Zoran S. Nedeljkovic, MD
- Assistant Professor of Medicine
- Department of Medicine, Section of Cardiology
- Boston University School of Medicine
- Interventional Cardiologist
- Boston Medical Center
- Boston, Massachusetts
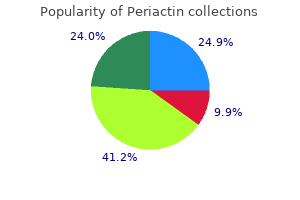
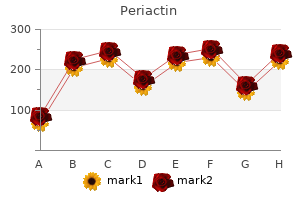
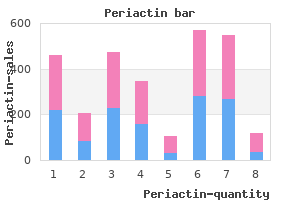
Key principles of infection prevention and control in an outpatient setting are as follows: 1 Centers for Disease Control and Prevention allergy testing joondalup periactin 4 mg with amex. Guideline for isolation precautions: preventing transmission of infectious agents in health care settings 2007 allergy symptoms hay fever order periactin 4mg without a prescription. Policies for children who are suspected of having contagious infections allergy testing japan cheap generic periactin canada, such as vari cella or measles allergy forecast green bay wi periactin 4mg generic, should be implemented allergy symptoms wasp sting buy discount periactin online. Immunocompromised children and neonates should be kept away from people with potentially contagious infections allergy forecast allen tx discount periactin express. In health care settings, alcohol-based hand products are preferred for decon taminating hands routinely. Soap and water are preferred when hands are visibly dirty or contaminated with proteinaceous material, such as blood or other body fuids. Alcohol is preferred for skin preparation before immunization or routine venipuncture. Skin preparation for inci sion, suture, or collection of blood for culture requires 70% alcohol, alcohol tinctures of iodine (10%), or alcoholic chlorhexidine (>0. The use of safer medical devices designed to reduce the risk of needle sticks should be implemented. Sharps disposal containers that are impermeable and puncture resistant should be available adjacent to the areas where sharps are used (eg, areas where injections or venipunctures are performed). Sharps containers should be replaced before they become overflled and kept out of reach of young children. Policies should be established for removal and the disposal of sharps containers consistent with state and local regulations. Physicians can prepare patients and families about the need for private time by educating both parents and pre adolescents about the need for confdentiality as adolescence approaches. For adolescent females who are immunosuppressed or immunocompromised, yearly Papanicolaou smears should begin with the initiation of consensual sexual intercourse or with a history of nonconsensual sexual intercourse. Sexually active adolescent females should be screened at least annually for chlamydia and gonorrhea. All adolescents should receive hepatitis B virus immunization if they were not immunized earlier in childhood. Hepatitis A vac cine should be offered to adolescent males who have sex with males (see Recommended Childhood and Adolescent Immunization Schedules, 1. Patients and their partners treated for gonorrhea, Chlamydia trachomatis infection, and trichomoniasis should be advised to refrain from sexual intercourse for 1 week after completion of appropriate treatment. Retesting to detect therapeutic failure (tests of cure) for patients who receive recommended treatment regimens for Neisseria gonorrhoeae or C trachomatis infection is not recommended unless therapeutic adherence is in question or symptoms persist. Repeat testing is recommended for these infections within 3 months because of the likelihood of reinfection as a result of nontreatment of a current sexual partner and/or new infection from a new sexual partner. Therefore, tests that allow for isolation of the organism and have the highest specifcities must be used. Specimens for culture to screen for N gonorrhoeae and C trachomatis should be obtained from the rectum and vagina of girls and from the rectum and urethra of boys. Specimens for culture to screen for N gonorrhoeae also should be obtained from the pharynx, even in the absence of symptoms. Culture and nucleic acid hybridization tests require female endocervical or male urethral swab specimens. Endocervical specimens for culture are not required for prepubertal girls but are required for culture of C trachomatis and N gonorrhoeae if the female is pubertal or postmenarcheal. If vaginal discharge is present, specimens for wet mount for Trichomonas vaginalis and wet mount or Gram stain for bacterial vaginosis may be obtained as well. Completion of the hepatitis B immu nization series should be documented, or the patient should be screened for hepatitis B surface antibody. Anogenital gonorrhea in a prepubertal child indicates sexual abuse in virtually every case. All confrmed cases of gonorrhea in prepubertal children beyond the neonatal period should be reported to the local child protective services agency for investigation. In an infant or toddler in diapers, genital herpes may arise from any of these mechanisms. In a prepubertal child whose toilet-use activities are independent, the new occurrence of genital herpes should prompt a careful investigation, including a child protective services investigation, for suspected sexual abuse. However, a new diagnosis of trichomoniasis in an older infant or child should prompt a careful investigation, including a child protective services investigation, for suspected sexual abuse. Although hepatitis B virus, scabies, and pediculosis pubis may be transmitted sexually, other modes of transmission can occur. The discovery of any of these conditions in a pre pubertal child does not warrant child protective services involvement unless the clinician fnds other information that suggests abuse. The presence of T vaginalis and bacterial vagi nosis in a pubertal and postpubertal female suggests sexual contact and should be investi gated appropriately (see Bacterial Vaginosis, p 247). Physicians are required by law to report abuse to their state child protective services agency. Most experts recommend universal screening of postpubertal patients who have been victims of sexual abuse or assault because of the possibility of a preexisting asymp tomatic infection. Only tests with high specifcities should be used, and whenever possible, specimens should be obtained by health care pro fessionals with experience in the evaluation of children who have been sexually abused or assaulted. A follow-up visit approximately 2 to 6 weeks after the most recent sexual exposure may include a repeat physical examination and collection of additional speci mens. Many experts believe that prophylaxis is warranted for postpubertal female patients who seek care within 72 hours after an episode of sexual victimization because of the possibility of a preexisting asymptomatic infection, the potential risk for acquisition of new infections with the assault, and the substantial risk of pelvic infammatory disease in this age group. Postmenarcheal patients should be tested for pregnancy before antimicrobial treatment or emergency contraception is given. Prophylaxis After Sexual Victimization of Preadolescent Children Weight <100 lb (<45 kg) Weight 100 lb (45 kg) For prevention of gonorrhea 1. Consider adding prophylaxis laxis for trichomoniasis and against trichomoniasis and bacterial vaginosis (metro bacterial vaginosis (metro nidazole, 15 mg/kg per day, nidazole, 2 g, orally, in a orally, in 3 divided doses for single dose) 7 days; maximum 2 g) See text for human immunodefciency virus infection prophylaxis in children following sexual abuse or assault. Although emergency contraception is most effective if taken within 72 hours of event, data suggest it is effective up to 120 hours. The number of arrests of juveniles (younger than 18 years of age) in the United States was 2. Juveniles accounted for 16% of all violent crime 2 arrests and 26% of all property crime arrests in 2008. On any given day, approximately 120 000 adolescents are held in juvenile correctional facilities or adult prisons or jails. Incarceration periods of at least 90 days await 60% of juvenile inmates, and 15% can expect