorgement contrasts with the quicker loss of penile firmness in men. Nongenital changes that took place during arousal are reversed, and the body can return to a resting state after some 5 to 10 minutes. With further stimulation, the response can resume before or after this resting state is reached. Women who enjoy arousal without orgasm and without any sense that orgasm is very close but frustratingly absent report a similar sense of well-being and relaxation. These factors include mood; age; relationship duration and quality; personal psychological factors stemming from relationships in childhood with parental figures; previous losses, traumas, and ways of coping with emotions; illness; and use of medication, alcohol, and illicit drugs. One study of women, where a diagnosis of clinical depression was excluded, showed a strong association between decreased sexual interest and self-reporting of negative emotional and psychological feelings, including low self-esteem, feelings of insecurity, and lost femininity (18). Impaired sexual desire is noted in most studies of women with depression, even before the administration of antidepressants with sexually negative side effects (35). Paradoxically, depressed women may masturbate more frequently than women who are not depressed, despite an increased prevalence of dyspareunia and difficulties with arousal and orgasm in partnered sex (38). Self stimulation may cause calmness, relaxation, and improved sleep and in women is often not a consequence of sexual urge or desire. Some studies showned little increase in sexual problems with age, whereas in others almost 40% of the sample reported reductions in responsiveness and an increased desire for nongenital sexual expression (13,39,40). In one study, the prevalence of reduced desire increased significantly as a function of both menopause status and age, from 22% in the premenopausal group to 32% in the postmenopausal group (41). Low levels of desire were strongly associated with other sexual problems, including difficulties with arousal and orgasm. One large cohort of women studied over 10 years from peri to postmenopause showed a decline in desire and responsiveness as a function of both age and menopause (42). The number of menopausal symptoms experienced influenced well-being, which in turn affected sexual responsiveness and sexual desire and interest. Many studies of sexuality and aging show that older women report less distress about lack of desire when compared with younger women (17,18,43). In a nonclinical study of 102 women, the determinants of sexual satisfaction in those younger than 45 years of age were compared with those of women older than 45 years of age (18). There was no difference in sexual satisfaction achieved either by intercourse or noncoital sexual activities. Older women reported lower frequency of orgasm and different ratings on certain dimensions of sexual satisfaction. For the older women, the dominant qualities important to their satisfaction were those related to an emotional sense of calm and to factors such as feeling secure with their partner, whereas for younger women the subjective physical experience was more important. Despite reports of reduced sexual interest and desire by some older women, most retain some interest and maintain the potential for sexual pleasure for their entire lives. In older women, a strong predictor of continued sexual interest is sexual behavior and enjoyment at an earlier age. A discrepancy between sexual interest and actual sexual activity occurs in many cases because an adequate partner is no longer available. In other instances, the cessation of sexual activity with age is more an expression of emotional problems resulting from lack of tenderness, communication, and attraction. If intercourse is perceived as a necessary component of sexual activity with a partner, some older women will lose motivation and interest as a result of discomfort and dyspareunia associated with lack of estrogen. Although the increase in vaginal congestion in response to visual sexual stimulation is similar in women with and without estrogen, baseline vaginal blood flow is lower in estrogen-deficient women (23). There may be loss of elasticity and thinning of the vaginal epithelium, which becomes vulnerable to damage from intercourse. Estrogen depletion predisposes women to vulvar vaginitis and urinary tract infections, both of which contribute to dyspareunia and reduce sexual self-image. Women who remain sexually active, alone or with a partner, may have less vulvar and vaginal atrophy than sexually inactive women but may still be symptomatic (47). Adrenal production of testosterone precursors gradually decreases with age, beginning in the late 30s. Available assays were not sufficiently sensitive in the female range of serum testosterone to detect particularly low levels. When mass spectroscopy was used: serum testosterone levels were similar in 121 women carefully assessed and diagnosed with disorders of low desire and arousability to levels in 125 women similarly carefully assessed but to exclude any sexual dysfunction (50). The association is weaker than that between male erectile dysfunction and hypertension, hyperlipidemia, diabetes, and coronary artery disease. Depression is the major factor influencing sexual function in women with chronic illness including end-stage renal disease (51), multiple sclerosis (52), or diabetes (53). Personality Factors Studies show that, compared with functional women, those who have concerns about low levels of desire and arousability are characterized as having vulnerable self-esteem, high levels of anxiety and guilt, negative body image, introversion, and somatization (18). The clinical impression of women with orgasmic disorder is that many are extremely uncomfortable in conditions in which they are not in control of circumstances or their bodily reactions. For many women with vaginismus, there is a phobic quality to the fear of vaginal penetration. Many women with provoked vestibulodynia show a marked fear of negative evaluation by others, ultra conscientiousness, and self-criticism, as well as an increase in somatization and anxiety (54). Relationships Most women who report loss of desire and arousability to physicians indicate that their partnerships are stable and satisfactory. The loss of sexual spontaneity resulting from the goal-oriented approach to sex while trying to conceive with scheduled intercourse (coinciding with ovulation naturally or after hormonal stimulation) may lead to sexual dysfunction and is considered a major problem for many women (57). The stress of testing and waiting for results may disrupt emotional intimacy, causing further damage to sexual function. Often there are unresolved feelings of guilt over personal responsibility for the infertility and feelings of resentment of the multiple procedures required for women compared with one semen analysis for men.