Larry T. Khoo, MD
- Director of Neurological and Spine Surgery
- The Spine Clinic of Los Angeles
- Los Angeles, California
In clients with severe hypertension or in those whose blood pressure is poorly controlled medications varicose veins purchase seroquel australia, heavy physical activity should be discouraged or postponed until appropriate drug therapy has been instituted and found to be effective (Williams et al medicine evolution order seroquel australia. Written exercise advice was shown to be more effective than verbal advice alone in encouraging clients to adopt and sustain increased levels of physical activity over a six week period xerostomia medications side effects discount 300 mg seroquel visa. The two most common reasons for being inactive are not enough time and not enough energy treatment jammed finger generic seroquel 300mg with mastercard. It has been suggested that any activity appears to be helpful treatment 9mm kidney stones cheap 300mg seroquel, but those who are more active appear to gain more benefit medicines 604 billion memory miracle cheap seroquel 100mg line. A client can benefit just as much from three ten minute spurts of moderate activity as from a solid half-hour. Discussion of Evidence According to the Canadian Medical Association Hypertension Guidelines (1999) 75% of Canadians over the age of 15 consume alcohol, and 6. The evidence shows that excessive alcohol consumption raises blood pressure independent of other risk factors including smoking, age, sex, race, coffee use, level of education, prior heavy drinking history and the type of alcohol consumed (Boggan, 2003; Oparil & Weber, 2000). Attempting to define an absolute cause and effect relationship between alcohol and hypertension is complicated, as other factors come into play. Some of these factors include amount of alcohol ingested, chronic or binge drinking, underlying state of health and effects of alcohol on the myocardium. A study done by De la Sierra (1996, as cited in Estruch, 2003) indicates some people are sensitive to the pressor effects of alcohol. One group of individuals had a mean rise in blood pressure of at least 3 mmHg compared to another group of resistant individuals who had no rise in their blood pressure when ingesting alcohol in the same controlled circumstances. Some of these theories are listed below: increased intracellular calcium or other electrolytes in vascular smooth muscle (Boggan 2003; Estruch, 2003; Lip & Beevers, 1995; Oparil & Weber, 2000) inhibition of vascular relaxing substances. This tool is a series of four questions meant to assess for alcohol dependence in a non-threatening manner. The questions should be part of an overall health assessment and asked at every visit regarding recent alcohol consumption. A positive response to any one of the four questions would indicate to the healthcare professional that there is a suspicion of over consumption. This tool places the emphasis on heavy drinking and frequency of intoxication rather than signs of dependency. In its initial pilot in six different countries, the sensitivity averaged 80% and specificity averaged 98% for detecting excessive alcohol consumption (Haggerty,1994). If alcohol overuse is suspected or identified, the client should be counseled on the negative health effects and referral to an alcohol treatment specialist or program may be appropriate (Cushman, 2001). This list of tools is not all-inclusive, and some of the tools are designed for use with specialized populations or as part of a broader substance use evaluation. Research has shown that approximately half of clients with excessive alcohol use have blood pressure readings >160/90, and these values were found to normalize during abstinence. Similar trends were found within a broader population base leading researchers to believe the blood pressure effects of alcohol are due to alcohol consumed in the days immediately prior to measurement and the effect is rapidly reversible (Seppa & Sillanaukee, 1999). Furthermore, binge drinking was found to be a risk factor for stroke in young persons who consumed alcohol on weekends and holidays, prime drinking times. Although there is no direct evidence, this study would suggest a link between alcohol, hypertension and stroke (Seppa & Sillanaukee, 1999). Multiple population cohort and cross-sectional trials have shown little difference in blood pressure in clients with low alcohol consumption and abstainers. There is also evidence to support the limited consumption of alcohol for its cardio protective effects. Nurses need to be aware of this evidence and should not discourage consumption within the recommended guidelines nor should they encourage the initiation of drinking as a method of risk factor reduction related to the associated potential health risks of overuse (Williams et al. Adoption of healthy lifestyle behaviours is an important factor in prevention of high blood pressure and lowering blood pressure in those known to be hypertensive. This resistance may be a result of poor adherence to the medication regime and/or a change in pharmakinetics of the antihypertensive agent metabolized by the liver that is under the influence of acute or chronic alcohol ingestion (Lip & Beevers, 1995). In conclusion, limiting the consumption of alcohol, to within recommended guidelines, has shown a modest reduction in hypertension. Smoking and hypertension are both independent risk factors which accelerate atherosclerosis and blood vessel injury, increasing the risk of vascular disease and subsequent end organ damage (heart, brain, kidney, eye or limbs). Atherosclerosis is a complex, diffuse and progressive process with a variable distribution and clinical presentation. Risk factors play an important role in initiating and accelerating the process (Faxon et al. Extensive observational data has shown that smoking has a graded adverse effect on cardiovascular health and increases cardiovascular 50 Nursing Best Practice Guideline disease risk more than mild hypertension (Williams et al. Smoking exacerbates uncontrolled hypertension, atherosclerosis, and blood vessel injury (Lamb & Bradford, 2002). Since blood pressure readings are usually taken when the client is not smoking, blood pressure is systematically underestimated among those who smoke regularly. Data suggests that smoking may interfere with the beneficial effects of some antihypertensive agents, such as blockers or may prevent the benefits of more intensive blood pressure lowering (European Society of Hypertension, 2003). There is a rapid decline in cardiovascular risk, by as much as 50% after 1 year, for those who stop smoking. Up to 10 years may be needed to reach the risk level of those who never smoked (Williams et al. Individuals need to recognize their increased risk due to smoking and the benefits of cessation. Despite significant declines in smoking in the past three decades, trends to stop smoking have slowed, and recently, smoking has increased among young minorities. This emphasizes that tobacco use should be assessed at every visit (Keevil, Stein & McBride, 2002). A Cochrane systematic review has confirmed the effectiveness of physicians advice to stop smoking (Rice & Stead, 2005). Physician advice and encouragement given repeatedly over time has shown to reduce smoking by 21% (Williams et al. Although there is less support for advice given by non-physician clinicians, the overall recommendation suggests that all clinicians provide interventions (Rice & Stead, 2005). This review notes the potential benefits of smoking cessation advice and/or counseling given by nurses to clients, with reasonable evidence that intervention can be effective. Nurses are the largest healthcare workforce, and are involved in virtually all levels of healthcare. Similar advice and encouragement given by nurses at health checks or prevention activities may be less effective, but may still have some impact. It recognizes that nurses have advocacy opportunities both in their individual practices and as a strong united voice. Nurses are encouraged to integrate tobacco use assessment, counseling and interventions