to be confned for a year or more behind bars. Males account for approximately 85% of juvenile offenders in residential placement, and 61% of juveniles in correctional facilities are members of ethnic or racial minority groups. Juvenile offenders commonly lack regular access to preventive health care in their communities and suffer signifcantly greater health defciencies, including psychosocial disorders, chronic illness, exposure to illicit drugs, and physical trauma when compared with adolescents who are not in the juvenile justice system. Personal knowledge of an infection and its transmissibility may allow youth to take preventive measure to reduce their risk to others. Fewer than 3% of new hepatitis virus infections of all types are acquired once incarceration has occurred. Most juvenile offenders ultimately are returned to their community and, without intervention, resume 1 Centers for Disease Control and Prevention. Prevention and control of infections with hepatitis viruses in correctional settings. Correctional facilities, in partner ship with public health departments and other community resources, have the opportu nity to assess, contain, control, and prevent liver infection in a highly vulnerable segment of the population. The extremely high rate of chronic carriage after infection increases the risk of transmission when youth are released into their communities. The controlled nature of the correctional system facili tates initiation of many hepatitis-prevention and treatment strategies for an adolescent population that otherwise is diffcult to reach. Hepatitis A Correctional facilities in the United States rarely report cases of hepatitis A, and national prevalence data for incarcerated populations are not available. States that have assessed prevalence of past infection in incarcerated populations younger than 20 years of age show a similar ethnic distribution of predominance in American Indian/Alaska Native and Hispanic inmates and documented and undocumented people from Mexico, as is refected in the population as a whole. Risk factors that could contribute to outbreaks of hepatitis A among adolescents include using injec tion and noninjection street drugs, having multiple sexual partners, and participating in male-with-male sexual activity. However, adolescents who have signs or symptoms of hepatitis should be tested for seromarkers of acute hepatitis A, acute hepatitis B, and hepatitis C. Adolescents in correctional facilities may include foreign-born (eg, Asia, Africa) residents who can have chronic infection and can transmit infection to susceptible residents. Adolescent female inmates present additional challenges for hepatitis B assessment and management if they are pregnant during incarceration, in which case coor dination of care for mother and infant become paramount. Adolescent detain ees with signs and symptoms of hepatitis disease should be tested for serologic markers for acute hepatitis A, acute hepatitis B, and hepatitis C to determine the presence of acute or chronic infection and coinfection. Routine preimmunization and postimmunization serologic screening is not recommended. Chronically infected people may remain infectious to sexual and house hold contacts for life and must be counseled accordingly to protect sexual partners and household contacts. Inmates commonly refuse testing, even when at high risk of hepatitis, to avoid persecution from fellow prisoners. In recent years, more than 90% of international adoptees are from Asian (China, South Korea, Vietnam, India, Kazakhstan, and Philippines), Latin American and Caribbean (Guatemala, Colombia, and Haiti), Eastern European (Russia and the Ukraine), and African (Ethiopia, Nigeria, Liberia, and Ghana) countries. The diverse birth countries of these children, their unknown medical histories before adoption, their previous living circumstances (eg, orphanages and/or foster care), and the limited availability of reliable health care in some resource-limited countries make the medical evaluation of interna tionally adopted children a challenging but important task. Internationally adopted children typically differ from refugee children in terms of their access to medical care and treatment before arrival in the United States and in the frequency of certain infectious diseases. Many refugee children may have resided in refu gee camps for months before resettlement in the United States and will have had access to limited medical care and treatment services. However, this examination is limited to completing legal requirements for screening for certain communicable diseases and examination for serious physical or mental defects that would prevent the issue of an immigrant visa. During preadop tion visits, pediatricians can stress to prospective parents the importance of acquiring immunization and other health records. Internationally adopted children who are 10 years of age and younger may obtain a waiver of exemption from the Immigration and Nationality Act regulations pertaining to immunization of immigrants before arrival in the United States (see Refugees and Immigrants, p 101). Children adopted from countries that are not part of the Hague Convention can receive waivers to have their immunizations delayed until arrival in the United States ( However, the child should be seen by his or her pediatrician or a physician 1 For additional information, see Canadian Paediatric Society. Infectious diseases are among the most common medical diagnoses identifed in international adoptees after arrival in the United States. Children may be asymptomatic, and therefore, the diagnoses must be made by screening tests in addition to history and physical examination. In addition to these infectious disease screening tests, other medical and developmental issues, including hearing and vision assessment, evaluation of growth and development, nutritional assessment, blood lead concentration, complete blood cell count with red blood cell indices and differential of white blood cells Table 2. Parents who have not met with a physician before adoption should notify their physician when their child arrives so that a timely medical evaluation can be arranged. Internationally adopted children should be examined as soon as possible after arrival in the United States, prefer ably within the frst 2 weeks after arrival. A list of pediatricians with special interest in adoption and foster care medicine is available on the American Academy of Pediatrics Web site at 2. Over the past 5 to 10 years, the number of countries with routine infant hepatitis B immunization programs has increased markedly. However, administration of a birth dose of hepatitis B vaccine, needed to prevent perinatal transmission from an infected mother, is not routine in many countries, and coverage among infants can be suboptimal. Although hepatitis B serologic tests are per formed routinely in the country of origin, testing may be incomplete and children may become infected after testing. Serologic test ing for acute infection (hepatitis A IgM) and immunity (total hepatitis A antibody) can be performed at the initial visit to determine whether the child has a current hepatitis A infection or immunity. In addition, hepatitis A vaccine should be administered to all susceptible nontravel ing people who anticipate having close personal contact with a child adopted internation ally from a country with high or intermediate hepatitis A endemicity before arrival of the adoptee. Adopted children or their household or other close contacts with symptoms con sistent with acute viral hepatitis should be evaluated promptly. Children without hepatitis A immunity who are 12 months of age and older should receive hepatitis A vaccine as recommended according to the routine immunization schedule 1. Intestinal Pathogens Fecal examinations for ova and parasites by an experienced laboratory will identify a pathogen in 15% to 35% of internationally adopted children. The prevalence of intes tinal parasites varies by age of the child and country of origin.
