Bernard Lopez, M.D.
- Assistant Professor
- Thomas Jefferson Medical College
- Thomas Jefferson University Hospital
- Philadelphia, PA
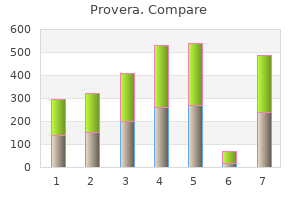
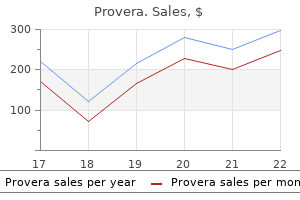
Liver toxicity was seen at a higher frequency in the azathioprine group whereas aStrength of recommendation D; level of evidence 3; bStrength of recommendation infections appeared more common in patients treated with B; level of evidence 1 (see Appendix 1) pregnancy ultrasound order provera visa. For the group of of one of these studies18 suggested that mycophenolate may be patients who have incomplete control with oral prednisolone more effective in achieving disease control than azathioprine pregnancy kit cost purchase 10 mg provera with mastercard. Azathioprine is licensed for use in systemic lupus erythematosus menopause patch provera 10 mg discount, and there is evidence to indicate superiority for mainteInammatory skin diseases nance compared with cyclophosphamide menopause yellow discharge order provera amex, following induction in patients with lupus nephritis women's health clinic flinders buy provera no prescription. Both studies used the drug as oral monotherapy in Azathioprine appears effective as a second-line agent in moderate-to-severe womens health kalamazoo mi cheap provera 5mg with mastercard, refractory disease. This is an important study, as the sample size was large, the design was prospective, and the result was statistically signicant. With this came the parallel understanding that the concomitant high levels of ple measures such as dose adjustment. Patients with true azathioHypersensitivity can manifest with generalized or organprine hypersensitivity also exhibit nausea as part of a wider specic symptoms. Fever, myalgia, arthralgia and nausea are common features; more rarely hepatitis, interstitial nephritis77 symptom complex, but management of these patients is differor renal failure78 are seen. Nausea early in the course of 79 azathioprine treatment is common and usually resolves after a shock can occur. This tendency is described, but it is possible that some reported eruptions, such as erythema nodosum,80 relate to the underlying condireected in the empirical approach of gradual dose escalation which has been practised by prescribers for years. If symptoms of hypersensitivity were escalation, one-quarter of patients had nausea which limited severe, then rechallenge in a hospital setting with access maximum achievable dose or resulted in treatment withto resuscitation facilities is advised. If sensitivity is directed against the imidazole rather than the these strategies fail, then there is also evidence that switching thiopurine moiety of the azathioprine molecule. Mild lymphopenia is quite comAzathioprine hypersensitivity is an idiosyncratic, immunologimonly seen in patients receiving thiopurines90 and this may cally mediated reaction that presents with a distinct symptom be a relevant factor. It is probably azathioprine in conjunction with other immunosuppressants underdiagnosed, as symptoms are easily confused with infecdo have an increased risk of infections, presumably due to the tion or underlying disease. Varicella zoster virus 75 serious adverse event, although fatality appears to be rare. Nevertheless, initial dose may cautiously be prescribed again with more this remains a theoretical risk and careful selection of patients frequent monitoring of liver blood tests thereafter. The following approaches should be used if abnorthe treatment of some inammatory skin diseases. For new transplant patients, superseding more traditional therapies such as thiopurines. In management should be proactive with education about sun contrast, epidemiological data on the long-term toxicity of protection beginning at the time of (or even before) transthiopurines are available from several medical disciplines. The co-prescription of several immunosuppressants in munosuppressants in solid-organ transplant recipients increases this situation is likely to be a major contributor to this the risk of developing several malignancies, with non-Hodgrisk,100,101 which may be elevated more than 200-fold. Although there are no studies addressing ular lymphoma, in nontransplant patients treated with azathiothis issue for inammatory skin disease, the results from the prine monotherapy is controversial. Two meta-analyses have addressed the Considerable progress has recently been made in determinissue and the conclusions are conicting. It should be emphasized that collecto patients with dermatoses that may require prolonged tively the number of heterozygous range patients in these azathioprine therapy. Consequently, these recommendations term risk, this would appear to be low in absolute terms. Furshould serve as a guide for current use, in anticipation of inthermore, studies of azathioprine use in the short-to-medium formation from future studies with larger patient numbers. The evidence 4) dose should be adjusted within these limits depending on response and haematological tolerance, with subsequent reduction for maintenance therapy following clinical response. Pregnancy is a relafor use or whether monotherapy or combination with oral tive contraindication (see section 10. A strategy for dose reduction for azathioprine are advised to not breastfeed their infants, patients in remission has not been addressed in studies of deralthough more recent data suggest this may be safe (see secmatological diseases, and remains a matter for empirical titration 10. A similar survey among gast119 enhanced toxicity in the presence of renal insufficiency. Azathioprine dose does not need to activity may be induced by thiopurines and that consequent130 be altered in those undergoing haemodialysis. Furthermore, the enzyme activity; this terminology is adhered to throughout development of acute liver failure in previously well carriers of these guidelines). Prince screened more frequently, and in some European centres (Manchester Royal Inrmary, Manchester, U. Data from the renal transplant population (receiving multiple immunosuppressive agents) suggests a vefold increase in the prevalence of abnormal cervical cytology 10. Similar guidelines do not exist for azathioprine use in other contexts, but given what is now known about the risks of 10. However, a degree of impaired cellular immunity may Food and Drug Administration categorizes azathioprine as risk also occur with azathioprine [G. Spickett (Royal Victoria Inrgroup D, indicating positive evidence of fetal risk is available, mary, Newcastle upon Tyne, U. However, the literature is inconclusive on any Green Books advice, but difficult cases would be best disteratogenic effects. One case report rare situation when nonimmune individuals receive azathiohas even shown a healthy child born to parents who were prine and subsequently have signicant exposure to chicken both receiving thiopurines. A few drugs have important interactions with azathioprine and these are summarized in Table 3. In particular, as it is now known that the risk of photocarcinogenesis escalates with increasing duration of thiopurine the most potentially serious azathioprine drug interaction treatment (see section 9. Care should be taken with use of azathioprine in the elderly; the this issue is covered in detail in Section 13. Close monitoring of anticoagulation is advised Ribavirin Severe pancytopenia has been reported. These include succinylcholine, tubocurarine, furosemide, bendroumethiazide, nonsteroidal anti-inammatory drugs and angiotensin-converting enzyme inhibitors. A dose-dependent increase in warfarin therapy rarine, and advises that patients should inform their anaesthe(at least 25-fold) and careful monitoring of coagulation is tist prior to receiving a general anaesthetic. The is based on studies performed with supratherapeutic doses of exact mechanism of the interaction is unknown. Nevertheless, the following general principles for examples are co-trimoxazole, trimethoprim and clozapine. It is attenuated vaccines to immunocompromised individuals and therefore crucial that they are provided with a complete and such vaccines are therefore contraindicated in patients receiving balanced overview of the advantages and disadvantages of azathioprine. Inacpotential health risks may be an unnerving experience for any tivated vaccines are safe in immunocompromised patients. It is essential, therefore, that the patient is both azathioprine-treated individuals should receive pneumococcal fully informed and takes part in the decision-making process. Studies in transplant Initial discussion typically involves a broad-brush approach recipients receiving azathioprine have shown this group to which attempts to give the patient some basic information mount a similar antibody response to healthy controls. Alternative immunosuppressant drugs which may be prescribed at a later date in the event of a poor therapeutic response or side-effects with azathioprine should also 10. The dermatologist must not overdramatize starting such treatment for fear of causing unnecessary alarm. Often, the patient will not remember 3 Explain if usage is for a licensed or unlicensed indication. Deci4 Advise patients to seek urgent medical attention if they sion-making may require careful thought over a period of develop signs or symptoms of azathioprine hypersensitivity, time, sometimes with more than one consultation to discuss bone marrow suppression or liver impairment. The need for a warn patient about: period of consideration is aided by the fact that the onset of a (a) High fever severe u-like illness therapeutic response with azathioprine is usually slow, and it (b) Unexplained bruising (c) New-onset jaundice is seldom necessary to prescribe this drug in haste. A detailed knowledge of the hazards of azathioprine (c) Liver blood tests treatment (see section 9. The clinician must then tread a ne line 9 Discuss the possible increased