into their practices and to lead in conducting research. Public Health Service-sponsored Clinical Practice Guideline: Treating Tobacco Use and Dependence (Fiore, 2000) recommends that medical offices include tobacco use as a vital sign. Highest screening and counseling rates are found when tobacco use is included with the vital signs for each client (Keevil et al. The probability of successful smoking cessation increases with each attempt and there is a 10-fold increase in success rates among those counseled during a clinical visit. Follow up and the number of contacts between the client and provider are also significant predictors of clinical success (Keevil et al, 2002). Nurses are involved in the majority of these visits and could therefore have a profound effect on the reduction of tobacco use (Whyte, 2003 as cited in Rice & Stead, 2005). Individuals who use tobacco can benefit from several types of interventions (Fiore et al, 2000). The Medical and Allied Healthcare Professionals: Basic Tobacco Intervention Skills Guidebook (Arizona Department of Health Services, 2005) states that Brief tobacco interventions delivered by multiple persons (including both medical and non-medical persons) are more effective in helping people quit using tobacco than minimal interventions (such as free literature) alone, 25. Public Health Service, is an integrated stage-based brief smoking cessation intervention. Practicing nurses should be encouraged to inquire about the availability of additional training on smoking cessation in their community. The lower amounts of nicotine contained in smoking cessation aids does not usually raise blood pressure, therefore, these aids may be used with appropriate counseling and behaviour interventions (Khoury et al. Nicotine replacement therapy is not an independent risk factor for acute myocardial events. The evidence on the impact of a smoke-free policy on smoking cessation rates is not yet available. However, some insight can be gleaned from the review of the literature on the effects of smoke-free workplaces, which reveals that these policies not only protect non-smokers from the dangers of passive smoking, but also encourage those who smoke to quit or to smoke 3. Arrange Follow-up after Quit Date 54 Nursing Best Practice Guideline Stress Recommendation 2. Outside pressures or demands, especially those in which we perceive a loss of control, can make us feel tense. Stress related to depression, social isolation, and lack of quality support increases the risk of coronary artery disease similar to conventional risk factors such as smoking, dyslipidemia and hypertension, but it remains unclear what the role of effective stress management is when optimizing blood pressure control (Bunker et al. Stressful situations range from major life altering events to multiple small situations that build up over time. Awareness of what causes stress, acceptance that life is not perfect and coping by learning strategies to effectively handle stress can reduce the risk of stress related conditions and enhance overall general health. It will take patience to understand, acknowledge and accept those problems that have been a part of their lives for a long time. Have the client write down how they respond/react when their buttons are pushed. Facilitate client to think critically and adopt strategies to accept the situation. Remember that we are all different, and that coping strategies should be individualized. However, nurses are in the best position to provide education about antihypertensive medications and monitor their therapeutic effectiveness (Bengtson & Drevenhorn, 2003). Studies have found that nursing interventions, including blood pressure checks, lifestyle and medication advice and monitoring, either on home visits or at the community clinics, were effective in reducing blood pressure in hypertensive clients (Garcia-Pena et al. Hence, nurses must be knowledgeable about the classes of medications that may be prescribed for clients diagnosed with hypertension. Nurses should educate clients that combination therapy may be necessary to manage their hypertension. Refer to Appendix O for a summary of medications commonly prescribed for hypertension. Refer to Appendix O for suggested resources regarding global vascular protection risk and treatment recommendations for clients with high risk health conditions. Some clients who take over-the-counter medications, vitamin/nutritional supplements or elect to augment their pharmacological treatment of blood pressure with herbal remedies (Miller & Kazal, 1998) may be unaware that any of these preparations may have potential interactions with the antihypertensive medications or may cause elevated blood pressure. All clients should be asked whether they use any natural/over the-counter/supplements products and should be advised that natural does not necessarily equal safe (UpToDate, 2005). To date, the effectiveness and safety of herbal preparations has not been studied in the same rigorous manner as conventional treatment, hence, evidence-based guidelines for the use of alternative treatments are not currently available. Some herbal remedies have been known to potentiate the antihypertensive effects of the drugs. It is important that nurses, in collaboration with pharmacists and physicians, educate clients about antihypertensive medications, including potential interactions with herbals/supplements/ over-the-counter preparations and to either avoid these remedies or take them with caution. Substance abuse and hypertension are an important health concern, especially in adolescent and young adults presenting with elevated blood pressure and associated cardiovascular conditions (Ferdinand, 2000). Nurses, in collaboration with pharmacists and physicians, should question clients about drug use and educate them about the risks and the potential interactions with antihypertensive medications. All five dimensions should be considered in a systematic exploration of adherence and the interventions aimed at improving it. Social and economic factors the main economic and social concerns that should be addressed in relation to adherence are poverty, access to healthcare and medicines, literacy, provision of effective social support networks and mechanisms for the delivery of health services that are sensitive to cultural beliefs about illness and treatment. Universal and sustainable financing, affordable prices and reliable supply systems are required if good rates of adherence to therapies are to be achieved. Community-based organizations, education of illiterate clients, assessment of social needs and family preparedness have been reported to be effective social interventions for improving adherence. Social support has been consistently reported as an important factor affecting health outcomes and behaviours. There is 59 Nursing Management of Hypertension substantial evidence that peer support among clients can improve adherence to therapy while reducing the amount of time devoted by health professionals to the care of clients with chronic conditions. Community interventions have also been shown to result in economic and health benefits by improving clients self management capacities by promoting the maintenance and motivation required for self-management, as well as keeping the client active in the knowledge of his or her disease and in the acquisition of new habits. Healthcare team and system-related factors Healthcare system variables include the availability and accessibility of services, support for education of clients, data collection and information management, provision of feedback to client and healthcare providers, community supports available to clients, and the training provided to health service providers. Relatively little research has been conducted on the effects of the healthcare team and other system related factors on clients adherence. Lack of clinical tools to assist health professionals in evaluating and intervening in adherence problems; 3. Condition-related factors Condition-related factors represent particular illness-related demands faced by the client.