Syndromes
- A broken bone
- Pulmonic stenosis
- Hemorrhage
- Superficial skin infections such as folliculitis and impetigo
- Skin biopsy of tumors
- One shoulder is higher than the other
If the cord has prolapsed allergy symptoms icd 9 purchase periactin overnight, put the mother in the the management of preterm labour is not a success story allergy medicine urination proven 4 mg periactin. If there is a delay allergy symptoms breathing difficulty order periactin no prescription, filling the supervised especially if there might be a hidden maternal bladder via a catheter with the help of an infusion bag of cardiac abnormality allergy medicine rx purchase periactin 4mg without a prescription. It often stops spontaneously allergy medicine you have to sign for periactin 4 mg fast delivery, and 70% of than when the membranes are ruptured some time before mothers do not deliver within 48hrs allergy symptoms and fever buy periactin 4mg free shipping, and start labour delivery. You can try to postpone delivery for at least 48hrs in order to ripen the foetal lungs with 12mg N. Using misoprostol to prime the cervix/induce membranes have not ruptured, assess as follows: labour has as disadvantage that the medication cannot be (1) In the active phase of labour (the cervix is >3cm), controlled as easily as an oxytocin infusion. On the other try to delay delivery with nifedipine (or indomethacin if at hand with misoprostol, the membranes do not need to be <30wks) in order to gain time to ripen the foetal lungs with ruptured till (very) late in labour making mother-to-child steroids. If the cervix is sill closed, as it often is, (7) an extra-uterine gestation (rare, 20. Teach that premature rupture of in the next pregnancy use them in the 2nd trimester for the membranes means there needs to be a very good 1wk. Handle the foetus occasionally you might detect a cord prolapse: you can gently and keep him warm, using the kangaroo method usually rule it out confidently; you may also deduce a. Loss of fluid from the vagina, before the onset of regular painful contractions, is diagnostic. If you are not sure of the dates, or there appears to be a discrepancy, assess the foetal age by ultrasound (38. When labour is normal, regular contractions start and the Start by separating the labia and asking for a cough: cervix begins to dilate before the membranes rupture and is liquor discharging from the vagina Make sure that a senior the advantages of expectant treatment (not inducing person does this, so that it need not be repeated. These are: a vaginal examination is much more reliable than visual (a) failure, which means that you will need to perform a inspection, Caesarean Section, and (2) feel the degree of cervical effacement, (b) the side-effects of oxytocin (21. Do not do a vaginal examination with until contractions are well established, ungloved fingers: the risk of infection is too high. Liquor, but not urine, or a discharge, will dry starts successfully within this time. Peculiarly, the foetus which is most often dead, may appear to be crying If gestation is <28wks, with a live foetus, and there are in the uterus because gas makes it possible to produce no signs of infection, the chances of the pregnancy sound. If gestation is 28-35wks, treat prophylactically with A foetus >2wks postmature is at increased risk of stillbirth, antibiotics, preferably erythromycin. If you use antibiotics before there are signs of 42wks significantly reduces the perinatal mortality. Once an obvious infection is established, induction is the risks of accidental premature induction are needed as well as antibiotics as before to prevent spread of considerable: this infection. Thus, if periods occur every 2months, If it continues to drain at 48hrs, induce labour, if the risk conception will occur 6wks after the last period, instead of of infection is high. There is a high risk of septicaemia with (9) A dead foetus: do not rupture the membranes. Empty the uterus as soon as assumed to be present, but is in fact the whole uterus! If you have the misfortune to find a grossly this is simplest under ultrasound guidance. If you are not abnormal conjoined twin, Caesarean Section is the method sure of the diagnosis, or do not feel you can risk of choice. Anencephaly is complicated in 90% of cases by the alternatives are: polyhydramnios; so when you diagnose this, (1);The best, to drain the head before making the uterine do an ultrasound on the mother to see if the foetus has a incision; brain (38. If not, it is usually stillborn, and even when it nd (2);2 best, to make a transverse, curved incision 4cm is born alive, it does not survive >6hrs. When you have higher than normal with the ends near the attachments of explained the diagnosis to the mother, she may insist that the round ligaments; the pregnancy is terminated. If you suspect it, confirm the because you made the incision in the direction of the diagnosis by ultrasound (38. If the diagnosis is In order to avoid a Caesarean Section when there is no doubtful, wait. Sometimes you have to not, and the membranes are intact, there is no hurry manipulate the foetus through the abdominal wall in anyway. To perforate the foetal head vaginally, wait until the cervix A breech presentation is no problem. Use low doses of is >3cm dilated, then drain the cerebrospinal fluid with a misoprostol erring on the side of too little because there is large needle or artery forceps between the widely no medical hurry. If anencephaly is not accompanied by polyhydramnios In this situation, however, you are committed because the (10%), pregnancy may rarely be prolonged up to 1yr or membranes are ruptured and if labour has not started or more, and make delivery difficult. Misoprostol is the drug stops, you might have to perform a Caesarean Section on a of choice also, the dose depending on the parity and dead or non-viable foetus. If you make the diagnosis during pregnancy, If you make the diagnosis during a breech try to measure the size of the foetal head and determine if presentation, (22. Often you are parents, explaining the need for a ventriculo-peritoneal alerted to the hydrocephalus by seeing clubfeet (32. Do not endanger the life of the as the hydrocephalic head fails to enter the pelvic brim. If, at this stage you see the commonly associated In this case, induce labour without artificial rupture of meningomyelocoele, pass a steel or gum elastic male membranes. The district these risks must be compared not only with the risks of doctor failed to notice that this was because there was a hydrocephalus: breech delivery but also of Caesarean Section. The foetus was put on the resuscitation table but not experienced midwives as often as it should be; it should attended to because everybody thought it was dead. It survived for 6months, paralysed from the waist down because perinatal mortality with breech deliveries is >2%, after of a spina bifida. It dribbled urine continuously and probably died of an correcting for prematurity and foetal abnormality urinary tract infection. This should be fairly easy to calculate from your labour