risk of malignancy with longbetween assessing the need for azathioprine treatment and term use (section 9. Otherwise, this 10 Give advice on sunscreens and sun avoidance could deter some patients with debilitating conditions from 11 Caution regarding avoidance of pregnancy (section 10. Patient exare sufficiently compensated for by a positive therapeutic pectations need to be realistic response. The dermatologist should enquire about the patients 2 Emphasize the need for toxicity monitoring with regular blood general health and other possible comorbidities that might be tests. Patients unable to comply should not be given the drug relevant to azathioprine usage. Patients also appreciate discussion of their blood test results; even if these are normal, being Recommendations: toxicity monitoring kept up to date provides valuable reassurance. Finally, the dermatologist should repeat advice about photoprotection, emphasizing the importance of compliance during the summer months and while on sunny holidays. With mutual agreement, responsibility is someAzathioprine is relatively inexpensive compared with other times shared with the patients general practitioner according immunosuppressive drugs used by dermatologists such as to protocols agreed locally. The azathioprine datasheet recommends the more cautious approach of an a 50-tablet pack of mycophenolate mofetil 500 mg is curinitial 8 weeks of weekly monitoring. Leucopenia ing is around 30; this cost may fall with further renements is the most common haematological adverse event. Berg (City Hospital, Birmingham, haematological side-effects include anaemia, thrombocytopenia U. Some studies have shown that levels of other Personal genomic screening is a relatively new type of metabolites (see. However, in rouWe are very grateful to the following people for their advice tine clinical practice, the combination of azathioprine and and input in the preparation of the manuscript: Andrew Damallopurinol is relatively contraindicated and the previous versell, patient representative; Dr Martin Prince, Consultant Hepasion of this guideline advised against concomitant use due tologist, Manchester Royal Inrmary, Manchester, U. Writing a British Association of Dermatol180,181 ogists clinical guideline: an update on the process and guidance dated. Pharmacogenetics of (Strength of recommendation D; level of evidence 4) acute azathioprine toxicity: relationship to thiopurine methyltransferase genetic polymorphism. Genetic variation in response to 6-mercaptopurine for childhood acute lymphoblastic 14. Thiopurine S-methyltransferase pharClinicians prescribing azathioprine should use audit to evaluate macogenetics: insights, challenges and future directions. Long-term maintenance treatment ized controlled open-label trial of four treatment regimens for of moderate-to-severe plaque psoriasis with iniximab in compemphigus vulgaris. Lupus 2005; 14 (Supmaintenance therapy for vasculitis associated with antineutrophil pl. Successful treatment of oprine treatment in patients with rheumatoid arthritis compligeneralized discoid skin lesions with azathioprine. No induction of thiopurine of relapses and survival of 73 patients with juvenile or adult dermethyltransferase during thiopurine treatment in inammatory matomyositis. Drug therapy in juvenile dermato49 Tassaneeyakul W, Srimarthpirom S, Reungjui S et al. Thiopurine methyltransferase ylprednisolone plus azathioprine or mycophenolate mofetil for activity and the use of azathioprine in inammatory bowel disthe treatment of bullous pemphigoid. Comparative effectiveness of azathioprine or mycotransferase genetic polymorphism a major factor for withdrawal phenolate mofetil as an adjuvant for the treatment of bullous of azathioprine in rheumatoid arthritis patients Azathioprine therapy and monitoring of thiopurine drugs in patients with inammatory adverse drug reactions in patients with inammatory bowel disbowel disease or autoimmune hepatitis. Eur J Gastroenterol Hepatol ease: impact of thiopurine S-methyltransferase polymorphism. Thiopurine methyltransferase ment should be considered in azathioprine intolerant patients enzyme activity determination before treatment of inammatory with inammatory bowel disease. Azathioprine induced acute and severe myelosuppression during azathioprine therapy. Azathioprine hypersensiyltransferase levels to exclude patients at high risk of tivity: report of two cases and review of the literature. Erythema methyltransferase activity and the efficacy and or side effects of nodosum-like eruption as a manifestation of azathioprine hyperazathioprine therapy in dermatologic patients. Thioguanine nucleotides tory bowel disease and successful subsequent treatment with and thiopurine methyltransferase in immunobullous diseases: mercaptopurine.
Aedes eggs can withstand desiccation breast cancer 2a prognosis provera 5mg otc, the intensity and duration of which varies menopause discharge discount provera online master card, but in many species they can remain dry women's health center baytown generic provera 5 mg without a prescription, but viable womens health pt buy provera 5mg without prescription, for many months womens health boise cheap provera amex. When flooded women's health center robinwood hagerstown md order provera american express, some eggs may hatch within a few minutes, others of the same batch may require prolonged immersion in water, thus hatching may be spread over several days or weeks. Even if environmental conditions are favorable, eggs may be in a state of diapauses and will not hatch until this resting period is terminated. Various stimuli including reduction in the oxygen content of water, changes in day length, and temperature may be required to break diapauses in Aedes eggs. Many Aedes species breed in small containerhabitats (tree-holes, plant axils, etc) which are susceptible to drying out, thus the ability of eggs to withstand desiccation is clearly advantageous. Desiccation and the ability of Aedes eggs to hatch in installments can create problems with controlling the immature stages Larvae Aedes species usually have a short barrel-shaped siphon, and there is only one pair of sub ventral tufts which never arise from less than one-quarter of the distance from the base of the siphon. Additional characters are at least three pairs of setae in the ventral brush, the antennae are not greatly flattened and there are no enormous setae on the thorax. These characters should separate Aedes larvae from most of the culicine genera, but not unfortunately from larvae of South American Haemagogus. In central and South America, Aedes larvae can usually be distinguished from those of Haemagogus, by possessing either larger or more strongly speculate antennae; also the comb is not on a sclerotized plate as in some Haemagogus. Aedes aegypti, often called the yellow fever mosquito, is readily recognized by the lyre shaped silver markings on the lateral edges of the scutum. Scales on the wing veins of Aedes mosquitoes are narrow, and are usually more or less all black, except may be at the base of the wing. In Aedes the abdomen is often covered with black and white scales forming distinctive patterns, and in the female it is pointed at the tip. Yellow fever Yellow fever is a zonoosis, essentially a disease of forest monkeys, which occasionally transmitted to humans. The yellow fever virus 54 mainly occurs in population of monkeys in dense forests and the disease is transmitted from monkey to monkey by forest dwelling mosquitoes called Aedes africanus in Africa, heamagogus and sabeths in south and central America Yellow fever. There are two epidemiological types of the disease, urban and jungle yellow fever. The same virus causes both types, but the mosquito vectors and vertebrate hosts are quite different. Transmission In Africa the yellow fever virus occurs in certain cercopithecid monkeys inhabiting the forest and is transmitted amongst them mainly by Aedes africanus. This sylvatic, forest or monkey cycle, as it is sometimes called, maintains a reservoir in the monkey population (Figure 2. Some species of monkeys involved in the forest cycle, such as the red-tailed guenon, descend from the trees to steal bananas from farms at the edge of 55 the forest in this habitat, the monkeys get bitten by different mosquito including Aedes bormeliae (formerly called Ae. This species bites during the day at the edges of forest and breeds in leaf axils of bananas, plantains and other plants such as cocoyams (Colocasia) and pineapples. If the monkeys have viraemia, that is yellow fever virus circulating in their peripheral blood, Ae. Bromeliae becomes infected, and if the mosquito lives long enough it can transmit yellow fever to other monkeys or more importantly to people. This transmission cycle, occurring in clearings at the edge of the forest involving monkeys, Ae. When people return to their villages they get bitten by different mosquitoes, including Ae. Aegypti, a domestic species breeding mainly in man made containers such as water-storage pots, abandoned tin cans and vehicle tyres. There is increasing evidence in West Africa that in rural areas other Aedes species spread the virus from monkeys to people. In some areas for example, yellow fever may be circulating among the monkey population yet rarely gets transmitted to humans because local vector mosquitoes are predominantly zoophagic. Other primates in Africa such as bush56 babies (Galago species) may also be reservoirs of yellow fever. There is some evidence from West Africa that yellow fever virus may be trans-ovarially transmitted in Aedes species, as males have been found infected with the virus. Thus, after 4 or 5 days the virus appears in the peripheral blood, that is viraemia is produced, and this occurs irrespectively of whether monkeys or humans are showing overt symptoms of the disease. Viraemia lasts only 2-3 days, after which the virus disappears from the peripheral blood