Some disadvantages include less tensile strength compared to sutures symptoms 9f anxiety buy cheap seroquel 200mg line, and increased wound dehiscence over joints and high-tension areas medicine 2355 generic seroquel 100 mg with visa. Tissue adhesives are seemingly simple medicine x pop up discount 50mg seroquel visa, but they should be used by experienced personnel since they have many adverse effects described which are preventable if used in the correct manner medications post mi discount seroquel 300 mg on-line, and if their use is avoided in wound conditions which are unsuitable for tissue adhesives symptoms 1dp5dt purchase seroquel paypal. What is the purpose of using epinephrine in local infiltration and topical anesthesia What has the best cosmetic result in the repair of lacerations: sutures or tissue adhesives What is the major clinical reason for preferring healing by secondary or tertiary intention (as opposed to primary closure) True/False: Antibiotics have only a modest effect on reducing the rate of wound infections in contaminated wounds medicine naproxen 500mg order genuine seroquel. Comparison of plain, warmed, and buffered lidocaine for anesthesia of traumatic wounds. Since epinephrine is a vasoconstrictor, it slows the rate of local anesthetic release into the general circulation permitting a higher total dose of local anesthetic that can be given (useful if the wound is large), it extends the duration of action, and decreases bleeding. The research done on the comparisons between sutures and tissue adhesives have shown that they have comparable cosmetic results. Cocaine component: arrhythmia, urticaria, drowsiness, excitation, seizure, vomiting, flushing, and death. Significantly contaminated wounds, are at greater risk of infection if closed by primary intention. On review of birth records, a moderate-sized scrotal mass had been appreciated on newborn examination with no other abnormalities noted. According to his parents, the bulge has not changed in size since birth and there has been no noticeable discomfort. His parents are reassured and counseled on the possibility of a communicating hydrocele/complete inguinal hernia and to proceed to an emergency room if signs or symptoms of incarceration and strangulation occur. On subsequent well child visits, the right scrotal mass is noted to minimally decrease in size. His parents continue to report no fluctuation in size during activity, crying or defecation. At his 12 month well child visit, the right scrotal mass is noted to be unchanged since his last visit 3 months prior. The estimated incidence of inguinal hernias in children is 5-50/1,000 live births. It is seen more frequently in males than females with a ratio of about 5:1 with a definite familial tendency. About 50% of cases present before 12 months of age with most occurring in the first 6 months of life. Approximately 99% of all inguinal hernias in children are indirect inguinal hernias. Most inguinal hernias are unilateral with about 60% occurring on the right side and 30% on the left side. Of note, inguinal hernias are more common in premature infants with an incidence of 5-30%. Most cases are bilateral, occurring in about 62% of affected premature infants (2-5). Normally, in the male fetus, the testes descend to the vicinity of the internal ring of the inguinal canal by approximately 28 weeks gestational age. With testicular descent, the lining of the peritoneal cavity extends into the inguinal canal and scrotum. Each testis descends through the inguinal canal external to the processus vaginalis. In the female fetus, a similar mechanism with descent of the ovaries into the pelvis occurs. The processus vaginalis in females extends through the inguinal canal into the labia majoris and is referred to as the canal of Nuck (2). In males, a hydrocele is formed when there is patency of the processus vaginalis between the scrotum and the peritoneal cavity resulting in an accumulation of fluid between the layers of the tunica vaginalis surrounding the testis. In the weeks prior to birth or shortly after, the processus vaginalis closes spontaneously in the area of the internal ring, obliterating the entrance to the inguinal canal. The scrotal fluid collection that remains within the tunica vaginalis is referred to as a scrotal hydrocele, or a non communicating hydrocele. If the processus vaginalis fuses proximally and distally but remains open in between, the isolated fluid collection is referred to as a hydrocele of the cord. This type of hydrocele, although not in communication with the peritoneal cavity or the scrotum, is often associated with a hernia and/or a scrotal hydrocele (6). In some older boys, a scrotal hydrocele may result from inflammation within the scrotum caused by various conditions including testicular torsion, torsion of the appendages, epididymitis, and testicular cancer (1,4). When the processus vaginalis fuses distally but remains patent proximally, abdominal contents can enter the inguinal canal resulting in an inguinal hernia. However, if the processus vaginalis fails to fuse completely, there will be communication between the scrotum and the peritoneal cavity through the patent processus vaginalis resulting in an inguinal-scrotal hydrocele, or communicating hydrocele. Of note, there is a rare but important type of communicating hydrocele called an abdominal-scrotal hydrocele. With this type of hydrocele, the communication is between the scrotum and a cystic loculation of fluid within the lower abdomen. This may result in recurrent communicating hydroceles or unusually large hydroceles. If a communicating hydrocele is large enough, abdominal contents may extend through the patent processus vaginalis to the scrotum resulting in an inguinal-scrotal hernia (complete inguinal hernia). The hernia sac in males and females may contain intestine or omentum, with the ileum being the most common intestinal component. Of note, it is possible for a testis to be found in the hernia sac of a female infant if testicular feminization (complete androgen insensitivity) is present. More than half of patients with testicular feminization have an inguinal hernia (4). In differentiating a hydrocele from a hernia, history and physical examination can be diagnostic. The most important information elicited from parents is a history of fluctuation in the volume of the mass that would be consistent with a hernia or communicating hydrocele. Parents may report an increase in size that is particularly noticeable at times of increased intra-abdominal pressure (activity, crying or straining). Parents may also report previous reduction of the mass by either themselves or another physician. A history of fussiness, obvious discomfort, poor feeding, vomiting, and abdominal distention would suggest incarceration. This usually results in crying, thereby causing an increase in intra-abdominal pressure. The mass is palpated and evaluated for tenderness, tenseness, and associated skin discoloration that, if present, would suggest incarceration and possible strangulation. If the mass is non-tender, smooth, firm and located in the scrotum, a hydrocele is likely to be present. A scrotal hydrocele should be moved away from the inguinal canal and palpation of normal cord structures superiorly should be performed to exclude the presence of a hernia. If a patient presents with a large hydrocele or a history of recurrent communicating hydroceles with or without a palpable ipsilateral lower abdominal mass, an abdominal-scrotal hydrocele should be suspected. If compression of the fluid-filled mass completely reduces the size of the hydrocele, a communicating hydrocele or hernia is the likely diagnosis. An inguinal hernia is non-tender, soft, reducible and can be located in the inguinal canal or may extend into the scrotum (inguinal-scrotal hernia). Of note, retractile testes, a common finding in infants and young children, can resemble an inguinal hernia. To avoid misdiagnosis, palpation of the testes should be done prior to palpation of an inguinal mass. An increase in size of the mass would be consistent with a hernia or communicating hydrocele. However, in children, inguinal-scrotal hernias and incarcerated bowel may also brilliantly transilluminate. The internal ring of the uninvolved side should be examined before proceeding to the internal ring of the affected side. If an inguinal hernia is present, abdominal contents may be palpated extending through the internal ring (2,3,6). If there is a history suspicious for a hernia but no mass can be demonstrated on examination, it may be helpful to empty the bladder which, when full, can block the internal inguinal ring and mask an inguinal hernia. Otherwise, a classic history of intermittent inguinal, scrotal or labial swelling that spontaneously reduces may be all that is necessary for diagnosis. However, another physical examination finding that can be present with inguinal hernias is a thickened spermatic cord with an