ward record books, which should routinely record presentation, birth weight, obvious abnormalities, and live 22. Work out your perinatal mortality for all babies If a foetus presents with his buttocks (breech) or his (10-80/1000) excluding breeches, babies <25kg, twins, foot, he is about four times more likely to die than if he and babies with obvious malformations. This is so, even if you exclude the period lasts (in this case) from the 28th week to the end of the 1st week of life. An incompletely dilated cervix (especially with available skilled personnel and/or patients arriving too straining before full dilatation, or prematurity). These are exactly the same factors which make it very (4) the increased risk of cord prolapse. Muslim, 22-2C) is an alternative to manipulation that (4) Abdominally, by Caesarean Section. This may allow the foetal In breech extraction you, rather than the mother, provide breech to disimpact from the pelvis, so that it can turn the power for expulsion. Only do this extraction if there is no alternative (foetal distress) or with the 2nd of twins. If you can reduce the number of breeches you deliver, you will reduce the perinatal mortality associated with them. Perhaps an acceptable approach in nullipara would After 36wks, a foetus gradually becomes less mobile, be to prepare for a Caesarean Section at 36-37wks. However, a mother who has previously delivered spontaneously vaginally around term has certainly no indication for an elective Caesarean Section for a simple breech presentation. Judgement is difficult nonetheless, if for example a primipara delivered by vacuum extraction the last time. Performing an elective Caesarean Section for breech presentation without very good reasons is irresponsible, if you cannot guarantee good supervision for trial of scar and access to a Caesarean Section for the next delivery. A liberal Caesarean Section rate will reduce your perinatal mortality, but you will have to weigh this against the increased maternal morbidity and mortality that will follow. If the difficulties of vaginal breech delivery worry you, and you are tempted to perform a Caesarean Section for all breech presentations, remember the dangers of anaesthesia, bleeding, sepsis, and a scarred uterus. However, if your hospital has not the skill available continuously to perform a vaginal breech delivery and. Flex the foetus between your hands so these skills, then you might be forced to perform an that you make him do a forward somersault. Much depends on the foetal age: manipulations that you have to do in the second stage of a (1) <28wks gestation (<1kg): the chances of life are small, vaginal delivery much easier. However, about 20% have severe abnormalities, and if you do not have ventilators, even the normal ones have a poor chance of surviving. So, in an area of high parity and high perinatal mortality, you should rarely perform a Caesarean Section for a premature breech presentation. It is important to dissuade the mother from pushing before full dilatation: do not leave her alone! You may not succeed >36wks, but it is still worth foetus is normal-sized, she will probably deliver vaginally. The best assurance of an adequate pelvis is of course pregnancy for some other reason. Mortality related to rhesus antibodies (fundal height >40cm), regardless of the size of the pelvis. A previous stillbirth, especially if it was associated is planning to breast feed then perhaps you should proceed with a breech or instrumental delivery. Previous operative vaginal deliveries unless certainly patient has greater risks for the mother (not the foetus). Empty the look for failure to progress which is not quickly amendable bladder and lie the patient supine tilted a little to one side. Make sure your hands are warm (2) Arrest at the brim, or delay in the descent of the breech and she is comfortable. Place one hand below the breech, to push before full dilatation, as the foetal feet enter the and your other hand above the head. This can result in the head being caught behind the between your hands, so that you make him do a forward undilated cervix. Cord presentation or prolapse: this is especially a side and wait until it is >100. If the membranes have ruptured but there most If both fail, rest mother with the foot of the bed raised. Most additional factors, which compromise the wellbeing If you succeed, see her again 1wk later to make sure the of a foetus, are indications for a Caesarean Section. Only for a healthy normal-sized mother with a foetus <37kg (as indicated by a fundal height of <40cm), If you cannot turn her foetus by 37wks, manage her as a who progresses normally in both stages of labour, should breech delivery. For breech delivery you need a quiet atmosphere and good communication with the patient. If the cervix dilates at <1cm/hr in the active phase, or there are any other signs of delay not quickly remediable by oxytocin, perform a Caesarean Section. Until the foetal buttocks are delivered, you can still elect to perform a Caesarean Section. If there is any delay before the delivery of the buttocks, go ahead with the Caesarean Section. A common fault is to try to deliver a breech through an incompletely dilated cervix, which may force the arms to extend and make the head difficult to deliver. Full dilation may not be easy to diagnose in a breech, so take your time for a proper vaginal examination. Put the mother into the lithotomy position (essential if you effect the Burns-Marshall manoeuvre) when the posterior buttock is distending the perineum. As soon as she wants to bear down, do a vaginal examination to make sure that. The breech should advance with A, allow the body to hang, until you can see the hair at the back of every contraction. Protect the scrotum (you do not want the If the head does not immediately deliver spontaneously episiotomy to castrate him! The foetus should be appear, pause, and ask your assistant to clear the airways delivered in the next 3mins. The shoulders and arms should deliver with a twisting movement, and the head should follow immediately. If you cannot get at least the mouth and nose into fresh Do not touch the baby, or try to disentangle the legs, air with the Burns-Marshall method, use: until you see the umbilicus. When the umbilicus appears, (2) apply Wrigley (outlet) forceps to the aftercoming head. Try to make sure that the foetal back is Rest the foetal belly and chest on your right forearm; uppermost. Never allow the foetal abdomen to face put your gloved right middle finger in the mouth, and your upwards. Put your left When the scapulae appear (and not before), search for the hand over the back; put your middle finger on the occiput arms in front of the chest. If, as is usual, the arms are not and your index and ring fingers over the shoulders. This will give you some control over the flexion and You should be able to deliver one or both of them. Grip the skull and guide it through the have difficulty, feel up to the shoulder from the foetal back birth canal. Ask your assistant to put his fist on the foetal head, Allow the body to hang (22-3A).
This condition is usually seen in patients with an underlying rotator cuff tendinitis or bicipital tendinitis but has also been associated with stroke allergy medicine depression buy periactin 4 mg without a prescription, myocardial infarction allergy treatment denver periactin 4mg mastercard, cervical radiculopathy allergy forecast hong kong cheap periactin 4 mg on line, and pulmonary disease allergy medicine enlarged prostate best order periactin. The pathophysiology of frozen shoulder is unclear allergy count nyc 4 mg periactin overnight delivery, and controversy exists as to how significantly capsular inflammation or fibrosis really contributes to the loss of motion that is characteristic of the condition allergy forecast woodbridge va order periactin 4 mg on line. Surgical procedures, capsular distention with saline injection, and closed manipulation have reportedly been useful in individual cases. Suprascapular nerve blockade has been shown to improve pain but does [33] not improve function or range of motion in patients with frozen shoulder. Myofascial Shoulder Pain Syndrome Myofascial shoulder pain syndromes are characterized by pain over the trapezius or medial or lateral scapular borders posteriorly, with the finding of reproducible trigger points. These poorly characterized syndromes usually respond to local injection with glucocorticoids and an anesthetic, though local modalities may be needed in more chronic cases. Chest Wall Pain Musculoskeletal chest wall pain syndromes account for about 10% to 15% of cases in which adults are seen for chest pain in the emergency room setting, and they account for about 15% to 20% of patients who have had chest pain but [34] whose coronary angiograms are negative. In rare cases, chest pain may result from Tietze syndrome-a benign, painful, nonsuppurative localized swelling of the costosternal, sternoclavicular, or costochondral joints, most often involving the area of the second and third ribs. More often, patients with musculoskeletal chest wall syndromes have a more diffuse pain syndrome, termed costochondritis or costosternal syndrome, the specific etiology of which is not well understood. Areas of tenderness are not accompanied by heat, erythema, or swelling; multiple areas of tenderness are found, usually in the upper costochondral or costosternal junctions. A number of less common chest wall syndromes have been described, each defined by the area of tenderness. Musculoskeletal chest wall syndromes are usually self-limited and respond to analgesics, local heat, stretching exercises, and local glucocorticoid injection. Elbow Pain the most common nonarticular syndromes of the elbow include epicondylitis, olecranon bursitis, and ulnar nerve entrapment. Epicondylitis Epicondylitis is caused by an inflammation at the origin of the tendons and muscles serving the forearm; it is usually caused by overuse or by repetitive activity. A similar, less common process may affect the flexor muscles originating at the medial epicondyle. Local infiltration of glucocorticoids and lidocaine often results in more rapid improvement than other [35, 36] measures in the first month or two but does not appear to affect the outcome over 6 to 12 months. Olecranon Bursitis Olecranon bursitis presents as a discrete swelling with palpable fluid over the tip of the elbow. Infectious bursitis-usually caused by gram-positive skin organisms-is accompanied by heat, erythema, and induration. When infection is suspected, prompt aspiration and culture of the fluid are mandatory. Antibiotics should be started empirically, and the bursa should be reaspirated frequently until the fluid no longer [37] reaccumulates and cultures are negative. Olecranon bursitis may also be part of rheumatoid arthritis or gout, usually in a patient in whom a diagnosis has already been made. On occasion, an initial diagnosis of gout is made by examination of bursal fluid for urate crystals. Patients typically complain of pain and numbness that radiates from the elbow to the little finger and the medial side of the hand. An increase in paresthesia with elbow flexion is helpful in making the diagnosis, but nerve conduction studies are often needed to confirm the diagnosis. Conservative therapy with a loose cast may help limit elbow flexion and improve symptoms in some patients; surgical decompression is indicated in patients with disabling pain or weakness. Hand and Wrist Pain Painful conditions of the tendons and tendon sheaths of the hand and wrist are often related to repetitive or unaccustomed activities. The resultant edema, inflammation, and fibrosis of the structures interfere with the normal function of the tendon as it moves within the sheath. De Quervain Tenosynovitis and Flexor Tenosynovitis De Quervain tenosynovitis affects the abductor pollicis longus and extensor pollicis brevis. Typical symptoms are pain over the radial aspect of the wrist during activities and tenderness that is usually found over the affected tendons proximal to the level of the carpometacarpal joint of the thumb. Pain is reproduced by stretching the tendons with the thumb inside a closed fist. Flexor tenosynovitis, or trigger finger, is caused by involvement of the flexor tendons of the digits, usually at the level of the metacarpophalangeal joint. Patients complain of locking of the affected digit in a flexed position, often with a sudden painful release on extension. Treatment of de Quervain tenosynovitis and flexor tenosynovitis may require rest, local heat, immobilization with a splint, or local infiltration with glucocorticoids. Entrapment is usually associated with flexor tenosynovitis related to overuse or trauma. In addition, an association has been observed with medical conditions such as diabetes mellitus, rheumatoid arthritis, pregnancy, and hypothyroidism, as well as with rare conditions, such as amyloidosis, acromegaly, and localized infection. A recent study found that 14% of the general population have symptoms suggestive of carpal tunnel syndrome; such symptoms were confirmed by clinical examination and electophysiologic [39] studies in 2% to 3% of the patients studied. In addition, 18% of asymptomatic people were found to have electrophysiologic evidence of median nerve entrapment. Carpal tunnel syndrome is more common in persons with occupations that require repetitive wrist movements, awkward wrist positions, or the use of vibrating tools or great force. Patients report numbness, tingling, and pain over the palmar radial aspect of the hand; these symptoms are often worse at night or after use. However, a recent review of published studies suggests that the pattern of pain and findings of decreased sensation [40] and weakness of thumb abduction are the most reliable diagnostic findings. Because of the uncertainties in the reliability of diagnostic findings, electrodiagnostic testing is usually necessary to confirm a diagnosis, particularly when surgical intervention is considered. Carpal tunnel syndrome involves the entrapment of the median nerve in the canal that encloses the nerve and several flexor tendons and that is formed by bones of the wrist and the transverse carpal ligament. Local [41] injection of glucocorticoids affords short-term relief in most patients, but long-term improvement is less predictable. Surgical decompression by sectioning of the volar carpal ligament results in excellent outcome in 67% to 80% of patients; it is indicated in patients whose conditions respond poorly to conservative therapy, patients with chronic or recurrent symptoms, or patients with weakness or atrophy of the thenar muscles. In a recent study, patients with poor upper extremity function, patients who used alcohol, or patients with worse mental health status were less likely to [42] have good results from surgical therapy. Dupuytren Contracture Dupuytren contracture is a fibrosing condition of the palmar and digital fascia that results in thickening and puckering of the palmar skin with subcutaneous nodules and often in flexion contracture of the underlying digit. Dupuytren contracture may be associated with other fibrosing syndromes, with an autosomal dominant inheritance pattern, and