never to return and the individual is immune. Monkeys and people are therefore infective to mosquitoes for only about 2-3 days in their entire lives. A relatively high titre of yellow fever (and also any other arbovirus) is needed before it can pass across the gut cells of the mosquito into the haemolymph, from where it invades many tissues and organs, including the salivary glands, where virus multiplication occurs. This is the extrinsic cycle of development and can take 5-30 days, depending on temperature, the type of virus and the mosquito species, but in yellow fever, and most other mosquito-borne viral infections, the incubation period is typically 12-15 days. A mosquito must therefore live a sufficiently long time before it becomes infective and capable of transmitting an arbovirus-or malaria or filariasis. It is characterized by a sudden high fever, severe headache, backache and pain in the joints. There are four strains or types 58 and at least one or all four are found throughout much of the world. Recovering victims are generally immune to future infections, but only from the strain they were infected with. Therefore, a person can potentially experience all four different strains of dengue. Important Species of Aedes Aedes aegypti is a small dark species easily identified by the lyreshaped, silvery-white lines on the thorax and the white bands on the tarsal segments. It is a vector of urban yellow fever and dengue, and it is a pest when present in large numbers. Aedes aegypti is essentially a tropical species, probably introduced into the Western World from Africa. This is a thoroughly domesticated mosquito and breeds almost exclusively in artificial containers in and around human habitations. The females lay their eggs singly on the water just at the margin, or on the sides of the container above the water line. They prefer human blood to that of other animals and readily enter homes to find suitable hosts. It attacks quietly, preferring to bite around the ankles, under shirt sleeves, or on the back of the neck. Adults can have a golden-brown color on top of the thorax and a longitudinal stripe of white or yellowish-white scales on the abdomen. Females lay their eggs singly on the mud of salt marshes where they remain until 59 flooded by high tides or rains. They usually use pot holes and depressions of various sizes, but they may also lay eggs over rather extensive level areas. After having been dry for a week or two, they will hatch in a few minutes when water covers them. Aedes sollicitans adults are strong fliers and often migrate in large swarms from marshes to cities and towns many miles away. Migratory flights begin just before dark and may include tremendous numbers of mosquitoes. They rest among the grasses during the day but will readily attack anyone who disturbs them. This is medium-sized dark mosquito with a longitudinal line of yellowish-white scales on the upper surface of the abdomen. Aedes vexans is a mediumsized, brown mosquito with narrow rings of white scales on the hind tarsi and a V-shaped notch on the middle of each band of scales on top of the abdomen. Aedes vexans breeds in rain pools, flood waters, roadside puddles, and practically all temporary bodies 60 of fresh water. The black salt-marsh mosquito has cross bands of white scales on top of the abdomen and white rings on the proboscis and tarsi. There is no simple method of distainguishing eggs of Haemagogus from those of Aedes or psorophora mosquitoes. They resemble Aedes larvae but can usually be separated by the following combination of characters: antennae short and either without, or with only very few, spicules, a ventral brush arising from a sclerotized boss. In some species the comb teeth are at the edge of a sclerotized plate, in Aedes this plate is absent. Adults Adults are very colourful and they can easily be recognized by the presence of broad, flat and bright metallic blue, red, green or golden coloured scales, covering the dorsal part of the thorax. Like Sabethes mosquitoes they have exceptionally large anterior pronotal thoracic lobes behind the head. Haemagogus adults are rather similar to Sabethes in other respects, and it may be difficult for the novice to separate these two genera. However, no Haemoagogus mosquito has paddles on the legs, which is a conspicuous feature of many, but not all, species of Sabethes. Larvae occur mostly in tree-holes and bamboo stumps, but also in rock-pools, split coconut shells and sometimes in assorted domestic containers. Adults bite during the day, but mostly in the tree tops where they feed on monkeys. Under certain environmental conditions, however, such as experienced at edges of forests, during tree felling operations or during the dry season, they may descend to 62 the forest floor to bite humans and other hosts. Eggs Little is known about the eggs of Sabethes species, but it appears that they are laid singly, have no prominent surface features such as bosses or sculpturing and are incapable of withstanding desiccation. The eggs of sabethes chloropterus, a species sometimes involved in the sylvatic cycle of yellow fever, are rhomboid in shape and can thus be readily identified from most other culicine eggs. Larvae the siphon has many hairs placed ventrally, laterally or dorsally, and is relatively slender and moderately long. Sabethes larvae can usually be distinguished from other mosquito larvae by having only one Pair of setae in the ventral brush, the comb teeth arranged in a single row, or at most with 3-4 detached teeth, and by the absence of a pectin. Adults of many species have one or more pairs of tarsi with conspicuous paddles composed of narrow scales. Species, which lack these paddles, resemble those of Haemagogus and a specialist is required to identify them. Biology Larvae occur in tree-holes and bamboo stumps; a few species are found in leaf axils of bromeliads and other plants. They bite during the day, mainly in the tree canopy, but like Haemagogus adults, may descend to ground level at certain times to bite humans and other hosts. Eggs Eggs are dark brown-black and cylindrical, but have a tube-like extension apically which is usually darker than the rest or the egg. Eggs are laid in sticky compact masses, often arranged as a rosette, which are glued to the undersurfaces of floating vegetation. Pupae also breathe through plants, by inserting their modified respiratory trumpets into plants. Adults Typically adults have the legs, palps, wings and body covered with a mixture of dark (usually brown) and pale (usually white or creamy) scales giving the mosquito a rather dusty appearance. The speckled pattern of dark and palescales on the wing veins gives the wings the appearance of having been sprinkled with salt and pepper, and provides a useful character for identification. Closer examination shows that the scales on the wings are very broad and often asymmetrical. Biology Eggs are glued to the undersurfaces of plants and hatch within a few days; they are unable to withstand desiccation. All larval habitats have aquatic vegetation, either rooted, such as grasses, rushes and reeds or floating, such pistia stratiotes, Saluinia or Eichhornia. Larvae consequently occur in armament collections or waters, such as swamps, marshes, ponds, borrows grassy ditches, irrigation canals and even in the middle of rivers if they we floating plants. Because they are more or less permanently attached to plants the immature stages, are frequently missed in larval surveys. It is therefore not easy to identify breeding places with certainty unless special collecting procedures are undertaken, such as the collection of plants to which the immature stages are thought to be attached. It is often difficult to control breeding of Mansonia species by conventional insecticidal applications, because of the problems of getting the insecticides to the larvae, which may be some distance below the water surface. The main medical importance of Mansonia mosquitoes is as vectors of filariasis, such as nocturnal periodic and nocturnal sub periodic forms of Brugia malayi in Asia. Psorophora mosquitoes are found only in the Americas, from Canada to South America. For example, their eggs look like those of Aedes and they can withstand desiccation, and a specialist is required to distinguish the larvae and adults of the two genera. Breeding places are mainly flooded pastures and sometimes rice fields; larvae of several species are 66 predators. Although they can be vectors of a few arboviruses, such as Venezuelan equine encephalomyelitis, their main importance is as vicious biters; some pest species can be very large. The need for surveys: Whether pest managers are aligned with a medical or engineering organization, its essential to conduct mosquito surveys to determine the species present, their abundance, their potential as disease vectors, and to collect enough information to base a pest management program on. Surveys should be a continuing part of the pest management program to evaluate the effectiveness of pest management actions. They will also help determine the effectiveness of pest management actions and anticipate increases or decreases in operations relative to changing mosquito populations. To adequately conduct mosquito surveys, the first thing needed is an adequate map Use it to become familiar with the area, locate breeding places for all developmental stages of mosquitoes and establish good sites for sampling stations. Larval surveys show the exact areas where mosquitoes are breeding, so they have special value in guiding mosquito management operations. Identify and mark the map for regular larval dipping stations, then inspect them periodically throughout the breeding season. Also, conduct random larval samplings in the control area to check the effectiveness of larviciding operations. Larval stations may be barrels, small pools, ditches, 67 drains, ponds or almost any type of water collection.
Routine antimicrobial susceptibility testing of S aureus strains historically did not include a method to detect strains susceptible to clindamycin that rapidly become clindamycin-resistant when exposed to this agent women's health clinic pei cheap provera 5 mg otc. Typing womens health fresno ca buy provera pills in toronto, in conjunction with epidemiologic information women's health center of lynchburg va order provera on line amex, can facilitate identifcation of the source menstrual upset stomach purchase provera 10mg amex, extent pregnancy lower back pain generic 10mg provera with amex, and mechanism of transmission in an outbreak women's health center bakersfield purchase 5mg provera otc. Antimicrobial susceptibility testing is the most readily available method for typing by a phenotypic characteristic. Firstor second-generation cephalosporins (eg, cefazolin or cefuroxime) or vancomycin are effective but less so than nafcillin or oxacillin, especially for some sites of infection (eg, endocarditis, meningitis). A patient who has a nonserious allergy to penicillin can be treated with a frstor second-generation cephalosporin, and if the patient is not also allergic to cephalosporins, with vancomycin or with clindamycin, if endocarditis or central nervous system infection is not a consideration and the S aureus strain is susceptible. Drainage of abscesses and removal of foreign bodies is desirable and almost always is required for medical treatment to be effective. Initial antimicrobial therapy should include a parentally administered beta-lactam antistaphylococcal antimicrobial agent and a protein synthesis-inhibiting drug, such as clindamycin, at maximum dosages. Once the organism is identifed and susceptibility is known, therapy for S aureus should be modifed, but an active antimicrobial agent should be continued for 10 to 14 days. Administration of antimicrobial agents can be changed to the oral route once the patient is tolerating oral alimentation. The total duration of therapy is based on the usual duration of established foci of infection (eg, pneumonia, osteomyelitis). Aggressive drainage and irrigation of accessible sites of purulent infection should be performed as soon as possible. All foreign bodies, including those recently inserted during surgery, should be removed if possible. Skin and soft tissue infections, such as impetigo or cellulitis attributable to S aureus, can be treated with oral penicillinase-resistant betalactam drugs, such as cloxacillin, dicloxacillin, or a frstor second-generation cephalosporin. In this situation, or for the penicillin-allergic patient, trimethoprim-sulfamethoxazole, doxycycline in children 8 years of age and older, or clindamycin can be used if the isolate is susceptible. Trimethoprim-sulfamethoxazole should not be used as a single agent in the initial treatment of cellulitis, because it is not active against group A streptococci. Infections are more diffcult to treat when associated with a thrombus, thrombophlebitis, or intra-atrial thrombus. A longer course (eg, 7 to 10 days) is suggested if the patient is immunocompromised or the organism is S aureus; experts differ on recommended duration, but many suggest 14 days. If the patient needs a new central line, waiting 48 to 72 hours after bacteremia apparently has resolved before insertion is optimal. If a tunneled catheter is needed for ongoing care, in situ treatment of the infection can be attempted. If the patient responds to antimicrobial therapy with immediate resolution of the S aureus bacteremia, treatment should be continued for 10 to 14 days parenterally. If blood cultures remain positive for staphylococci for more than 3 to 5 days or if the clinical illness fails to improve, the central line should be removed, parenteral therapy should be continued, and the patient should be evaluated for metastatic foci of infection. Vegetations or a thrombus in the heart or great vessels always should be considered when a central line becomes infected. Transesophageal echocardiography, if feasible, is the most sensitive technique for identifying vegetations. However, contact precautions should be used for patients with abscesses or draining wounds that cannot be covered, regardless of staphylococcal strain, and should be maintained until draining ceases or can be contained by a dressing. Prophylactic administration of an antimicrobial agent intraoperatively lowers the incidence of infection after cardiac surgery and implantation of synthetic vascular grafts and prosthetic devices and often has been used at the time of cerebrospinal fuid shunt placement. Measures to prevent and control S aureus infections can be considered separately for people and for health care facilities. Community-associated S aureus infections in immunocompetent hosts usually cannot be prevented, because the organism is ubiquitous and there is no vaccine. However, strategies focusing on hand hygiene and wound care have been effective at limiting transmission of S aureus and preventing spread of infections in community settings. Specifc strategies include appropriate wound care, minimizing skin trauma and keeping abrasions and cuts covered, optimizing hand hygiene and personal hygiene practices (eg, shower after activities involving skin-to-skin contact), avoiding sharing of personal items (eg, towels, razors, clothing), cleaning shared equipment between uses, and regular cleaning of frequently touched environmental surfaces. Another promising technique is the use of bleach in the bath water 2 to 3 times a week (cup per tub or 13 gallons of water) for approximately 3 months; studies are ongoing to determine whether this intervention reduces the incidence of recurrent infections. Measures to prevent health care-associated S aureus infections in individual patients include strict adherence to recommended infection-control precautions and appropriate intraoperative antimicrobial prophylaxis, and in some circumstances, use of antimicrobial regimens to attempt to eradicate nasal carriage in certain patients can be considered. Children with S aureus colonization or infection should not be excluded routinely from child care or school settings. Children with draining or open abrasions or wounds should have these covered with a clean, dry dressing. Routine hand hygiene should be emphasized for personnel and children in these facilities. Careful preparation of the skin before surgery, including cleansing of skin before placement of intravascular catheters using barrier methods, will decrease the incidence of S aureus wound and catheter infections. Meticulous surgical technique with minimal trauma to tissues, maintenance of good oxygenation, and minimal hematoma and dead space formation will minimize risk of surgical site infection. Appropriate hand hygiene, including before and after use of gloves, by health care professionals and strict adherence to contact precautions are of paramount importance. The benefts of systemic antimicrobial prophylaxis do not justify the potential risks associated with antimicrobial use in most clean surgical procedures, because the risk of overall infection (most commonly caused by S aureus) is only 1% to 2%. Staphylococci are the most common pathogens causing surgical site infections, and cefazolin is the most commonly recommended drug. Preprocedure detection and eradication of nasal carriage using mupirocin twice a day for 5 to 7 days before surgery can decrease the incidence of S aureus infections in some colonized adult patients after cardiothoracic, general, or neurosurgical procedures. Use of intermittent or continuous intranasal mupirocin for eradication of nasal carriage also has been shown to decrease the incidence of invasive S aureus infections in adult patients undergoing long-term hemodialysis or ambulatory peritoneal dialysis. However, eradication of nasal carriage of S aureus is diffcult, and mupirocinresistant strains can emerge with repeated or widespread use; therefore, this treatment is not recommended for routine use. These include general recommendations for all settings and focus on administrative issues; engagement, education, and training of personnel; judicious use of antimicrobial agents; monitoring of prevalence trends over time; use of standard precautions for all patients; and use of contact precautions when appropriate. When endemic rates are not decreasing despite implementation of and adherence to the aforementioned measures, additional interventions, such as use of active surveillance cultures to identify colonized patients and to place them in contact precautions, may be warranted. When a patient or health care professional is found to be a carrier of S aureus, attempts to eradicate carriage with topical nasal mupirocin therapy may be useful. Other topical preparations for intranasal application to be considered if mupirocin fails are ointments containing bacitracin and polymyxin B or a povidone-iodine cream. To date, the use of catheters impregnated with various antimicrobial agents or metals to prevent health care-associated infections has not been evaluated adequately in children. Outbreaks of S aureus infections in newborn nurseries require unique measures of control. Application of triple dye, iodophor ointment, or 1% chlorhexidine powder to the umbilical stump has been used to delay or prevent S aureus colonization. Other measures recommended during outbreaks include reinforcement of hand hygiene, alleviating overcrowding and understaffng, colonization surveillance cultures of newborn infants at admission and periodically thereafter, use of contact precautions for colonized or infected infants, and cohorting of colonized or infected infants and their caregivers. For hand hygiene, soaps containing chlorhexidine or alcohol-based hand rubs are preferred during an outbreak. Colonized health care professionals epidemiologically implicated in transmission should receive decolonization therapy, but eradication of colonization may not occur. Purulent complications of pharyngotonsillitis, including otitis media, sinusitis, peritonsillar and retropharyngeal abscesses, and suppurative cervical adenitis, develop in some patients, usually those who are untreated. Scarlet fever occurs most often in association with pharyngitis and, rarely, with pyoderma or an infected wound. Scarlet fever has a characteristic confuent erythematous sandpaper-like rash that is caused by one or more of several erythrogenic exotoxins produced by group A streptococci. Other than occurrence of rash, the epidemiologic features, symptoms, signs, sequelae, and treatment of scarlet fever are the same as those of streptococcal pharyngitis. Streptococcal skin infections (ie, pyoderma or impetigo) can result in acute glomerulonephritis, which occasionally occurs in epidemics. Because of a variety of factors, including M nontypability and emm sequence variation within given M types, emm typing generally is more discriminating than M typing. Epidemiologic studies suggest an association between certain serotypes (eg, types 1, 3, 5, 6, 18, 19, and 24) and rheumatic fever, but a specifc rheumatogenic factor has not been identifed. Several serotypes (eg, types 49, 55, 57, and 59) are associated with pyoderma and acute glomerulonephritis. Other serotypes (eg, types 1, 6, and 12) are associated with pharyngitis and acute glomerulonephritis. These toxins act as superantigens that stimulate production of tumor necrosis factor and other infammatory mediators that cause capillary leak and other physiologic changes, leading to hypotension and organ damage. Pharyngitis and impetigo (and their nonsuppurative complications) can be associated with crowding, which often is present in socioeconomically disadvantaged populations. The close contact that occurs in schools, child care centers, contact sports (eg, wrestling), boarding schools, and military installations facilitates transmission. Foodborne outbreaks of pharyngitis occur rarely and are a consequence of human contamination of food in conjunction with improper food preparation or improper refrigeration procedures. Streptococcal pharyngitis occurs at all ages but is most common among school-aged children and adolescents. Pyoderma is more common in tropical climates and warm seasons, presumably because of antecedent insect bites and other minor skin trauma. Streptococcal pharyngitis is more common during late autumn, winter, and spring in temperate climates, presumably because of close person-toperson contact in schools. Communicability of patients with streptococcal pharyngitis is highest during acute infection and untreated gradually diminishes over a period of weeks. From a normally sterile site (eg, blood, cerebrospinal fuid, peritoneal fuid, or tissue biopsy specimen) B. Defning the group A streptococcal toxic shock syndrome: rationale and consensus defnition. Patients are not considered to be contagious beginning 24 hours after initiation of appropriate antimicrobial therapy. In streptococcal impetigo, the organism usually is acquired by direct contact from another person with impetigo. Impetiginous lesions occur at the site of breaks in skin (eg, insect bites, burns, traumatic wounds, varicella). Infection of surgical wounds and postpartum (puerperal) sepsis usually result from contact transmission. Infections in neonates result from intrapartum or contact transmission; in the latter situation, infection can begin as omphalitis, cellulitis, or necrotizing fasciitis. For impetigo, a 7to 10-day period between acquisition of group A streptococci on healthy skin and development of lesions has been demonstrated. A specimen should be obtained by vigorous swabbing of both tonsils and the posterior pharynx for culture and/or rapid antigen testing. False-negative culture results occur in fewer than 10% of symptomatic patients when an adequate throat swab specimen is obtained and cultured by trained personnel. Recovery of group A streptococci from the pharynx does not distinguish patients with true streptococcal infection (defned by a serologic response to extracellular antigens [eg, streptolysin O]) from streptococcal carriers who have an intercurrent viral pharyngitis. The number of colonies of group A streptococci on an agar culture plate also does not differentiate true infection from carriage. Cultures that are negative for group A streptococci after 18 to 24 hours should be incubated for a second day to optimize recovery of group A streptococci. Most are based on nitrous acid extraction of group A carbohydrate antigen from organisms obtained by throat swab. Specifcities of these tests generally are high, but the reported sensitivities vary considerably (ie, false-negative results occur). As with throat swab cultures, sensitivity of these tests is highly dependent on the quality of the throat swab specimen, the experience of the person performing the test, and the rigor of the culture method used for comparison. The Food and Drug Administration has approved a variety of rapid tests for use in home settings. Because of high specifcity of rapid tests, a positive test result does not require throat culture confrmation. In assessing such patients, inadequate adherence to oral treatment also should be considered. Cultures of impetiginous lesions often yield both streptococci and staphylococci, and determination of the primary pathogen is not possible. Culture is performed when it is necessary to determine susceptibility of the S aureus. In necrotizing fasciitis, imaging studies often delay, rather than facilitate, the diagnosis. Clinical suspicion of necrotizing fasciitis should prompt surgical evaluation with intervention, including debridement of deep tissues with Gram stain and culture of surgical specimens. Culture results from a focal site of infections also usually are positive and can remain so for several days after appropriate antimicrobial agents have been initiated. S pyogenes uniformly is susceptible to beta-lactam antimicrobial agents, and susceptibility testing is needed only for nonbeta-lactam agents, such as erythromycin or clindamycin, to which S pyogenes can be resistant. A signifcant increase in antibody titers to streptolysin O, deoxyribonuclease B, or other streptococcal extracellular enzymes 4 to 6 weeks after infection can help to confrm the diagnosis if culture results are negative. Prompt administration of penicillin therapy shortens the clinical course, decreases risk of suppurative sequelae and transmission, and prevents acute rheumatic fever, even when given up to 9 days after illness onset. Although different preparations of oral penicillin vary in absorption, their clinical effcacy is similar. Treatment failures may occur more often with oral penicillin than with intramuscularly administered penicillin G benzathine as a result of inadequate adherence to oral therapy.
Inhibits 10 days Schizonticidal a) Highly potent the rapid plasmodial heme for all species against sensitive development of polymerase Gametocidal for strains resistance Toxic drug-heme Pv women's health center watertown wi order generic provera line. Weak Good prophylactic Can not be used of the bi-functional schizonticidal agent for Pf or alone in the dihydrofolate action against all mixed infection 2 menstrual periods one month buy 10mg provera visa, treatment of reductasespecies menopause 38 order provera in india. Dengue viruses are transmitted to humans through the bite of infected Aedes mosquitoes menstruation questions and answers purchase provera cheap, principally Aedes aegypti women's health birth control options 5mg provera visa. Patients with dengue infection may not have specific localizing symptoms at the time of presentation menopause guidebook 7th edition generic provera 5mg otc. Moderate to a high-grade fever which is sudden in onset is a universal complaint, which lasts for up to 6 days. Patients usually experience an abrupt onset of a severe headache, retro-orbital pain, and as the name break-bone fever suggests is associated with a backache, severe myalgias. Pain in abdomen in dengue fever may be as a warning sign and suggests the need for admission and close monitoring. Causes of pain abdomen in dengue infection include stretching of liver capsule due to hepatitis, pancreatitis, acalculous cholecystitis and peptic ulcer. In patients with dengue infection, initially, there is transient flushing of the face due to capillary dilatation. After 3-6 days of onset of fever, blanchable maculopapular rash associated with itching appears. Some patients develop hemorrhagic manifestations such as petechiae, subconjunctival haemorrhages and ecchymoses with positive tourniquet test, particularly in severe dengue infection. In some cases, individual lesions may coalesce and are seen as generalized confluent erythema with rounded islands of sparing described as white islands in a sea of red. This is an important clue in the outpatient department to admit a patient of suspected dengue. A high index of suspicion is required in patients with dengue fever during convalescence about intracranial bleed when they present with altered sensorium. Increased menstrual flow (menorrhagia) as a bleeding complication in dengue infection is described in the literature as case reports. Rapid dengue antigen detection tests can be used in field settings to detect infection in less than an hour. During the primary infection with dengue virus, IgM antibody is the first immunoglobulin isotype to appear and will rise to detectable levels at around 7 days followed by IgG antibody rise. In contrast during secondary dengue infection, IgG antibody titers rise rapidly during the first week with lower titers of IgM, though detectable levels. Raised haemoglobin level, raised hematocrit, low total leucocyte count and mildly low platelet counts are initial indicators for dengue infection. Low haemoglobin occasionally can be seen due to preexisting nutritional anaemia or due to bleeding manifestations. Leucocytosis should not be ignored in a case of diagnosed dengue infection as it may indicate a secondary bacterial infection. It is characterized by hepatomegaly and mild to moderate increase in transaminase levels although jaundice and acute liver failure are uncommon. Complete urine examination may 22 reveal hematuria and albuminuria in some patients. General principles management of dengue include Treatment of dengue is dynamic involving initial treatment and reassessment periodically till patient completes critical phase. These are patients who are able to tolerate adequate volumes of oral fluids and pass urine at least once every six hours and do not have any of the warning signs, particularly when the fever subsides. Adequate oral fluid intake to patients initially may be able to reduce the number of hospitalizations. Oral fluids should contain electrolytes and sugar to replace losses from fever and vomiting. Patients who are sent home should be monitored daily by health care providers for temperature pattern, the volume of fluid intake and losses, urine output (volume and frequency), warning signs, signs of plasma leakage and bleeding, haematocrit, and white blood cell and platelet counts. If a patient does not show any clinical improvement and deteriorates around the time of defervescence, should be referred for in-hospital management and follow the action plan. Group B Dengue patients with warning signs: the warning signs include abdominal pain or tenderness, persistent vomiting, clinical fluid accumulation (ascites or pleural effusion), mucosal bleeding, lethargy or restlessness, liver enlargement >2 cm, or when a laboratory parameter includes an increase in hematocrit with concurrent rapid fall in platelet count. Patients need to be admitted to a secondary health care centre for close observation, particularly as they approach the critical phase. These include patients with warning signs, those with co-existing conditions such as pregnancy, infancy, old age, obesity, diabetes mellitus, renal failure and other comorbid conditions. Reassess the clinical status, repeat the haematocrit and review fluid infusion rates accordingly. Sometimes patients receive intravenous fluids elsewhere and present with complications like myocarditis and fluid overload. Fluids containing glucose may exacerbate hyperglycaemia of physiological stress from dengue and in patients with diabetes mellitus. Group C: Severe dengue includes severe plasma leakage leading to dengue shock or fluid accumulation with respiratory distress, severe haemorrhages or severe organ impairment (hepatic damage, renal impairment, cardiomyopathy, encephalopathy or encephalitis). All patients with severe dengue should be admitted to a hospital with access to intensive care facilities and blood transfusion. Judicious intravenous fluid 24 resuscitation is essential and usually, the sole intervention required. Plasma losses should be replaced immediately and rapidly with isotonic crystalloid solution. It is important to monitor haematocrit levels before and after fluid resuscitation. World Health Organization Comprehensive guidelines for prevention and treatment of dengue and dengue hemorrhagic fever. The North Indian dengue out break 2006: a retrospective analysis of intensive care unit admissions in a tertiary care hospital. Dengue haemorrhagic fever: ultrasound as an aid to predict the severity of the disease. It is transmitted to humans by the bite of larval mites (chiggers) of Leptotrombidium deliense. Primary reservoir and vector for the disease is Leptotrombidium deliense, a trombiculid mite. That is why transmission is seasonal, and the peak of scrub typhus occurs during monsoon and continues in to cooler months in India. But in some patients, the disease may be more severe and protracted, and may be fatal. Initial clinical features of scrub typhus patients include fever, headache, myalgia, cough and loose motions. Though eschar was pathognomic of scrub typhus, it was noted in less percentage of patients in Indian studies. Clinicians should suspect scrub typhus in a case of fever and diarrhea if accompanied by symptoms of respiratory or central nervous system in an endemic area. Cardiac conduction abnormalities in the form of bradycardia can be seen on electrocardiogram. Weil felix can be a useful tool when used and interpreted in correct clinical context. In patients in the endemic areas, presenting with fever, respiratory symptoms and hepatitis, scrub typhus should be considered in the differential diagnosis. As delay in treatment may lead to complications and higher mortality, empiric treatment with doxycycline or macrolides may be given in cases where scrub typhus is suspected if facilities for diagnosis are not available. Scrub typhus in patients reporting with acute febrile illness at a tertiary health care institution in Goa. Travel-acquired scrub typhus: emphasis on the differential diagnosis, treatment, and prevention strategies. Early identification of sepsis and septic shock patients and appropriate management in the initial hours has seen a nearly 50% reduction in mortality during the last decade. Septic shock is a subset of sepsis in which particularly profound circulatory, cellular, and metabolic abnormalities are associated with a greater risk of mortality than with sepsis alone. Clinically they are identified by a vasopressor requirement to maintain mean arterial pressure of 65 mmHg and serum lactate level greater than 2 mmol/L (>18mg/dL) in absence of hypovolemia. Sepsis is the primary cause of death from infection, especially if not recognized and treated promptly. It is a simple risk stratification tool that can be used to identify patients at risk of sepsis in outof-hospital, emergency department and general hospital ward settings. Infection-induced organ dysfunction may be occult; therefore, all patients with infection should be carefully evaluated. Conversely, any unexplained acute onset of organ dysfunction should also raise the possibility of an underlying infection. These may include blood, respiratory secretions, urine, cerebrospinal fluid, wounds, and other body fluids. If it is not logistically possible to obtain cultures promptly (45 minutes), the appropriate antimicrobials should be administered. In sepsis or septic shock patients, the diagnosis includes identification of a specific anatomic site of infection requiring emergent source control. Clinical experience with molecular diagnostic methods for the diagnosis of infection is still limited and needs further verification before they can be recommended for use in clinical practice. A bundle is a selected set of elements of care that, when implemented as a group, effects the outcomes beyond implementing the individual elements alone. Lower mortality has been observed in hospitals with higher compliance of sepsis bundle. Circulatory shock is possible with normal arterial blood pressure, and not all patients with arterial hypotension have a circulatory shock. Resuscitation aims to normalize lactate in patients with elevated lactate levels as a marker of tissue hypoperfusion. In absence of a definitive diagnosis at presentation, which is common (in the Golden hour), empiric broad-spectrum therapy should be initiated to cover all likely pathogens (including bacterial, potentially fungal or viral coverage). Selection of an optimal empiric antimicrobial regimen in sepsis and septic shock is one of the central determinants of outcome. Various factors which must be taken into consideration for deciding the choice of empiric antimicrobial therapy are shown in box 2. Box 2: Factors determining the selection of antimicrobials for sepsis and septic shock 1. Age and concomitant underlying diseases, chronic organ failures, medications, indwelling devices 5. Recent infections, intake of antimicrobials within the previous 3 months 31 Sepsis can originate from community locations as well as a healthcare facility. The common sites of infection leading to sepsis include lungs followed by abdomen, bloodstream, renal and genitourinary tracts. Refer to the appropriate sections in this guideline for the empirical antibiotic therapy for a different site of infection. Triazoles are acceptable in hemodynamically stable, less ill patients who have not had previous triazole exposure and are not known to be colonized with azoleresistant species. De-escalation includes discontinuation of combination therapy within the first few days in response to clinical improvement and/or evidence of infection resolution. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). Surviving Sepsis Campaign: international guidelines for management of sepsis and septic shock. Effect of Piperacillin-Tazobactam vs Meropenem on 30-Day Mortality for Patients with E coli or Klebsiella pneumoniae Bloodstream Infection and Ceftriaxone Resistance A Randomized Clinical Trial. Manish Soneja Associate Professor Department of Medicine All India Institute of Medical Sciences. Pneumococcal resistance in non meningeal isolates is very low in our country and hence standard doses of amoxicillin generally suffice. Conversely, pneumococcal resistance to co-trimoxazole and macrolides is widespread. Resistance to amoxicillin by production of beta lactamase in Hemophilus influenzae is around 30% and that in Moraxella is 90%. The term influenza like illness is used when there are systemic signs such as fever and malaise along with the upper respiratory symptoms. The patients should be warned about symptoms which indicate complications like breathing difficulty, persistent fever beyond 4-5 days or ear pain. The positive predictive value of these signs for streptococcal sore throat is around 60%. The first line drug for patients who have not received penicillin in the past one month and those with absence of purulent conjunctivitis is amoxicillin. Coamoxiclav should be used in others and if the patient fails to respond to amoxicillin. The duration of therapy for severe disease and children less than 2 years is 10 days. Children between 2 and 5 years with mild disease can be treated for 7 days and those above 5 years with 5-7 days of therapy. The percentage contribution of viruses reduces as age advances and the relative contribution of mycoplasma increases. Mycobacterium tuberculosis should also be considered a possible etiology in some individuals with a slightly protracted illness. Since penicillin resistance is very low, standard doses of amoxicillin (30-40 mg/ kg/day or 500 mg thrice daily in adults)suffice. Resistance in Hib to ampicillin in a recent study evaluating lower respiratory tract isolates was 10%.
Provera 10 mg discount. Health Benefits of Palm Jaggery | Unave Marundhu | 21/10/2016 | PUTHUYUGAM TV.
The level of renal function below which the dose of a drug must be reduced depends on how toxic it is and whether it is eliminated entirely by renal excretion or is partly metabolized to inactive metabolites pregnancy 10 discount 5mg provera with visa. In general menopause depression treatment cheap 10 mg provera otc, all patients with renal impairment are given a loading dose which is the same as the usual dose for a patient with normal renal function breast cancer oakleys quality provera 10mg. The maintenance dose of a drug can be reduced either by reducing the individual dose leaving the normal interval between doses unchanged or by increasing the interval between doses without changing the dose menstruation occurs in females 10mg provera with amex. The interval extension method may provide the benefits of convenience and decreased cost women's health center rome ga buy provera 5 mg with amex, while the dose reduction method provides a more constant plasma concentration women's health issues in the military cheap 5mg provera with mastercard. The following table lists drugs, in alphabetical order, for which specific information on use in renal impairment (including recommended doses) is available. Many drugs should be used with caution in renal impairment but no specific advice on dose adjustment is available; it is therefore important to also refer to the individual drug entries. The serum creatinine concentration is sometimes used instead as a measure of renal function but it is only a rough guide even when corrected for age, sex and weight by special nomograms. When prescribing for the elderly, assume at least a mild degree of renal impairment. In these patients the complexity of clinical status as well as other variables for example altered absorption, protein binding or metabolism, or liver function, and other drug therapy precludes use of fixed drug dosage and an individualized approach is required. However, the hepatic reserve appears to be large and liver disease has to be severe before important changes in drug metabolism take place. The ability to eliminate a specific drug may or may not correlate with the livers synthetic capacity for substances such as albumin or clotting factors, which tends to decrease as hepatic function declines. Unlike renal disease, where estimates of renal function based on creatinine clearance correlate with parameters of drug elimination such as clearance and half-life, routine liver function tests do not reflect actual liver function but are rather markers of liver cellular damage. In severe liver disease increased sensitivity to the effects of some drugs can further impair cerebral function and may precipitate hepatic encephalopathy (for example, morphine). Oedema and ascites in chronic liver disease may be exacerbated by drugs that cause fluid retention (for example, acetylsalicylic acid, ibuprofen, prednisolone, dexamethasone). However, most hepatotoxic reactions to drugs are rare but tend to be unpredictable. Information to help prescribing in hepatic impairment is included in the following table. However, absence from the table does not automatically imply safety as for many drugs data about safety are absent; it is therefore important to also refer to the individual drug entries. A new denition of dry eye was develschemes for dry eye, as well as the current clinical oped to reect current understanding of the disease, and the and basic science literature that has increased and claried committee recommended a three-part classication system. The second is mechanistic and shows how herein an updated denition of dry eye and classications each cause of dry eye may act through a common pathway. It is stressed that any form of dry eye can interact with and exacerbate other forms of dry eye, as part of a vicious circle. These guidelines are not intended to override the Subcommittee were to develop a contemporary denition of clinical assessment and judgment of an expert clinician in dry eye disease and to develop a three-part classication of individual cases, but they should prove helpful in the conduct dry eye, based on etiology, mechanisms, and disease stage. The manner of working of the committee is outlined in the introduction to this issue of the O cular S urface. Initially two denitions were developed and presented to members Proprietary interests of Subcommittee members are disclosed on pages 202 and 204. The d enition and classication of d ry eye potential damage to the ocular surface. It is accompad isease: report of the Denition and Classication Sub committee of 11-14 nied by increased osmolarity of the tear lm and the International Dry Eye W orkShop (2007). Classication of dry eye disease as specialized invaginations from the ocular surface. Etiopathogenic classication of dry eye disease broader concept, which has additional features, has been 1. Aqueous tear-decient dry eye termed the Ocular Surface System and is discussed further in the Research chapter of this issue. Non-Sjogren syndrome dry eye An important aspect of the unit is the part played by 1) Primary lacrimal gland deciencies sensory impulses, which arise from the ocular surface, in the maintenance of resting tear ow. Currently, it is considered 2) Secondary lacrimal gland deciencies that waking tear ow is a reex response to afferent im3) Obstruction of the lacrimal gland ducts pulses deriving particularly, but not entirely, from the ocular 4) Reex hyposecretion 22 surface. Sensory input from the nasal mucosa also makes a) Reex sensory block 23 a contribution. Evaporative dry eye and motor nerves, and the tear-secreting glands) can destaa. Intrinsic causes bilize the tear lm and lead to ocular surface disease that 1) Meibomian gland dysfunction expresses itself as dry eye. Tear lm stability, a hallmark of 2) Disorders of lid aperature and lid/globe the normal eye, is threatened when the interactions between congruity or dynamics stabilizing tear lm constituents are compromised by de3) Low blink rate creased tear secretion, delayed clearance, and altered tear b. Ocular surface inammation is a secondary 1) Ocular surface disorders consequence. Reex tear secretion in response to ocular 2) Contact lens wear irritation is envisioned as the initial compensatory mecha3) Ocular surface disease nism, but, with time, inammation accompanying chronic secretory dysfunction and a decrease in corneal sensation 4) Allergic conjunctivitis eventually compromises the reex response and results in C. Tear hyperosmolarity is considered to play an important role in the evolution of 2. The basis for symptoms in dry eye the distinctions aq ueous-decient dry eye and evaporative E. Classication of dry eye based on severity dry eye were removed from the denition, but are retained in the etiopathogenic classication. Here, scheme can provide a guide, but an expert clinician, applypostganglionic bers arise, which terminate in the lacrimal ing appropriate diagnostic criteria, is needed to establish gland, nasopharynx, and vessels of the orbit. Recently, two new classication this functional unit controls the major components schemes were published, and these were used as source of the tear lm in a regulated fashion and responds to documents by the committee. These include: the Triple environmental, endocrinological, and cortical inuences. The left hand box illustrates the inuence of environment on the risk of an individual to develop dry eye. The term environment is used broadly, to include bodily states habitually experienced by an individual, whether it reects their milieu interieur or is the result of exposure to external conditions which represent the milieu exterieur. Aqueous-decient dry eye has two major groupings, Sjogren syndrome dry eye and non-Sjogren syndrome dry eye. Evaporative dry eye may be intrinsic, where the regulation of evaporative loss from the tear lm is directly affected, eg, by meibomian lipid deciency, poor lid congruity and lid dynamics, low blink rate, and the effects of drug action, such as that of systemic retinoids. Extrinsic evaporative dry eye embraces those etiologies that increase evaporation by their pathological effects on the ocular surface. Causes include vitamin A deciency, the action of toxic topical agents such as preservatives, contact lens wear and a range of ocular surface diseases, including allergic eye disease. The committee also rejected schemes: one based on etiopathogenesis; one based on the a subdivision based on the presence or absence of lid disglands and tissues targeted in dry eye; and one based on ease, because it is frequently difficult to identify the relative disease severity. The committee felt that the concept of three different the majority of the Denition and Classication Subschemes serving different purposes was attractive, but it committee was in favor of adopting a severity grading based was noted that evidence-based referencing was limited. The Delphi Panel was a consensus group that met to review the classication of dry eye. Etiopathogenic Classication of Dry Eye Disease changing the name of dry eye disease to dysfunctional tear synthe etiopathogenic classication developed by the drome, suggesting that the name more accurately reected Subcommittee is an updated version of that presented in pathophysiological events in dry eye. The classication has the following features: Occupational factors may cause a slow blink rate, reprethe left hand box in Figure 1 illustrates the inuence of senting a risk for dry eye in those working with video disenvironment on an individuals risk of developing dry eye. For instance, a normal subject may have a low chiey to a failure of lacrimal secretion, and this approach is natural blink rate, or the blink rate may be slowed for beretained. However, it should be recognized that a failure of havioral or psychological reasons. It is recognized that disease initiing palpebral width and is, therefore, increased in upgaze. Biologically active, androgens promote lacrimal of dry eye cause goblet cell loss and that this, in turn, will and meibomian gland function. Tear Lacrimal tear secretion is reduced by a number of lm hyperosmolarity causes hyperosmolarity of the ocular systemic drugs, and these effects may be looked upon as surface epithelial cells and stimulates a cascade of inamdisturbances of the milieu interieur. Evaporative water loss detected in the tears, it is not usually possible to know from the eye is increased in conditions of low relative whether they derive from the lacrimal gland itself or from humidity, occurring either as part of natural variation at the ocular surface (conjunctiva and cornea). Revised international classication criteria for ocular manifestations of Sjogren syndrome muscarinic receptors within the glands. Ocular symptoms: a positive response to at least one of the following questions: There are two forms 1. Oral symptoms: a positive response to at least one of the following questions: American collaboration. Ocular signs: that is, objective evidence of ocular involvement dened as a positive result toms of dry mouth, in the for at least one of the following two tests: presence of autoantibod1. Schirmer I test, performed without anesthesia (b5 mm in 5 minutes) ies, evidence of reduced 2. Histopathology: In minor salivary glands (obtained through normal-appearing mucosa) focal minor salivary gland bilymphocytic sialoadenitis, evaluated by an expert histopathologist, with a focus score r1, opsy. Salivary gland involvement: objective evidence of salivary gland involvement dened by a 1. Parotid sialography showing the presence of diffuse sialectasias (punctate, cavitary or of an overt autoimmune destructive pattern), without evidence of obstruction in the major ducts19 connective disease, such as 3. Autoantibodies: presence in the serum of the following autoantibodies: systemic lupus erythema1. Classication criteria for Sjogrens syndrome: a revised version of the European criteria proposed by the American-European Consensus Group. Delayed or absent tissues), and exposure to environmental agents, ranging spreading of the tear lm could lead to an increase in water from viral infections affecting the lacrimal gland to polluted loss from the eye. Sjogren Syndrome Dr y Eye to increased evaporative water loss from the eye (eg, low Sjogren syndrome is an exocrinopathy in which the humidity, high wind velocity, and increased exposure of the lacrimal and salivary glands are targeted by an autoimmune ocular surface) may act as a trigger by invoking inammaprocess; other organs are also affected. The lacrimal and tory events at the ocular surface through a hyperosmolar salivary glands are inltrated by activated T-cells, which mechanism (see Section V). Conditions associated with non-Sjogren than in the normal population; thus, a defective tear lm syndrome dry eye lipid layer may contribute to dry eye by leading to excess evaporation. Reex sensory block With increasing age in the normal human population, Contact lens wear there is an increase in ductal pathology that could promote Diabetes lacrimal gland dysfunction by its obstructive effect. They postulated a sequence of periductal brosis, interacinar brosis and, nally, acinar atrophy. There is a developmental and progressive neuronal 6 months after hematopoietic stem cell transplantation. A reduction in sensory drive from the ocular Obstruction of the ducts of the main palpebral and acsurface is thought to favor the occurrence of dry eye in two cessory lacrimal glands leads to aqueous-decient dry eye ways, rst, by decreasing reex-induced lacrimal secreand may be caused by any form of cicatrising conjunctivitis tion, and, second, by reducing the blink rate and, hence, (Table 2). Specic conditions Bilateral sensory loss reduces both tear secretion and are discussed below. Bilateral, topical proparacaine decreases the Trachoma: Trachoma is a cause of blindness on a global blink rate by about 30% and tear secretion by 60-75%. Dry eye is part of terminals supplying the palpebral and accessory lacrimal the overall picture, resulting from lacrimal duct obstruction, glands (Belmonte C: personal communication). Conjunctival scarring can lead to dry eye in ments have been put forward to suggest that at least some the manner outlined above. Goeb124 Replacement Dystichiasis Bron et al137 bels found a reduction in reex tearing (Schirmer Dystichiasis lymphedema syndrome Brooks et al138 Kiederman et al139 test) in insulin-dependent diabetics, but no differMetaplasia ence in tear lm breakup Meibomian Gland Dysfunction time or basal tear ow by 140 Hypersecretory Meibomian seborrhoea Gifford uorophotometry. In addition, it is tions were reported by Schein et al, unrelated to the disease envisaged that there is a loss of trophic support to the ocular for which they were used. Evaporative Dry Eye nervus intermedius, leads to dry eye due to loss of lacrimal Evaporative dry eye is due to excessive water loss from secretomotor function. The nervus intermedius carries the exposed ocular surface in the presence of normal lacpostganglionic, parasympathetic nerve bers (of pterygorimal secretory function. Its causes have been described as palatine ganglion origin) to the lacrimal gland. Dry eye is intrinsic, where they are due to intrinsic disease affecting lid due to lacrimal hyposecretion in addition to incomplete lid structures or dynamics, or extrinsic, where ocular surface closure (lagophthalmos). An association between systemic drug use and dry eye has been noted in several studies, with decreased lacrimal a. Endocrine exophthalmos ple causes and associations are listed in Table 4 and include and, specically, increased palpebral ssure width, is asdermatoses, such as acne rosacea, seborrhoeic dermatitis, sociated with ocular drying and tear hyperosmolarity. Less common but important associaIncreasing palpebral ssure width correlates with increased tions include the treatment of acne vulgaris with isotretintear lm evaporation. Diagnosis is based ocular surface is exposed to water loss before the next on morphologic features of the gland acini and duct orices, blink. In the latter group, esterases tear meniscus height, and meibomian gland function. They also suggest that a reduced blink rate could impair the clear2) Disorders of Lid Aperture and Lid/Globe ance of lipid-contaminated mucin. This, together with poor lens wettability, could deciency and the effects of chronically applied topical be a basis for a higher evaporative loss during lens wear and anesthetics and preservatives. Patients wearing high water-content hydrogel lenses were Vitamin A is essential for the development of goblet cells more likely to report dry eye. This is a controversial area in in mucous membranes and the expression of glycocalyx the literature.