associated "silk" sign. The spermatic cord is palpated over the pubic tubercle and a "silky sensation" is appreciated when the two layers of peritoneum are rubbed together. This finding, along with a history of a hernia, is highly suggestive of an inguinal hernia (2). A scrotal hydrocele that is sufficiently large and tense may cause ischemic injury to the testis. A communicating hydrocele may enlarge and lead to development of an inguinal-scrotal hernia (6). Nine to twenty percent of inguinal hernias in children become incarcerated with more than half of those cases occurring in children less than 12 months of age. The incidence of incarceration increases in premature infants and in term female infants (2,5). Strangulation of the hernia can occur and ischemic injury to intestine and testis/ovary may result (3,6). Intestinal obstruction, intestinal gangrene, and gonadal infarction occur more commonly in the first 6 months of life (4). Thus, because the risk of incarceration is high, particularly in infants, with a risk of strangulation, prompt surgical intervention is recommended as soon as the diagnosis is made. The differential diagnosis of inguinal-scrotal swelling in children (6,7) can be classified based on acuteness of presentation, tenderness, location (intratesticular versus extratesticular), and transillumination. They are extratesticular, but scrotal hydroceles may be difficult to distinguish from an enlarged testicle on palpation. Communicating hydroceles are compressible (that is, they decrease in size with pressure), while non-communicating hydroceles will not change in size. Non-communicating hydroceles are frequently mistaken for incarcerated hernias, because they do not change in size with compression (seemingly non-reducible). However, scrotal hydroceles are spherical or oval in shape, while an incarcerated inguinal hernia is usually tubular in shape (often shaped like a small banana with a slightly tapered point at the end). Additionally, hydroceles are usually softer in consistency, while incarcerated hernias are the consistency of a refrigerated hot dog and sometimes harder than this. Other diagnoses in the differential include lymph nodes, undescended or retracted testis (smaller in size), varicocele (soft spaghetti or bag of worms consistency), and spermatocele. Other considerations include epididymal cyst, testicular cancer, peritesticular rhabdomyosarcoma, benign soft tissue tumors, meconium sequestration, testicular torsion (tender), torsion of appendages, epididymitis, trauma, idiopathic scrotal edema, and Henoch-Schonlein purpura. If there is uncertainty in the diagnosis, an ultrasound examination may aid in differentiating a hydrocele from a hernia, may confirm the presence of an abdominal-scrotal hydrocele, or may rule out other causes of inguinal-scrotal swelling. In a female, ultrasound examination can be used as part of the evaluation for testicular feminization (4). It can also be used to examine both ovaries when an incarcerated ovary is suspected (6). Abdominal x-rays are unnecessary for diagnosis of an incarcerated hernia, although they may be helpful in confirming an intestinal obstruction. If an incarcerated or strangulated hernia is associated with bowel obstruction or shock, laboratory studies and vascular access are indicated (5). Treatment is usually not required for uncomplicated, simple hydroceles (non-communicating) because they tend to decrease in size with complete resolution in the first 2 years of life. Significant hydroceles persisting beyond 12-24 months are likely to be communicating and are generally surgically corrected at that time (1). However, early surgical repair is recommended for large, tense hydroceles because they rarely disappear spontaneously, they can cause ischemic injury to the testis, and they may be difficult to distinguish from hernias. Communicating hydroceles also require early surgical repair due to the fact that they may progress to symptomatic inguinal-scrotal hernias (6). In fact, inguinal hernia repair is the most common surgical procedure in children (4). In an outpatient setting, if a child presents with an inguinal hernia but is otherwise well (no obstruction or shock), manual reduction should be attempted. About 95% of inguinal hernias can be reduced by applying gentle but steady upward pressure on the hernia sac. If the hernia is easily reducible, referral to a pediatric surgeon should be done for elective surgical repair. While awaiting repair, parents should be counseled to seek immediate evaluation and treatment in an emergency department if signs and symptoms of incarceration and strangulation occur. Inguinal hernias that cannot be easily reduced are incarcerated and require immediate referral to an emergency department. Once the child is sedated, firm steady upward pressure can be applied to the hernia sac using one hand while the other hand gently guides the neck of the hernia sac into the distal ring of the inguinal canal. If reduction is successful, a pediatric surgeon should be consulted for outpatient follow-up. However, children with difficult to reduce hernias or a history of incarceration in the past are at high risk for future incarceration and strangulation and should be managed more urgently. If reduction is unsuccessful, then a pediatric surgeon must be consulted immediately.
Buy cheap seroquel 300 mg on-line. About me living with HNPP and HIV.
Sometimes not until the end of the second week medications 142 buy 100 mg seroquel, and they are marked by fever medications you cant crush cheap seroquel, a chill in some cases and pain and swelling and tenderness along the muscles involved medicine 0552 order line seroquel. The migration of the parasites into the muscles excites a more or less intense inflammation of these muscles symptoms mold exposure generic 50mg seroquel with visa, which is characterized by pain on pressure and movement medicine for sore throat cheap 50 mg seroquel otc, and by swelling and tension of the muscles symptoms non hodgkins lymphoma purchase seroquel overnight, over which the skin may be swollen. Difficulty in chewing and swallowing is caused by the involvement of the muscles controlling these acts. In severe cases the involvement of the diaphragm and intercostal muscles may lead to difficult breathing (Dyspnoea) which sometimes proves fatal. Watery swelling, a feature of great importance, may be seen early in the face, particularly about the, eyes. Later it develops in the extremities when the swelling and stiffness of the muscles are at their height. Profuse sweats, tingling and itching of the skin and in some instances hives (Urticaria) have been described. In the severe cases the appearance may be like that in the third week of typhoid fever. In mild cases the fever and muscular symptoms subside in ten to fourteen days, in others only after two or three months. The mortality, from one to thirty per cent, seems to depend upon the virulence and number of parasites. Beginning with the outer one and naming inward, they are named as follows: the outer layer is called the epidermis or cuticle (near or upon the skin). The third layer is called the sub-cutaneous (under the skin) (fatty or connective) tissue. A round flat, white or pink elevation of the skin; such as hives, mosquito bites, etc. This is a pin-head or pea-sized elevation of the outer layer (epidermis) filled with a watery fluid. A circumscribed elevation of the skin and contains a watery fluid, such as a burn, etc. A rounded elevation of the outer layer (epidermis) of varying size, containing pus (matter). This is a dry attached or unattached thin piece from the skin as a result of disease of the skin. It forms these pimples or pustules and these are intermingled with black-heads (comedones), flesh-worms. They vary from a pin-head to a split-pea in size, and are of a bright or dark red color. The active cause may be the stomach troubles, constipation, womb disorders, and poor general nutrition. When there is dyspepsia and constipation, bitter tonics, like compound tincture of gentian, one dram before meals, or pepsin (five grains) and loosening medicines like salts should be given. Tincture of Nux Vomica is a good stomach and bowel tonic given in doses of one to two drops before meals. Calomel, one-half grain at night for a few nights, followed in the morning by epsom salts or some mineral water like Abilena or Hunjadi is useful. Schalek: Tincture of Nux Vomica 2 drams Dilute Nitro Muriatic Acid 4 drams Sherry Wine enough for 3 ounces Mix and take one teaspoonful three times a day. First wash the parts with warm water and the best soap, rinse with hot water and then dry carefully. Remove the black heads by careful pressure of the fingers, or with black-head extractor; the pimples and pustules should be freely cut, to allow the matter to escape and all the matter taken out. If the skin becomes rough and chapped, soap should not be used in washing, and a soothing ointment should be applied. The