possibly with liver disease, epilepsy, and alcoholism. Although spontaneous improvement may be seen, surgical intervention to improve function may be useful in individual cases. Stiff-Hand Syndrome the stiff-hand syndrome, resembling scleroderma, is characterized by thickening of the skin and subcutaneous tissues and generalized limitation of hand and wrist motion. This condition is seen almost exclusively in young [43] patients with long-standing insulin-dependent diabetes mellitus. Hip Girdle Pain Pain around the hip girdle is a common complaint in clinical practice. Patients with pain resulting from diseases of the hip joint usually describe pain in the anterior thigh or inguinal region that worsens with weight bearing. More commonly, patients with a chief complaint of hip pain have a problem in one of the nonarticular structures of the hip girdle, usually located posteriorly or laterally [see Table 2]. Pain in the upper buttock in and around the gluteal muscles is often referred to as myofascial hip pain or gluteal bursitis. Local therapy with heat, stretching, or glucocorticoid injection is usually helpful, but many patients require long-term therapy. Patients typically complain of pain over the lateral aspect of the hip girdle, sometimes radiating down the thigh, that is worse at night when they lie on the affected side. Pain is sometimes present when the patient arises from a chair, but it tends to improve with ambulation. Point tenderness over the lateral or posterior aspect of the greater trochanter is usually diagnostic, though some patients with referred lumbar facet or disk disease may have a similar presentation. Patients with more severe pain may have a positive Trendelenburg sign on physical examination. In refractory cases, repeated injections, physical therapy, and, in rare instances, surgical excision of the bursa may be indicated. Ischiogluteal Bursitis Ischiogluteal bursitis results from an irritation of the bursa in the area of the attachments of the hamstring and gluteal muscles at the ischial tuberosity. The condition may be brought on by prolonged sitting or by pressure in the area and usually responds to local heat, stretching, or glucocorticoid injection. Iliopectineal Bursitis Iliopectineal bursitis, which is caused by irritation of the bursa between the iliopsoas muscle and the inguinal ligament, is an uncommon cause of inguinal pain and may mimic true hip joint disease. The diagnosis is suggested by the presence of inguinal pain that is aggravated by extension of the hip (in a patient whose hip x-ray is normal). Treatment is usually with local measures or, in rare cases, by means of surgical excision. Meralgia Paresthetica Meralgia paresthetica is characterized by intermittent paresthesia, hypoesthesia, or hyperesthesia over the upper anterolateral thigh. The syndrome is caused by an entrapment of the lateral femoral cutaneous nerve at the level of the anterosuperior iliac spine where the nerve passes through the lateral end of the inguinal ligament. Causes include local trauma, rapid weight gain, and the wearing of constrictive garments around the hips. Useful therapies include avoidance of pressure in the area, weight loss, and local infiltration of glucocorticoids at the level of nerve exit. Knee and Lower Leg Pain Clinically, it can be difficult to differentiate articular from nonarticular knee pain. Most patients with articular knee pain have a relatively diffuse pain that is not well localized to one area of the knee. Physical examination shows loss of motion, crepitus (in osteoarthritis), warmth (in inflammatory arthritis), or the presence of effusion. If knee pain is localized or if the knee has full range of motion without warmth, crepitus, or effusion, one of the following nonarticular syndromes should be considered: infrapatellar tendinitis, Osgood-Schlatter disease, prepatellar bursitis, anserine bursitis, anterior knee pain syndromes, and restless legs syndrome. Tenderness is localized to the infrapatellar tendon, with no associated swelling, and conservative measures almost always result in resolution of symptoms. Osgood-Schlatter Disease Osgood-Schlatter disease is characterized by pain and swelling over the tibial tubercle at the tendon insertion point. This condition is seen predominantly in adolescent males and is thought to represent a traumatic avulsion injury. Symptoms usually resolve with temporary immobilization and slow resumption of activities. An area of localized fluid collection is usually detectable; aspiration is often needed for diagnosis. As in olecranon bursitis of the elbow, prepatellar bursitis may be associated with trauma, localized bacterial infection, and, less commonly, gout, rheumatoid arthritis, and atypical infections. The differentiation between trauma and infection is particularly important for initiation of appropriate therapy. Anserine Bursitis Anserine bursitis, which is caused by irritation of the bursa near the attachment of the sartorius and hamstring muscles at the medial tibial condyle, is a common cause of medial knee pain. Patients with this condition complain of pain at night or when climbing stairs, and an area of localized tenderness can be found on examination. Coexistent osteoarthritis of the knee joint is present in many patients, and relief with local heat or injection of glucocorticoids and anesthetic may be helpful both diagnostically and therapeutically. Anterior Knee Pain Syndromes Anterior knee (patellofemoral) pain syndromes usually manifest themselves as pain and crepitus associated with [45] activities that require knee flexion under load conditions. Physical findings that help with diagnosis include (1) reproduction of pain with pressure over the patella during knee motion and (2) tenderness over the medial surface of the patella. The cause of most anterior knee pain syndromes is uncertain, but the pain may be related to misalignment of the quadriceps with lateral patellar subluxation, patella alta, hypermobility, or findings of chondromalacia of the patella on arthroscopic evaluation. Local measures and an exercise program that emphasizes isometric quadriceps strengthening is helpful in most patients. Some patients require arthroscopic intervention to diagnose and correct articular irregularities or patellar misalignment. Restless Legs Syndrome Restless legs syndrome is characterized by unpleasant, deep-seated paresthesia in both legs that usually occurrs [46] during rest and that is relieved by movement. Although idiopathic in most patients, restless legs syndrome has been associated with iron deficiency, uremia, pregnancy, diabetes, and polyneuropathies. However, some patients may require treatment with bromocriptine, carbamazepine, clonidine, benzodiazepines, or opioids. Ankle and Foot Pain Nonarticular foot and ankle pain is best approached with a consideration of the region affected: the forefoot, midfoot, or hindfoot [see Figure 3]. In the anterior foot, hallux valgus may cause diffuse pain, whereas Morton neuroma is usually localized. Plantar fasciitis and Achilles tendinitis are common causes of posterior foot pain. It is a common deformity that causes pain because of direct pressure over the first metatarsophalangeal joint resulting from footwear or because of pressure over the lateral toe joints caused by crowding of the toes. Initial treatment of these problems should begin with adequate footwear that allows ample width for the metatarsal heads, individualized orthoses, and surgical correction (reserved for patients with persistent pain). Morton neuroma is an entrapment neuropathy of the interdigital nerve, with or without an associated plantar neuroma, that is most commonly seen between the third and fourth metatarsal heads. Patients report pain and paresthesia radiating into the affected toes; tenderness between the metatarsal heads that reproduces the described symptoms will also be found. Orthoses to decrease pressure in the area, local glucocorticoid injection, or surgical excision of the neuroma may be needed to relieve symptoms. Midfoot Pain Midfoot pain is usually the result of deformities of the arch of the foot or arthritic changes of the midfoot joints.
Medial rectus where the isolated primary movement of each muscle is observed (elevation allergy shots cancer generic periactin 4mg without a prescription, depression allergy quiz questions buy discount periactin on line, abduction allergy shampoo for dogs discount generic periactin canada, or adduction) allergy symptoms cough periactin 4 mg amex, are shown in part D (also see Clinical Note) allergy testing hair sample buy generic periactin 4mg on-line. The image at the bottom of the facing page illustrates which muscle is being tested as this happens allergy testing nuts purchase periactin 4mg line. If weakness of a muscle is observed, then the physician must determine if it is a muscle problem and/or a nerve problem (damage to the nerve innervating the muscle). Plate 3-3 See Netter: Atlas of Human Anatomy, 6th Edition, Plates 85 and 86 Muscular System Extra-ocular Muscles 3 Trochlea (pulley) 1 1 2 3 4 1 7 5 Trochlea Common 2 pulley 6 tendinous ring A. Right lateral view 6 Lacrimal gland Periorbita 3 Fascial sheath of eyeball Periorbita 4 5 C. Frontal section Superior Inferior Superior rectus oblique rectus Lateral Medial Lateral rectus rectus rectus Inferior Superior Inferior D. The principal muscle of the tongue is the genioglossus, which blends with the intrinsic longitudinal muscle n 7. Musculus uvulae (uvular muscle) ounce, the genioglossus (and its intrinsic muscle component) is the strongest muscle in the body! The tongue and palate mus different color for each muscle: cles are summarized in the table below. Sagittal view Superior pharyngeal constrictor muscle 7 Basilar part of occipital bone Epiglottis B. Pharyngeal mucosa removed Levator veli palatini muscle (cut) 6 Epiglottis 5 Palatopharyngeal Choanae arch and muscle (cut) Pterygoid hamulus Superior Palatine tonsil (cut) pharyngeal Levator veli Palatoglossal arch constrictor palatini muscle (cut) and muscle (cut) muscle (cut) 8 Foramen cecum Terminal sulcus 7 Vallate papillae Foliate papillae C. This process of swallowing is called deglutition and involves the interplay and coordinated movements of the tongue, soft palate, pharynx, and larynx to work properly. Partially opened posterior view 3 Thyroid cartilage Choanae Trachea Esophagus Nasopharynx Nasal septum B. Lateral view Soft palate Uvula Oropharynx Root of tongue Epiglottis Larygeal inlet (aditus) Laryngopharynx Esophagus C. This action is important during swallowing but larynx, so these will be reviewed frst. The larynx lies at the C3 also adjusts the size of the vestibule during phonation to add to C6 vertebral level, just superior to the trachea, and consists quality to the sound. All of these intrinsic muscles are innervated of nine cartilages joined by ligaments and membranes. The vocal folds (vocal ligaments covered by mucosa) control phonation much like the reed instrument. Posterior crico-arytenoid: the only pair of muscles that abduct the vocal folds Cuneiform Paired cartilages in ary-epiglottic folds that have no articulations n 6. Arytenoid muscle: composed of transverse and oblique fbers, this muscle adducts the vocal folds and narrows the rima vestibuli n 7. Arytenoid Hoarseness can be due to any condition that results in improper vibration or coaptation of the vocal folds. Infammation and edema (swelling) are commonly the cause for hoarseness and the intrinsic muscles of the larynx act largely to adjust the can be induced by smoking, overuse of the voice, gastroesoph tension on the vocal cords (ligaments), opening or closing the ageal refux disease, cough, and infections. Surgical scarring, rima glottidis (space between the vocal cords) and opening and nodules or cysts, and cancer also may cause hoarseness. Posterior view 1 Hyoid bone Ary-epiglottic muscle Thyro-epiglottic muscle Lateral crico-arytenoid muscle 2 5 Thyro-arytenoid muscle 7 3 3 C. Right lateral view Lamina of cricoid cartilage Posterior crico-arytenoid muscle Arytenoid cartilage Arytenoid mm. Conus elasticus Cricothyroid muscle Vocal muscle Lamina of thyroid cartilage Vocal ligament E. Omohyoid sternocleidomastoid muscles, this triangle is not subdivided further Anterior, which is further subdivided into the triangles Clinical Note: listed below: the neck provides a conduit that connects the head to the n 2. The muscles, vessels, and visceral structures (trachea gland and esophagus) are all tightly bound within three fascial layers n 3. Infections or masses (tumors) in one or another of these tight spaces can compress n 4. Muscular: lies anteriorly in the neck below the hyoid softer structures and cause signifcant pain. The fascial lay bone ers themselves also can limit the spread of infection between n 5. On the labeled diagram of the neck in transverse section, color the three fascial layers to highlight their extent. The and invests the trapezius and sternocleidomastoid muscles key muscles are summarized in the table below. Lateral view Styloid process Mastoid process Mylohyoid muscle Stylohyoid muscle Digastric muscle Hyoid bone Digastric muscle (posterior belly) 9 (anterior belly) Thyrohyoid muscle Geniohyoid muscle 6 Sternohyoid muscle 7 Omohyoid muscle Omohyoid 10 (superior belly) muscle (inferior belly) Thyroid Sternothyroid muscle cartilage 10 Sternum Scapula 13 12 11 D. Infrahyoidal and suprahyoidal muscles and their actions Thyroid gland Pretracheal Retropharyngeal fascia space 13 Carotid sheath Investing fascia Trachea Clavicle C. Longus capitis (capitis refers to the head) the scalene muscles (anterior, middle, and posterior) that attach n 2. Longus colli (colli refers to the neck) to the upper ribs and also are accessory muscles of respiration. Anterior scalene (note that the subclavian vein passes They help raise the thoracic cage during deep inspiration. The anterior to this muscle) prevertebral muscles are summarized in the table below. Middle scalene (note that the subclavian artery passes between this muscle and the anterior scalene muscle) n 5. Infections and abscesses can gain access to this space and spread anywhere from the base of the skull to the upper portion of the thoracic cavity (superior medias tinum). Serratus posterior superior: intermediate group of n muscles; have respiratory function n 5. Intermediate muscles, just deep to the superfcial layer, are accessory muscles of respiration and have attachments to ribs. The trapezius and latissimus dorsi are removed from the right side of the plate so that you can see this group of muscles. The superfcial group migrates onto the back during development of the embryo, although they function as muscles of the upper limb. They participate in movement of the head and neck or to the semispinalis muscles) postural control of the vertebral column. Spinalis (erector spinae group, found most medially n superfcial (splenius muscles), intermediate (erector spinae), in the back) and deep layers (transversospinal). Rectus capitis posterior major (suboccipital region) permit movements of the spine, and are innervated by dorsal rami of spinal nerves. Plate 3-10 See Netter: Atlas of Human Anatomy, 6th Edition, Plates 172 and 173 Muscular System Deep (Intrinsic) Back Muscles 3 A. Deep layer (rightside deeper dissection) Semispinalis capitis muscle Semispinalis capitis muscle 1 Semispinalis Longus thoracis muscle Rotatores Brevis cervicis mm. Serratus posterior superior muscle Longus Rotatores Erector 2 Brevis thoracis spinae mm. Semispinalis capitis muscle Rectus capitis posterior minor muscle Splenius capitis muscle 5 7 6 Vertebral artery Posterior ramus of C1 Semispinalis capitis muscle Splenius capitis muscle Spinous process of C2 C. Functionally, the muscles of color for each muscle: the thoracic wall keep the intercostal spaces rigid, thereby pre n 1. External intercostals: outermost layer of the three venting them from bulging out during expiration or being sucked intercostal muscles; fbers run from superolateral to in during inspiration. The exact role of individual intercostal mus inferomedial cles on the movements of the ribs is diffcult to interpret despite n 2. Internal intercostals: middle layer of intercostals; many electromyographic studies. Innermost intercostals: fbers almost parallel those of On the anterior chest wall, the pectoralis major and minor the internal intercostals and may sometimes be fused muscles overlie the intercostal muscles, but these two muscles to this muscle really act on the upper limb and will be discussed later. Transversus thoracis tal intercostal nerves and vessels travel between the internal and innermost intercostal muscles, as seen in the cross section of the thoracic wall. Careful positioning of the needle or catheter is necessary to avoid impaling the intercostal nerve and vessels, which pass inferior to each rib in the costal groove. Plate 3-11 See Netter: Atlas of Human Anatomy, 6th Edition, Plates 187 and 188 Muscular System Thoracic Wall Muscles 3 First rib 1 Body of sternum Intercostal 2 neurovascular bundle 3 Lung Skin Rib 4 B. Anterior view Spinal (radicular, or segmental medullary) branch of posterior intercostal artery Intercostal nerve (ventral ramus of thoracic spinal nerve) Posterior intercostal artery Serratus Left Right anterior Aorta lung lung 3 Lateral cutaneous branch 2 Lateral cutaneous branch 1 Anterior branch of lateral cutaneous branch of intercostal nerve Anterior cutaneous branch of intercostal nerve Perforating branch Anterior intercostal arteries C. Work from the superfcial to the deeper layer and note found in the thoracic wall, where they lie between the ribs and the direction of the muscle fbers as your color: comprise the intercostal muscles. Internal abdominal oblique the functions of these anterior abdominal muscles include: n 3. The layers (lamina) that compose the sheath are defcient arcuate line internal abdominal oblique muscles below the arcuate line (in the lower quarter) of the rectus sheath, Posterior lamina Formed by fused aponeuroses of internal abdomi where only the transversalis fascia lies in contact with the rectus above arcuate line nal oblique and transversus abdominis muscles abdominis. Pyramidalis to a weakness of the wall, can occur on the anterior abdominal n wall. Use a color different from the the midline linea alba muscle colors, but note the relationship to the muscles. Aponeurosis transverse abdominis muscle region (where abdomen and thigh meet) Plate 3-12 See Netter: Atlas of Human Anatomy, 6th Edition, Plates 246 and 248 Muscular System Anterior Abdominal Wall Muscles 3 Right side: deeper dissection Intercostal muscles 4 2A 1 2 3 Tendinous 3A intersection 1A Linea alba Rectus sheath Inguinal ligament 5 Conjoint tendon Pubic tubercle A. Intermediate dissection 1A 2A 3A 4 Linea alba Skin Above arcuate line 1 2 Transversalis fascia Posterior layer 3 of rectus sheath 4 1A 2A 3A Skin Below arcuate line 1 2 Transversalis fascia 3 Peritoneum B. The inguinal canal itself is a small passageway through the However, the presence of the spermatic cord in the inguinal abdominal musculature that is demarcated at both ends by canal and the descent of the testis during fetal development inguinal rings, the deep ring opening in the abdomen and render this region clinically unique in males and predispose the superfcial ring opening externally just lateral to the pubic males to inguinal hernias. Each spermatic cord, using a different color for each feature: testis is tethered by its spermatic cord, which among other 1. Ductus deferens n structures contains the ductus (vas) deferens, which will provide n 2. External oblique muscle and aponeurosis a passageway for sperm to re-enter the body cavity and join with the prostatic urethra during sexual arousal. Transversus abdominis muscle As the spermatic cord runs in the inguinal canal, it picks up 5. Transversalis fascia n spermatic fascial layers derived from the abdominal wall struc n 6. Inguinal canal External oblique muscle Internal oblique muscle 2 Transversus abdominis muscle 3 Transversalis fascia 4 5 Testis Gubernaculum C. Fetal descent of testis Formation of processus vaginalis Testis descends along gubernaculum via inguinal canal, behind processus vaginalis 6 7 Gubernaculum Processus 8 vaginalis Gubernaculum D. Iliacus: this muscle and the psoas fuse to function as cage and line the abdominopelvic cavity to the level of the true one muscle, the iliopsoas pelvis. Often the abdominal diaphragm is included with these muscles, and its superior extent rises almost to the level of the the psoas minor muscle is not always present but does act as a 8th thoracic vertebral body. Relaxation of the diaphragm and the elastic recoil of the lungs expels the air during normal expiration. This infection can spread beneath the psoas fascial sheath that covers this muscle and even extend inferior to the inguinal ligament.
Order 4 mg periactin mastercard. Allergy Symptoms - Bee Stings.