following used as a soothing lotion: Washed Sulphur 2-1/2 drams Spirits of Camphor 3 drams Biborate of Sodium 2 drams Glycerin 6 drams Distilled water enough for 4 ounces Mix and shake well and apply freely so as to leave a film on the face. Corrosive sublimate 1/2 to 2 grains Emulsion bitter almonds 4 ounces Mix thoroughly and use to stimulate the skin. Ointment of white precipitate (five to fifteen per cent strength) can be used in place of one above. The hair should be shampooed two or three times a week, to remove sebaceous accumulations and other foreign materials. Carbolic add 15 grains Glycerin 2 drams Cologne water 1 ounce Mix, and apply to the scalp once daily. Precipitated Sulphur 1 dram Lanolin 2-1/2 drams Glycerin 2-1/2 drams Rose water enough to make 1 ounce Mix well. They are circular bald patches which may appear on any hairy part of the body, but more frequently on the scalp. The patient does not sweat enough, especially in certain skin diseases like psoriasis, etc. We all know how disagreeable it is to sit near a person in a street car or any crowded place, who has an odor of perspiration about them, How easy it would be to use this wash and rid yourself of this difficulty," 2. Have a simple blanket soaking in hot water and when all is ready, wring blanket as dry as possible and wrap about the patient up to the neck. Care should be taken not to have the blanket hot enough to burn the patient, but not too cool. After a few minutes the patient is taken out, rubbed dry gently and left to rest and sleep. One per cent solution of potassium permanganate or permanganate of potash is good applied to the parts. Causes-They come as the result of the occupation or pressure, and sometimes without any seeming cause. The latter is done by soaking them with prolonged hot water baths and scraping off the mass afterwards. After this paste has been on the corn for three days, it should be removed and the feet soaked well, and the corn scraped off. In the morning (if the onion has remained over the corn) the soreness will be gone and you can pick out the core. Salicylic Acid 1-1/2 dram Extract of Cannabis indica 10 grains Collodion 1 ounce Mix and paint on the corn for several days and after soaking corn scrape it off with a sharp knife. A Good but Weaker Remedy: Salicylic Acid 30 grains Extract of Cannabis indica 5 to 10 grains Collodion 1/2 ounce Both of these prescriptions are good, the first being stronger with salicylic acid. When the corns are soft with inflammation, wash and dry the foot and apply a solution of nitrate of silver, sixty to one hundred and twenty grains to the ounce of water, to every part every four or five days. It is a hard mass and ends in local death of some of the tissue and formation of pus, which empties upon the surface through several sieve-like openings. The several dead parts may run together until the entire mass separates in a slough. It occurs frequently in patients suffering from diabetes, in whom it is usually fatal. Sometimes it is necessary to go slowly and take out at each dressing only what can be easily removed, It is not always possible to get the whole mass away at once. Opening the carbuncle and giving free drainage afford great relief from the fever and often general symptoms. The dressings frequently become hard and do not absorb all of the material ready to be discharged. There is no danger if the one who dresses it is clean with the instruments, hands and gauze or cotton. Bulkley recommends this lotion: Corrosive Sublimate 5 grains Dilute Acetic Acid 2 drams Borax 40 grains Rose water enough for 4 ounces Shake bottle, mix and apply to the part night and morning. If the skin becomes too scaly, a mild soothing ointment should be substituted for the above. Chlar 2 drams Subnitrate Bismuth 2 drams Starch 1/20 ounce Glycerin 1/2 ounce Mix and apply twice daily. Stomach-bowel disorders, menstrual disturbances and anemia are other causes and assist in making them worse. For this purpose prolonged (ten minutes at a time) bathing of the face with hot water and soap; tincture of green soap in the more indolent, sluggish cases, should precede the pressing out of the blackheads: Lateral pressure with the fingers or with the comedone extractor, especially contrived for this purpose, will express the black-heads. After they are out, the skin dried and cleaned, various stimulating remedies can be applied in ointments and lotions such as following: 1. It can come from injuries, for instance the rubbing or pressure of ill-fitting clothes, bandages, bites of insects and from scratching. Paint the burned part with a one to five per cent solution of cocaine, according to the severity of inflammation. Then apply soothing lotions of equal parts of lime-water and olive or linseed oil; cover the whole with absorbent cotton. The parts can be washed with a solution of boric acid, one teaspoonful to a cup of water; then dust upon the parts sugar of lead once or twice a day. It terminates in a watery or pus-like discharge with the formation of crusts or scaling. There are six cardinal symptoms; inflammation, itching, moisture, crusting, infiltration (liquid filling of the tissues), fissuring or cracking. Fox says that nearly one-third of all skin diseases are eczema in some of its stages or varieties. The skin is dry, of a bright or dull red color, with intense itching or burning, more or less watery swelling in the acute stage. In the chronic stage, the skin becomes thick and covered with fine dry scales, usually in the face (Eczema Erythematosum). When the pustules rupture, their contents dry up to the thick greenish-yellow crusts. In chronic cases they run together, and finally form thick scaly patches, and may run into a scaly eczema. They are various sized and shaped reddish patches, which are dry and more or less scaly. Thickening is always present, also a tendency to cracking of the skin, especially if it affects the joints. Use oily preparations to soften the crusts and then they can be removed with water and good soap. For the acute kind the remedy should be soothing, and more or less stimulating for the chronic forms. In acute cases, with much pouring out of liquid (serum), lotions have a cooling effect. Bathe the affected parts several times daily for fifteen or twenty minutes with this lotion and apply oxide of zinc ointment afterwards. Oxide of Zinc ointment alone, applied night and morning, is valuable in many cases. The Black wash should be used twice a day just before the oxide of zinc ointment is applied. In other cases powdered oxide of zinc is dusted over the part if the discharge is watery or profuse. When the disease is not so acute (sub-acute) applications of a mildly stimulating character are needed. For this purpose, resorcinal in the proportion of two to thirty grains to the ounce of lard, according to the severity and amount of hardness existing. Tincture of green soap used with hot water until the skin is bared and then dress with oxide of zinc ointment. Salicylic acid thirty to sixty grains to an ounce of lard and applied for stimulating purposes. Schalek uses the same remedies in part and the following for a fixed dressing, especially on the eyes. Dress the parts in a thin gauze bandage, over which the melted preparation is painted. I have given many different prescriptions, but those who treat skin diseases know that a great many are needed, for they act differently upon different persons. To prevent scratching, masks must be applied to the scalp and face, or the hands must be tied in bad cases. The local treatment is the same as above except the strength of the drugs used must be reduced in proper proportion. Greatly thickened patches may be softened by soap plasters or bathe the parts in ten or twenty per cent solutions of caustic potash and followed by a salve application. The above remedy was sent in by a number of mothers, all of whom said they had tried it with success when other remedies failed. Elixir, iron, quinine and strychnine from a half to one teaspoonful three times a day is a good tonic for an adult. Paint the inflamed spot when it first begins, with a solution of gun cotton (collodion) and renew it every hour until a heavy contractile coating is formed. Alcohol and camphor applied over the skin in the early stages is recommended by Ringer. When boils occur in the external ear, the canal should be washed out with hot water. The following is good for the pain of a boil: Iodoform 4 grains Menthol 2 grains Vaselin 1 dram Mix and smear a cotton plug and insert in the ear two or three times a day. Wash the abscess and surrounding parts in hot water and good soap, and rinse off with alcohol, a salt solution, or listerine, etc. Dress with a clean linen gauze or absorbent cotton, Poultices may be used if you are careful. The inner dressing should be soft and thick enough to absorb all the secretion given out between dressings. Cook until smooth and creamy, then add enough flour so it will spread but not be dry.
Despite this medicine 60 purchase on line seroquel, he was hospitalized 4 more times for lower respiratory exacerbations medications with sulfa seroquel 200mg fast delivery. He is now being hospitalized for evaluation and treatment of an exacerbation consisting of coughing treatment laryngomalacia infant buy discount seroquel 200mg on-line, wheezing and hypoxemia inoar hair treatment order seroquel us. Auscultation of his chest reveals heterophonous (small airway) and homophonous (large airway) wheezing with diffuse fine crackles x medications seroquel 300 mg without prescription. A chest radiograph shows bibasilar reticulonodular opacities that have been essentially unchanged for almost one year chi royal treatment order seroquel cheap, with new right middle lobe disease. Bronchoscopy with bronchoalveolar lavage reveals erythematous, friable airways with no obvious airway anomalies. Lavage revealed a cell count of 750 per microliter, of which 105 were red blood cells and the remainder white blood cells (70% neutrophils and 30% macrophages). Staining of the lavage fluid with oil red-O reveals numerous lipid-laden macrophages (a marker of chronic aspiration). He is placed on cefuroxime for presumed bacterial bronchitis despite inconclusive cultures. More importantly, he is also started on nasogastric feeds and is not allowed to take anything by mouth. His digital clubbing eventually resolves and a chest radiograph shows no suggestion of bronchiectasis. Bronchiectasis is a chronic lung disease whose pathophysiology is poorly understood. Traction of airways from collapsed surrounding structures, bulging of the airways from retained secretions, weakening of the bronchial wall by infection or inflammation, or combinations of these factors are all suggested mechanisms (2). Single or repeated acute infections, chronic obstruction from congenital anomalies, tumors, cystic fibrosis, chronic asthma or immunodeficiencies may also predispose a patient to developing the disease (3). Bronchiectasis has been termed an "orphan disease" which may not always be considered in the evaluation of children with obstructive pulmonary disease because it has become relatively uncommon in the antibiotic era (1,5). Fifty years ago, Field studied 160 children with bronchiectasis for almost 2 decades (6,7,8,9). In that period, she documented a fall in the annual hospitalization rate for bronchiectasis in five British hospitals (1952-1960) of approximately 48/10,000 to 10/10,000 (9). At our institution among children of American Military members, there have been 14 pediatric cases in the past 19 years including the present case, yielding an approximate rate of 0. The term "bronchiectasis" has traditionally implied permanent, irreversible alteration in the anatomy of the airways (1,10). The diagnosis should be considered in children with daily, productive cough of longer than 6 weeks duration, hemoptysis, children with persistent radiographic infiltrates, digital clubbing or isolated, persistent crackles on auscultation. Traditionally, the diagnosis was made by bronchography (chest radiograph taken with inhaled contrast), as the plain chest radiograph is relatively insensitive for the detection of bronchiectasis (10). The diagnosis is based upon the presence of an internal bronchial diameter greater than the adjacent pulmonary artery, lack of tapering of the bronchial lumina, and visualization of the bronchi within 1 cm of the pleura, although the use of the first of these criteria has been debated (11,12). The combination of small airway obstruction coupled with chronic inflammation of the bronchial wall is most likely the mechanism in the development of bronchiectasis. The inflammation usually results from acute or chronic bacterial infection or "colonization" of the airways (7,10,13). The majority of cases of bronchiectasis follow severe pneumonia or other lower respiratory infection (10). In a series by Field fifty years ago, 24% of cases followed pneumonia, and 33% followed some combination of pertussis and/or measles infections (6). Page 310 Chronic aspiration, either from cricopharyngeal dyscoordination or gastroesophageal reflux, is a recognized condition that can lead to bronchiectasis in adults and children (5,10). It has probably emerged as a more common cause as antibiotics and vaccinations have diminished the other infectious etiologies. In addition, bronchiectasis has been shown to be more common in patients of Polynesian descent (13,14). A ciliary defect is thought to be the etiology but has not been consistently demonstrated (15). Bronchiectasis has also been reported with increased frequency in Native Alaskan children, although some theorize that the common thread is a low socioeconomic level (16,17). Bronchiectasis, particularly the mildest of the pathologic forms, cylindrical bronchiectasis, may be reversible. When associated with pneumonia, it may resolve with treatment of the acute process (18). Resolution of post-obstructive bronchiectasis has even been reported after removal of a chronic foreign body (19). In many cases, the clubbing cleared after the affected section of the lung was removed surgically. In cases treated medically, occasionally the clubbing improved and in some cases it disappeared despite persistent bronchographic evidence of bronchiectasis (6). Of interest, Field concluded, "clubbing when present, usually signified irreversible bronchiectasis, providing there was no congenital cardiac lesion" (6). In the same patient series, Field also described the condition of "reversible bronchiectasis," a temporary dilation of airways in areas of the lung that had been collapsed due to infection or atelectasis (7). She suggested that duration of cough and pulmonary symptoms was commonly of three months duration or less in children with reversible bronchiectasis and pulmonary collapse which reexpanded. In the same series, the majority of children with a history of symptoms for two years or more generally developed severe bronchiectasis (7). The evaluation of a child with bronchiectasis should include an evaluation for any identifiable cause of the condition. Testing for cystic fibrosis with a sweat chloride test as well as genotype determination should be performed in select cases. Children in their first two decades do not usually develop lung disease from alpha-one protease inhibitor deficiency, but a level should be obtained. Evaluation for allergic aspergillus or allergic fungal disease should be considered. Serum levels for pertussis, measles and adenovirus are probably not helpful in a child with bronchiectasis because of immunization and the possibility of previous, unrelated disease (5). Basic aspects of the immune system should be evaluated including serum immunoglobulins and serum IgE. There are cases of bronchiectasis preceding other symptoms of rheumatic disease, sometimes by decades, so an anti-nuclear antibody and rheumatoid factor should be obtained. Finally, a thorough evaluation for gastroesophageal reflux should be undertaken including extended intraesophageal pH probe monitoring (5). Children with bronchiectasis should be treated with antibiotics during symptom exacerbations based upon sputum culture results. Exacerbations should also be treated with increased frequency of the daily regimen of chest physiotherapy and postural drainage, usually conducted twice a day. Bronchodilators are indicated where there is evidence of bronchial hyper-reactivity (8,9,10,13). There may also be a role for inhaled corticosteroids to modulate the host response and curb inflammatory damage to the lung (13). Therapy for an identified cause of bronchiectasis should be undertaken, including aggressive medical and perhaps even surgical therapy for gastroesophageal reflux. When damage is severe and well localized, pulmonary segmental resection may be beneficial (8,9,10). However, Field demonstrated a gradual symptomatic improvement of children who did not have surgical therapy for bronchiectasis, even before the proliferation and availability of broad spectrum antimicrobials (9). Lewiston recommended that surgery be delayed unless symptomatically necessary, until the patient is 6-12 years, because of the possibility of clinical improvement (10). Bronchiectasis has become an uncommon disease in the developed world, but it may often be unrecognized. It should be suspected in children with chronic respiratory symptoms, since it is often amenable to long-term medical management. Surgical therapy should be reserved for situations of recurrent pulmonary sepsis unresponsive to aggressive medical management. True/False: Causes of bronchiectasis in childhood include cystic fibrosis, asthma and immunodeficiency. True/False: Bronchiectasis has been traditionally classified as round, cylindrical or cavitating. True/False: Chronic aspiration is a recognized cause of bronchiectasis in children. True/False: Children of Polynesian descent are at no increased risk of bronchiectasis. True/False: Therapy for bronchiectasis in children includes early surgical resection. Aetiology and pathogenesis, including a survey of 272 cases of doubtful irreversible bronchiectasis. Prophylaxis, treatment and progress with a follow-up study of 202 cases of established bronchiectasis. Mucociliary transport and ultrastructural abnormalities in Polynesian bronchiectasis. Resolution of severe bronchiectasis after removal of long-standing retained foreign body. His mother is unsure if he had eaten anything else with the potato chips and does not think the child turned blue during the choking and gagging episode. He returned to his normal activity shortly after the episode occurred, but since then, he has had a few intermittent coughing spells. He has a normal physical exam except for an occasional low-pitched, monophonic expiratory wheeze heard best over the sternal notch. Since end exhalation films were unable to be obtained, decubitus films were performed. The right lateral decubitus film (right side down) shows air trapping on the right as evidenced by failure of the mediastinum to shift toward the dependent side. The patient is discharged the next morning with follow up scheduled with his pediatrician in the next few days. Of children younger than 15 years, toddlers seem to be the most vulnerable for foreign body aspiration (77% of deaths) (1). Some reasons for this are related to their developmental age such as: 1) exploration of their environment by putting objects into their mouths; 2) learning to walk and run; 3) inadequate dentition; 4) immature swallowing coordination; and 5) supervision by an older sibling. Baharloo, et al, found that 91% of foreign bodies aspirated by children (<8 years old) were organic in nature with peanuts accounting for 54% of that number (2). Meat (especially hot dogs) and other types of nuts are also frequently found on bronchoscopy. They also found that children, unlike adults, did not have a significant difference between the foreign body being found in the right or left bronchial tree (2). This may be explained by the fact that children have symmetric bronchial angles until about 15 years of age. At that time, the aortic knob has developed fully, causing the left mainstem bronchus to be displaced, which creates a more obtuse angle at the carina favoring the right mainstem for a foreign body (3). There are three distinct clinical phases that occur after a foreign body is aspirated (4). The patient will usually experience choking, gagging, coughing, wheezing, and/or stridor. The second phase is the asymptomatic period that can last from minutes to months following the incident. The duration of this period depends on the location of the foreign body, the degree of airway obstruction, and the type of material aspirated. The ease with which the foreign body can change its location is also a factor in the duration of this period. Airway inflammation or infection from the foreign body will cause symptoms of cough, wheezing, fever, sputum production, and occasionally, hemoptysis. Some of these illnesses are: asthma, croup, pneumonia, bronchitis, tracheomalacia, bronchomalacia, vocal cord dysfunction, or psychogenic cough (4). Page 312 the diagnosis and treatment of an aspirated foreign body depends on which clinical phase the patient has on presentation. History, as always, is the best determinant of how suspicious one should be of a potential aspiration. However, this is often complicated by the fact that the event may be unwitnessed, witnessed by a person not present for history taking, or witnessed by an older sibling who may have had a role in the aspiration and chooses not to say anything. On physical exam, the classic findings consist of cough, unilateral decreased breath sounds, and unilateral monophonic wheezing. Although 75% of patients have one or more of these findings, only 40% have all three (5). If stridor (inspiratory and/or expiratory), aphonia, or hoarseness is present, the foreign body is most likely in the larynx or cervical trachea. Since most foreign bodies are not radiopaque, one must rely on indirect findings suggestive of the presence of a foreign body such as: mediastinal shift, atelectasis, and hyperinflation. It has been reported that imaging studies have a sensitivity of 73% and a specificity of 45%, however, up to 20% of patients will have both negative history and radiographic evaluation (6). For patients who present early, radiographic studies must look for evidence of air trapping. However, many foreign body aspirations involve both main stem bronchi or the foreign body is in the trachea. If the expiratory view looks the same as the inspiratory view, this implies bilateral air trapping. Expiratory views rely on timing, so these are sometimes deceiving (an "expiratory view" could have been really taken during inspiration). In a lateral decubitus view, the mediastinum should shift downward toward the dependent side. Thus, if a decubitus view looks the same as an upright inspiratory view, this suggests air trapping on the dependent side. If the patient presents in the first clinical phase, the family and/or health care professional should be advised to follow the recommendations of the American Academy of Pediatrics and American Heart Association (7).
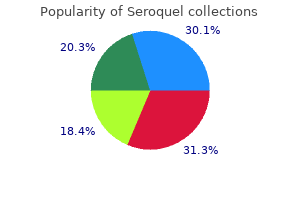
Anesthesia for Liver Transplantation 503 response laboratory service with rapid turnaround times and blood bank services are essential symptoms thyroid problems order generic seroquel. The operation is divided into 3 phases: preanhepatic treatment writing discount seroquel 100mg on-line, anhepatic medicine hat news 200mg seroquel free shipping, and the neohepatic phases medicine effexor seroquel 200 mg visa. Compression or occlu sion of major blood vessels can cause further hemodynamic compromise symptoms of anemia purchase seroquel with visa. This phase ends in the clamping of the inferior vena cava medications zolpidem purchase generic seroquel pills, portal vein and hepatic artery, and removal of the liver. The presence of portal varices and other new vessels in patients with longstanding cirrhosis can ameliorate this effect. Care must be taken not to overcompensate with significant volume expansion, because this volume will return to the circulation upon unclamping. The resulting hypervolemia can lead to venous congestion and poor function of the new liver. With partial return of blood from the inferior vena cava to the heart, hemo dynamics are usually more stable than with a full clamp. Venovenous bypass: Venous blood from the inferior vena cava and femoral vein is returned into the internal jugular vein using extracorporeal venovenous cannulas and a centrifugal pump. As the vena cava is unclamped, adequate return of venous blood volume to the heart is restored. The portal vein is then opened, causing the cold, acidotic, hyperkalemic blood from below the clamp and from the liver graft itself to circulate directly into the right heart. This can cause a significant decrease in blood pressure, bradycardia, other arrhythmias, and occa sionally cardiac arrest. Severe hypotension upon unclamping is called reperfusion syndrome and can be ameliorated by administration of calcium chloride, bicarbonate, epinephrine, and vasopressin. Warm ischemia is very damaging to the graft, and thus limiting warm ischemia time is critical to graft function. The neohepatic phase consists of the hepatic artery and bile duct anastomoses, often with a concomitant cholecystectomy. Hemosta sis requires excellent surgical skills, temperature control and the early diagnosis and treatment of fibrinolysis. Failure to do so leads to breakdown of existing clots and the development of diffuse bleeding. Maintenance of a low central venous pressure may reduce venous bleeding during hepatectomy. Treatment of abnormal laboratory values such as low platelet counts, low fibrin ogen, and high prothrombin times is only required if there is clinical bleeding. These laboratory values frequently normalize as the new graft functions and platelets return to the circulation from the spleen. In case of bleeding, patients are treated with factor replacement, blood, and platelets. Approaches to resuscitation and treatment of high blood loss differ by institution. Renal dysfunction, with poor urine output and rising creatinine, may occur during transplantation, especially after a full caval clamp, long anhepatic time, or prolonged hypotension. Patients with volume overload, hyperkalemia, or hyponatremia may benefit from continuous venovenous hemodialysis that can be instituted in the oper ating room or upon arrival to the intensive care unit. They must meet usual standard Anesthesia for Liver Transplantation 505 extubation criteria. In some institutions, extubated patients with good liver function can bypass the intensive care unit and are sent to the postoperative recovery unit and then to a regular surgical floor or step-down unit. Occasionally, the abdominal distension owing to an especially large organ or tissue swelling might prevent primary closure of the surgical wound. Abdominal closure can be delayed for several days af ter transplantation to prevent abdominal compartment syndrome. Function of the new graft must be moni tored closely, looking especially for signs of infection, bleeding, and acute rejection. Some patients with bleeding or graft dysfunction may require emergent return to the operating room. Patients may have a difficult postoperative course with significant multiorgan dysfunction, and these patients require expert intensive care. Does intraoperative hepatic artery flow pre dict arterial complications after liver transplantation Evaluation and management of hepatic en cephalopathy: current status and future directions. Hepatic encephalopathy in chronic liver dis ease: 2014 Practice Guideline by the American Association for the Study Of Liver Diseases and the European Association for the Study of the Liver. Complications and use of intracranial pressure monitoring in patients with acute liver failure and severe encephalopa thy. Clinical management of acute liver fail ure: results of an international multi-center survey. Diastolic cardiac dysfunction is a predictor of dismal prognosis in patients with liver cirrhosis. Diastolic dysfunction is a predic-tor of poor outcomes in patients with cirrhosis, portal hypertension, and a normal creatinine. Diastolic dysfunction in liver cirrhosis: prognostic predictor in liver transplantation Effectively screening for coronary artery disease in patients undergoing orthotopic liver transplant evaluation. The prevalence of coronary artery dis ease in liver transplant candidates over age 50. Factors associated with major adverse cardiovascular events after liver transplantation among a national sample. Liver transplantation outcome in patients with angiographically proven coronary artery disease: a multi-institutional study. Intraoperative management of liver transplantation in patients with hypertrophic cardiomyopathy: a review. The perioperative management of patients undergoing combined heart-liver transplantation. Evaluation for liver transplantation in adults: 2013 practice guideline by the American Association for the Study of Liver Dis eases and the American Society of Transplantation. Hepatopulmonary syndrome and liver transplantation: a recent review of the literature. Improved survival after liver transplantation in patients with hepatopulmonary syndrome. Retrospective analysis of the re sults of liver transplantation for adults with severe hepatopulmonary syndrome. Severe pulmonary hypertension and amelioration of hepatopulmonary syndrome after liver transplantation. Association between primary pulmonary-hypertension and portal-hypertension analysis of its pathophysiology and clinical, laboratory and hemodynamic manifestations. Survival in portopulmonary hypertension: Mayo Clinic experience categorized by treatment subgroups. International liver transplant society prac tice guidelines: diagnosis and management of hepatopulmonary syndrome and portopulmonary hypertension. Rebalanced hemostasis in patients with liver disease: evi dence and clinical consequences. Hemostasis in liver transplantation: pathophys iology, monitoring, and treatment. Intraoperative hypercoagulability during liver transplantation as demonstrated by thromboelastography. The coagulopathy of chronic liver disease: is there a causal relationship with bleeding Transesophageal echocardiography during orthotopic liver transplantation: maximizing information without the distraction. Anesthesia for liver transplantation in United States academic centers: intraoperative practice. Postreperfusion syndrome during liver transplantation for cirrhosis: outcome and predictors. Effect of low central venous pressure andphlebotomy on blood product transfusion requirements during liver transplanta tions. Effects of continuous octreotide infusion on intraoperative transfusion requirements during orthotopic liver transplantation. The following collection of information from many sources is designed to be a quick reference for anyone who is involved in the preparation of the patient for non-cardiac surgery. These are proposed guidelines and in no way should supersede good clinical evaluation and assessment. I am assuming that the high-risk procedures may include lower extremity bypass, aortic aneurysm repair, and carotid endarterectomy. I would suggest at this decision point that a second option would be to undergo an operation with invasive preopera tive monitoring and optimization. These decisions should be made between the surgeon and the patient with the understanding of what the risk entails. Comfortable at rest, but less than ordinary activ ity causes fatigue, palpitation, or dyspnea. Scheie: Defciency of A-iduronidase, cloudy cornea, normal intelligence, peculiar facies. Yes Yes Pheochromo Perform is renal Yes Renal artery cytoma clonidine angiography stenosis suppression test postive Nearly 50% of deaths due to unsuspected pheochromocytomas occur during anesthe sia and surgery or parturition. After 2 to 12 weeks, circulation improves and lung function increases by up to 30%. At the 5-year mark, the death rate from lung cancer for the average former pack-a-day smoker decreases by almost 50%. Adequate preoperative treatment is associated with a reduced incidence of serious cardiovascular complications. Also, this classifcation is limited to persons who are neither taking antihypertensive drugs nor acutely ill. For amoxicillin/peni ciillin-allergic patients, the Heart Association recommended: Erythromycin ethylsuccinate 800 mg or erythromycin stearate 1. Pharmacists generally agree that 250 mg of tearate is roughly equivalent to 500 mg of the ethylsuccinate. Complete infusion within 30 patients allergic to minutes of starting the procedure. Croup, bronchitis, pneumonia (current or Airway irritability with tendency for cough, laryngospasm, broncho recent) spasm Papillomatosis Airway obstruction Tetanus Trismus renders oral intubation impossible. Sarcoidosis Airway obstruction (lymphoid tissue) Angioedema Obstructive swelling renders ventilation and intubation diffcult. Preoperative Evaluation of the Pulmonary Patient Undergoing Non Pulmonary Surgery. They are usually unpredictable and are not observed during conventional pharmacological and toxicological screening programs. In contrast, an intolerance to a drug is categorized as a type A (augmented) adverse drug reaction. They are usually dose-dependent and although their incidence and morbidity are often high, their mortality is generally low. Example: A patient comes to the emergency room with sustained chest pain and history of angina, hypertension, and coronary artery disease. Morphine (and other narcotic analgesics to a lesser de gree) is desirable for pain associated with ischemia because of its cardiovascular effects of venous pooling in the extremities causing decreased peripheral resistance. Acute pericarditis typically appears within a year of therapy and may result in tamponade. Chronic pericarditis may resolve spontaneously or may progress to constrictive pericarditis. The side effects to the nitrosoureas are quite similar and these agents have not been subcategorized. Report to the Ranking Minority Member, Committee on Commerce, House of Representatives. Hypertension, or abnormally high blood pressure, is a leading risk factor for cardiovascular disease. In the United States, there are approximately 67 million adults who have hypertension, of whom over half do not have it under control. Among the adults whose hypertension was not under control, 14 million were unaware they had hypertension. Managing high blood pressure is important because if left uncontrolled, it can lead to other health conditions and even death. Health consequences of high blood pressure may include: Coronary artery disease Heart attack Heart disease Congestive heart failure Stroke Kidney damage Vision loss Erectile dysfunction in males What is hypertension Blood pressure is the force being applied against arterial walls as the heart pumps blood throughout the body.
Additional information: