Jeffrey David Clough, MD
- Assistant Professor of Medicine
- Core Faculty Member, Duke-Margolis Center for Health Policy
- Member in the Duke Clinical Research Institute
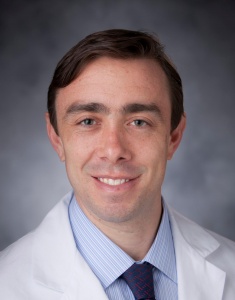
https://medicine.duke.edu/faculty/jeffrey-david-clough-md
Procure and maintain equipment for the prevention and treatment of pressure ulcers diabetes in dogs food recommendations order cheapest glucotrol xl and glucotrol xl. Evaluate and optimize psychosocial factors that often impair surgical wound healing diabetes japanese diet buy discount glucotrol xl on-line. Evaluate the individual for osteomyelitis if exposed bone is present diabetes quotes purchase 10mg glucotrol xl amex, the bone feels rough or soft can diabetes type 2 kill you cheap glucotrol xl 10mg with amex, or the ulcer has failed to heal with contemporary therapy blood sugar guidelines 10mg glucotrol xl with mastercard. Resect infected bone prior to or during surgical closure unless bone involvement is too extensive diabetic diet handout in spanish glucotrol xl 10mg without prescription. Intraoperative Recommendations During surgery, patients are immobile, positioned on a relatively hard surface, unable to feel the pain caused by pressure and shear forces, and are unable to change their position in order to relieve pressure. These factors increase the risk of pressure ulcer development in the intra-operative period. Excise the ulcer, including abnormal skin, granulation and necrotic tissue, sinus tracts, bursa and involved bone to the extent possible at surgical closure. When possible, choose a fap that will not violate adjacent fap territories to preserve all future options for fap coverage. Use a fap that is as large as possible, placing the suture line away from an area of direct pressure. Consider possible functional loss and rehabilitation needs, especially in ambulatory individuals. Transfer the individual from the operating table with adequate assistance to avoid disruption of the fap. Instead, lift the individual from the operating room table onto the bed rather than sliding or pulling. Select a high specifcation support surface that provides enhanced pressure redistribution, shear reduction, and microclimate control for individuals with who have undergone pressure ulcer surgery. Avoid transferring the post-surgical individual onto a non-high specifcation support surface unless clinically indicated. Avoid pressure, shear and friction in order to protect the blood supply to the fap. They should be used with extreme caution, as they create pressure on the pelvic fap. Position the individual on a pressure redistributing support surface when sitting out of bed. Confrm the presence of healthy lifestyle choices and a supportive social network prior to discharging the individual from a facility. Provide or facilitate access to pressure ulcer prevention education for the individual and his or her caregivers prior to discharge from the facility. Provide safe, respectful care and avoid injuries to both the individual and health professionals. Maximize workplace safety by implementing organization-wide bariatric management strategies that address manual handling techniques. Provide pressure redistribution support surfaces and equipment appropriate to the size and weight of the individual. Refer bariatric individuals to a registered dietitian or an interprofessional nutrition team for a comprehensive nutrition assessment and weight management plan. Ensure the individual is provided with a bed of appropriate size and weight capacity specifcations. Ensure that the bed surface area is suffciently wide to allow turning of the individual without contact with the side rails of the bed. Consider selecting a support surface with enhanced pressure redistribution, shear reduction and microclimate control for bariatric individuals. Use a pressure redistribution cushion designed for the bariatric individual on seated surfaces. Where appropriate, provide bariatric walkers, overhead trapezes on beds, and other devices to support continued mobility and independence. Use pillows or other positioning devices to offoad the pannus or other large skin folds and prevent skin-on-skin pressure. These recommendations are intended to supplement and not replace the general recommendations outlined in this guideline. Evaluate the need to change the pressure redistributing support surface for individuals with poor local and systemic oxygenation and perfusion to improve pressure redistribution, shear reduction, and microclimate control. Evaluate the need to change the support surface for individuals who cannot be turned for medical reasons, including a temporary oral-pharyngeal airway, spinal instability and hemodynamic instability. Consider slow, gradual turns allowing suffcient time for stabilization of hemodynamic and oxygenation status. Turning the individual more slowly or in small increments that allow adequate time for stabilization of vital signs should be considered when possible. Pillows placed under the full length of the calves to elevate heels may be appropriate for short-term use in alert and cooperative individuals. The knee should be in slight fexion to prevent obstruction of the popliteal vein and caution should be taken to place no pressure on the Achilles tendon. Assess critically ill individuals placed in the prone position for evidence of facial pressure ulcers with each rotation. Secure the individual with bolster pads (provided by the manufacturer) to prevent sacral shearing when lateral rotation features are selected for individuals without existing pressure ulcers. If indicated and consistent with medical needs, change to a support system with improved pressure redistribution, shear reduction, and microclimate control. Consider alternative methods of pressure redistribution (or avoid lateral rotation beds) in individuals with sacral or buttock pressure ulcers. Inspect the pressure ulcer and the periulcer skin for shear injury with every dressing change. Shear injury may appear as deterioration of the ulcer edge, undermining, and/or as increasing infammation of periulcer skin or the ulcer. Due to insuffcient evidence to support or refute the use of specifc additional nutrition interventions in critical care patients, specifc additional nutrition interventions are not recommended for routine use in this population. Ensure pressure ulcers are correctly differentiated from other skin injuries, particularly incontinence associated dermatitis or skin tears. Engage the family or legal guardian when establishing goals of care and validate their understanding of these goals. Educate the individual and his or her signifcant others regarding skin changes in aging and at end of life. Use a barrier product to protect aged skin from exposure to excessive moisture in order to reduce the risk of pressure damage. Select atraumatic wound dressings to prevent and treat pressure ulcers in order to reduce further injury to frail older skin. Exercise caution in position selection and manual handling technique when repositioning the older adult. Frequently reposition the head of older adults who are sedated, ventilated or immobile. Ensure that medical devices are correctly sized and ft appropriately to avoid excessive pressure. Use a high specifcation reactive or alternating pressure support surface on the operating table for all individuals identifed as being at risk of pressure ulcer development. Position the individual in such a way as to reduce the risk of pressure ulcer development during surgery. Do not position the individual directly on a medical device unless it cannot be avoided. Use heel suspension devices that elevate and offoad the heel completely in such a way as to distribute the weight of the leg along the calf without placing pressure on the Achilles tendon. Place the individual on a high specifcation reactive or alternating pressure support surface both prior to and after surgery. Position the individual in a different posture preoperatively and postoperatively than the posture adopted during surgery. The goals of palliative wound care are comfort for the individual and limiting the impact of the wound on quality of life, without the overt intent of healing. Consider using the Marie Curie Centre Hunters Hill Risk Assessment Tool, specifc to adult individuals in palliative care. Pre-medicate the individual 20 to 30 minutes prior to a scheduled position change for individuals who experience signifcant pain on movement. Consider changing the support surface to improve pressure redistribution and comfort. Strive to reposition an individual receiving palliative care at least every 4 hours on a pressure redistributing mattress such as viscoelastic foam, or every 2 hours on a regular mattress. Document turning and repositioning, as well as the factors infuencing these decisions. Adequate nutritional support is often not attainable when the individual is unable or refuses to eat, based on certain disease states. As such, the goal of care may be to maintain or improve the status of the pressure ulcer rather than heal it. Assess the impact of the pressure ulcer on quality of life for the individual and his/her signifcant others. Set a goal to enhance quality of life, even if the pressure ulcer cannot be healed or treatment does not lead to closure/healing. Assess the individual initially and at any change in their condition to re-evaluate the plan of care. Assess the pressure ulcer initially and with each dressing change, but at least weekly (unless death is imminent), and document fndings. Monitor the pressure ulcer in order to continue to meet the goals of comfort and reduction in wound pain, addressing wound symptoms that impact quality of life such as malodor and exudate. Consider use of topical metronidazole to effectively control pressure ulcer odor associated with anaerobic bacteria and protozoal infections. Assess psychosocial resources initially and at routine periods thereafter (psychosocial consultation, social work, etc. Educate the individual and his or her signifcant others regarding skin changes at end of life. Of particular relevance to children is the guideline section Medical Device related Pressure Ulcers. An exception is the chapter Nutrition in Prevention and Treatment, which provides recommendations for nutritional intake for adult populations, based on research conducted in adults. Consider using a reliable and valid pediatric pressure ulcer risk assessment tool to facilitate a structured assessment. Conduct and document a skin assessment at least daily and after procedures for changes related to pressure, friction, shear, moisture. Inspect the skin under and around medical devices at least twice daily for the signs of pressure related injury on the surrounding tissue. Regularly reassess the nutritional requirements of critically ill neonates and children who have, or are at risk of, a pressure ulcer. Develop an individualized nutrition care plan for neonates and children with, or at risk of, a pressure ulcer. When oral intake is inadequate, consider age appropriate nutritional supplements for neonates and children who are at risk of a pressure ulcer and are identifed as being at risk of malnutrition. When oral intake is inadequate, consider age appropriate nutritional supplements for neonates and children who have an existing pressure ulcer and are identifed as being at risk of malnutrition. When oral intake is inadequate, consider enteral or parenteral nutritional support in neonates and children who are at risk of a pressure ulcer or have an existing pressure ulcer and who are also identifed as being at risk of malnutrition. Select an age appropriate, high specifcation support surface for children at high risk of pressure ulcers. When selecting a pressure redistribution support surface for children, consideration should be given to the specifc bony prominences most at risk.
The physical findings in common conditions of the lumbar spine are summarized in Table 9-2 diabetes insipidus findings buy glucotrol xl 10 mg on-line. Spondylolysis Lumbar tenderness at the level of involvement (variable) Decreased lumbar lordosis (variable) nonorganic pathology or organic symptoms that are Hamstring tightness with straight-leg raising test being enhanced by nonorganic factors diabetes organizations proven glucotrol xl 10mg. Pain exacerbated by hyperextension of the lumbar spine (passive extension diabetes type 2 zwangerschap order 10mg glucotrol xl visa, active extension early signs diabetes feet buy cheap glucotrol xl line, single leg extension test) (frequent) Signs of associated spondylolisthesis joslin diabetes diet guidelines generic glucotrol xl 10 mg online, if present Examination of Other Areas and Systems Spondylolisthesis Pain due to lumbar spine pathology frequently radiates to Signs of spondylolysis (see above) the pelvis blood glucose to a1c discount glucotrol xl 10mg on-line, the posterior hip, or the thigh. In the case of Visible or palpable lumbar step-off (more severe cases) Sciatic notch tenderness (variable) lumbar disk disease, back pain may sometimes be com Motor or sensory deficit (variable) pletely absent, with the patient sensing pain only in the Lumbar Fracture sciatic notch and the posterior thigh areas. Patients with Tenderness at the level of injury this clinical picture often believe that they have a painful Localized swelling and hematoma or ecchymosis hip joint or a hamstring strain. Complete investigation of Lower motor neuron deficit owing to injury to the cauda equina or the potential lumbar spine pathology, therefore, often nerve roots (variable) Upper motor neuron deficit if lesion above the level of the cauda includes evaluation of the sacroiliac joint, the sacrum equina and the pelvis, the hip joint, and the thigh. The details of Lumbar Spondylosis these related examinations are described in Chapter 5, Decreased range of motion Pelvis, Hip, and Thigh. Pain exacerbated by motion (variable) Localized or diffuse tenderness (variable) Because the symptoms of claudication due to periph Low-Back Strain eral vascular disease are similar to those of pseudoclaudi Paraspinous muscle tenderness cation associated with spinal stenosis, an examination of Paraspinous muscle spasm (variable) the peripheral circulation of the lower extremities is Symptoms exacerbated by forward flexion List (variable) often a necessary adjunct to the lumbar spine examina Normal neurologic examination tion. Lumbar spine examination should include careful 1 loppenfeld S, ed: Physical Examination of the Spine and Extremities, New York, Appleton-Century-Crofts, 1976. Glossary 367 opposition A complex motion of the thumb in which the pelvic rotation Rotation of the pelvis in the coronal or trans thumb abducts and rotates (pronates) at the basilar joint, so verse planes during gait. Q angle, quadriceps angle the angle formed between a line pelvic flexion Rotation of the pelvis around a transverse axis in from the anterior superior iliac spine to the center of the which the superior pelvis rotates posteriorly while the infe patella and a line from the center of the patella to the center rior pelvis rotates anteriorly of the tibial tubercle when the patient is standing with the feet pelvic obliquity the situation in which the two sides of the in a neutral position. Index Note: Page numbers in italics refer to illustrations; page numbers followed by "t" refer to tables. A Adductor longus muscle, 165, 168, 170, Ankylosing spondylitis, 188, 301, 302, Abdomen, pathology of, back pain in, 360 171, 190 307, 339 Abdominal muscle reflexes, testing of, 325 Adductor magnus muscle, 168, 170, 190 Antalgic gait, 267-268, 339 325-326 Adductor pollicis muscle, 143 Antecubital fossa, 69 Abduction, definition of, 8, 9 Adductor tubercle, 168 Anterior, definition of, 1 of hip, 181 Adductors, humeral, testing of, 41-43, 43, 44 Anterior compartment muscles, 251 in extension, 181-182, 182 of fingers, 141 Anterior compartment syndrome, exercise in flexion, 182-183, 183 of hip. See also Osteoarthritis; shoulder, 20, 21 ligaments of, stability testing of, 290-292 Rheumatoid arthritis. See Rotator cuff, laxity of, abnormal, 14 windswept deformity of, 212 impingement syndrome of. See Collateral foot, and ankle, 247-296 extension of, 342, 342, 345-349, 347 ligament, ulnar. Roos test, 6l, 63 Sartorius muscle, 161, 168, 170, 187, 191 motion(s) of, 8, 9 Rostral, definition of, 3 Scalene muscles, 312 in deficient forearm rotation, 80, 81 Rotation, external, 8 Scaphoid bone, 109, 133 sliding out of joint, complaints of, 51t internal, 8 fracture of, 125t voluntary dislocation of, 56-58, 60 of hip, assessment of, 183-185, 184, 185 tubercle of, 135 Shoulder and upper arm, 17-67 of lumbar spine, 343, 344 Scaphoid shift test, 151-152, 152 alignment of, 27-28, 28 of shoulder and upper arm, external, at Scaphoid shuck test, 152, 152 anatomy of, 17 side, 30-32, 32 Scapholunate capitate joint, 133 anterior aspect of, palpation of, 35-39 in 900 abduction, 31-32, 33 Scapholunate ligament, injury of, 125t conditions of, physical findings in, internal, at side, 32, 34 injury to , test of, 151-152, 152 62-63, 64t in 900 abduction, 32, 33 instability of, 157t lateral aspect of, palpation of, 39, 40 passive, of shoulder and upper arm, 49, 52 Scaphotrapeziotrapezoid joint, 133 surface anatomy of, 22, 23 Rotation lag sign, external, 46, 48 Scapula, and snapping scapula syndrome, manipulation of, 40-63 Rotation simulation maneuver, of spinal 34, 40, 40 medial aspect of, palpation of, 40 nerves, 332, 332 inspection of, 22-25, 24 surface anatomy of, 27, 28 Rotational alignment, 3 lateral border of, 24, 25 motion in, 8, 9 Rotational malalignment, of lower limbs, 168 medial border of, 25, 25, 26 muscle testing of, 40-44 Rotator cuff, disorders of, in subscapulars palpation of, 39-40 normal, 27 injury, 47-49, 49 protraction of. See also Cervical spine; Lumbar spine; Superficialis tendon, laceration of, Tennis leg, 282-283 Thoracic spine. Splayfoot, 261 inspection of, 25-26, 26 326-328, 329 Splenitis capitis muscles, 299, 309 testing of, 41, 43 ulnar nerve dominant variation of, Splenitis cervicus muscles, 299 Supscapularis liltolf test, 41 328-330, 329-330 Spondylitic myelopathy, cervical, physical Sural nerve, 283, 290, 291 Tensor fascia lata, 163. See Elbow; Forearm; Hand; first metacarpal of, fractures of, 133 Torsion, definition of, 3 Shoulder and upper arm; Wrist. They have been carefully researched and are continually updated in order to be consistent with the most current evidence-based guidelines and recommendations for the provision of musculoskeletal management services from national and international medical societies and evidence-based medicine research centers. In addition, the criteria are supplemented by information published in peer reviewed literature. Health Plan medical policy supersedes the eviCore criteria when there is conflict with the eviCore criteria and the health plan medical policy. For that reason, we have peer reviewers available to assist you should you have specific questions about a procedure. Treatment may include active and passive modalities using a variety of means and techniques, based upon biomechanical and neurophysiologic principles. Treatment should be directed toward restoration or compensation for lost function. Services that do not require the performance or supervision of a qualified clinician are not skilled and are not considered reasonable or necessary therapy services, even if they are performed or supervised by a qualified professional. Coverage Criteria for Providers Several provider specialties utilize various approaches to achieve therapeutic benefit in the treatment of neuromusculoskeletal conditions. Services Not Covered Physical Therapy services will not be covered when provided by athletic trainers, and other providers not recognized by the Health Plan. Care Classifications Therapeutic Care Therapeutic care is care provided to relieve the functional loss associated with an injury or condition and is necessary to return the patient to the functioning level required to perform their activities of daily living, instrumental activities of daily living and work activities. Typically, it follows an acute injury or exacerbation, 7 of 937 and can extend up to three months from onset. Supportive Care Supportive care is that phase of care that occurs following the corrective or rehabilitative phase. Treatment is directed towards management of ongoing, unresolved symptoms that may or may not impact functional status. The therapeutic goal of this phase is patient/caregiver education, self-management, and to prevent deterioration of physical or functional status. Means and methods include progression of exercise and continued patient education. Palliative Care (Noncovered Service) Palliative care is typically given to alleviate symptoms and does not provide corrective benefit to the condition treated. Habilitation: Physical, occupational and speech therapy services provided in order for a person to attain and maintain a skill or function for daily living, that was never learned or acquired and is due to a disabling condition such as developmental delay, developmental disability, developmental speech or language disorder, developmental coordination disorder and mixed developmental disorder. Severity is determined by several factors including, but not limited to , mode of onset, duration of care, loss of work days, and functional deficits. Conditions Severity Criteria Table Criteria Mild Moderate Severe Condition Condition Condition Mode of onset Variable Variable Severe Anticipated duration of care 1-6 weeks 6-10 weeks 10 or more weeks Loss of work days No loss of 0-4 days of work 5 or more days of work days lost work lost Work restriction None Possible, Restriction, depends on depending on occupation; 0-2 occupation; 2 or weeks more weeks Functional deficits: Mild/no Mild to moderate Considerable loss 1. Contract limitations for physical therapy services will determine the available benefit if such therapy is determined to be medically necessary. Physical therapy services must be ordered by a physician (exception in direct access states). Therapy requires the judgment, knowledge and skills of a qualified provider of physical therapy services due to the complexity and sophistication of the therapy and the physical condition of the patient. The patient must have functional deficits that interfere with Activities of Daily Living or return to work (see definitions at the end of policy) Refer to the Evidence-based Guidelines, Admission Criteria, for information on specific functional losses for specific conditions. In keeping with professional standards, this home management program should be introduced into the course of treatment at the earliest appropriate time; (This may also be applicable to parents, guardians, or caregivers of pediatric patients and adult patients needing assistance. Refer to the Evidence-based Guidelines for a review of specific conditions and their course of recovery. Services do not duplicate those provided concurrently by any other therapy, particularly occupational therapy. T hey must have separate treatment plans and goals with treatment occurring in separate treatment sessions and visits. Rehabilitative Physical Therapy Services Are Generally Not Considered Medically Necessary Under the Following Circumstances 1. Therapeutic care is care provided to relieve the functional loss associated with an injury or condition and is necessary to return the patient to the functioning level required to perform their activities of daily living, instrumental activities of daily living 11 of 937 and work activities. Maintenance care when palliative procedures are performed that are repetitive or to reinforce previously learned skills or when services performed are related to activities for the good and welfare of member such as a fitness program. Satisfactory motor ability of the impaired or injured part(s) such that further improvement can be accomplished with a self-management program. When there is no documented continual progression of function or improvement over the course of treatment, or a negative trend occurs. Physical therapy services are not considered medically necessary for pain mediation alone. Unskilled Care: Unskilled services are palliative procedures that are repetitive or reinforce previously learned skills 12 of 937 They are not covered because they do not involve complex and sophisticated therapy procedures, or require the judgment and skill of a qualified therapist for safety and effectiveness. Eating, bathing, dressing, toileting and moving from one place to another are some examples. Instrumental Activities of Daily Living:A ctivities that are often performed by a person who is living independently in a community setting during the course of a normal day, such as managing money, shopping, telephone use, travel in the community, housekeeping, preparing meals, and taking medications correctly. Dutton, Mark, Orthopaedic Examination, Evaluation, & Intervention, McGraw-Hill Medial Publishing Division, 2004 20. The Practical Guide to Range of Motion Assessment American Medical Association, 2002 21. Guide to Physical Therapist Practice, Interactive Guide to Physical Therapist Practice, Version 1. Evidence-based practice: Belief, attitudes, knowledge and behaviors of physical therapists. American Academy of Orthopedic Surgeons and American Academy of Pediatrics, 1997 15 of 937 36. T hese services emphasize useful and purposeful activities to improve neuromusculoskeletal and cognitive functions, and to teach adaptive skills to accomplish the activities of daily living. Other occupational therapy services include guidance in the selection and use of adaptive equipment. Medically Necessary Services To be considered reasonable and necessary the following conditions must each be met: Services are for the treatment of a covered injury, illness or disease, and are appropriate treatment for the condition Treatments are expected to result in significant, functional improvement in a reasonable and generally predictable period of time, or are necessary for the establishment of a safe and effective maintenance program. T reatment should be directed toward restoration or compensation for lost function. Services that do not require the performance or supervision of a therapist are not skilled and are not considered reasonable or necessary therapy services, even if they are performed or supervised by a qualified professional. Services Not Covered Occupational Therapy services will not be covered when provided by athletic trainers, and other providers not recognized by Landmark Healthcare or provided beyond the scope of his or her license. A patient receiving palliative care, in most instances, demonstrates varying lapses between treatments. If an exacerbation of a condition occurs, care becomes therapeutic rather than palliative, and documentation of the necessity for care. Conditions Severity Criteria Table Criteria Mild Moderate Severe Condition Condition Condition Mode of onset Variable Variable Severe Anticipated duration of care 1-6 weeks 6-10 weeks 10 or more weeks Loss of work days No loss of 0-4 days of work 5 or more days of work days lost work lost Work restriction None Possible, Restriction, depends on depending on occupation; 0-2 occupation; 2 or weeks more weeks Functional deficits: Mild/no loss Mild to moderate Considerable loss 20 of 937 1. Contract limitations for occupational therapy services will determine the available benefit if such therapy is determined to be medically necessary. Therapy requires the judgment, knowledge and skills of a qualified provider of occupational therapy services due to the complexity and sophistication of the therapy and the physical condition of the patient. Refer to the Evidence Based Guidelines for a review of specific conditions and their course of recovery. Such terminology includes objective measurements for ranges of motion, motor ability, and levels of function. When a patient receives both occupational and physical or speech therapy, the therapies should provide different interventions and not duplicate the same treatment. Training in nonessential self-help or recreational tasks such as: Homemaking, gardening, educational activities and driving, return to sport or recreational activities. This is particularly applicable to patients with chronic, stable conditions where skilled supervision/interventions are no longer required and further clinical improvement cannot reasonably be expected from continuous ongoing care. This includes but is not limited to: Therapy that is supportive rather than corrective in nature Therapy that is intended to maintain a gradual process of healing, or to prevent deterioration or relapse Ongoing treatment solely to improve endurance, strength, or distance Passive exercises to maintain range of motion that can be carried out by non skilled persons A general exercise program to promote overall fitness Treatment that is intended to provide diversion or general motivation Treatment that seeks to prevent disease, promote health, and prolong and enhance quality of life 3. Ongoing or prolonged treatment for chronic conditions and/or chronic pain is not considered medically necessary in the absence of measurable improvement that is sustained from treatment visit to treatment visit. T herapy is also not covered when the condition is not expected to improve significantly within a reasonable time period. The intensity or frequency of care should not exceed the number of visits necessary for a clinician to provide skilled care. Group exercise/ therapy programs defined as the simultaneous treatment of two or more patients who may or may not be doing the same activities is not a covered benefit. Occupational therapy is not covered when the member suffers a temporary loss or reduction of function and could reasonably be expected to improve spontaneously without the services of an occupational therapist. Collaboration with other agency or professional personnel or with other community resources 11. For additional therapy requests to be considered medically necessary, they must include documented objective, measurable clinical data demonstrating the need for continued treatment. Occupational therapy services are not considered medically necessary for pain mediation alone. The Practical Guide to Range of Motion Assessment American Medical Association, 2002 26 of 937 21. American Academy of Orthopedic Surgeons and American Academy of Pediatrics, 1997 36. What factors explain the number of physical therapy treatment sessions in patients referred with low back pain; a multilevel analysis.
Purchase glucotrol xl with visa. Comment trouver le coeur de votre bébé avec un doppler ?.
It is generally accepted that pain after inguinal surgery (hernia) is a consequence of damage to the nerves inside the spermatic cord (4) blood glucose safe zone cheap 10mg glucotrol xl with mastercard. This is based on the anatomical knowledge that all nerves involved in testicular pain merge in the spermatic cord (5) blood sugar 450 purchase glucotrol xl on line. The pudendal nerve supplies the skin of the perineum and the posterior side of the scrotum diabetes quinoa discount 10mg glucotrol xl with mastercard. Postvasectomy scrotal pain syndrome is often associated with negative cognitive diabetes diet and watermelon glucotrol xl 10 mg lowest price, behavioural diabetes response dogs order genuine glucotrol xl on-line, sexual or emotional consequences managing your diabetes basics and beyond order discount glucotrol xl on-line, as well as with symptoms suggestive of lower urinary tract and sexual dysfunction. This may lead to congestion in the epididymis which in turn gives rise to pain because of dilatation of hollow structures (6). Incidence of post-vasectomy pain is 2-20% among all men who have undergone a vasectomy (7). In a large cohort study of 625 men, the likelihood of scrotal pain after 6 months was 14. The risk of scrotal pain was significantly lower in the no-scalpel vasectomy group, at 11. An international working group has set up guidelines for prevention and management of postoperative chronic pain following inguinal hernia surgery. They have stated that the most important way of preventing pain is to identify and preserve all three inguinal nerves (10). Chronic scrotal pain is a complication of hernia repair, but in trials, it is seldom reported or it is put under the term chronic pain (not specified). In almost all studies, the frequency of scrotal pain was significantly higher in the laparoscopic than in the open group (4, 11-13). In one particular study, there was no difference at 1 year but after 5 years, the open group had far fewer patients with scrotal pain (14). The best known referred pain is of myofascial origin, especially the trigger points (see Chapter 9). Problems inside the bladder or abdominal cavity can also give rise to pain in the scrotal area. When making a treatment plan for patients with scrotal pain, it is important to remember this phenomenon. Gentle palpation of each component of the scrotum is performed to search for masses and painful spots. A rectal examination is done to look for prostate abnormalities and to examine the pelvic floor muscles. In > 80% of patients, ultrasound does not show abnormalities that have clinical implications (15, 16). If physical examination is normal, ultrasound can be performed to reassure the patient that there is no pathology that needs therapy (mainly surgery). Ultrasound can be used to diagnose hydroceles, spermatoceles, cysts and varicoceles. When abnormalities such as cysts are seen, this may play a role in therapeutic decision making. In general practice, it seems that many urologists are performing ultrasound examination in almost all patients. It is becoming increasingly clear that advances in the non-surgical management of testicular pain are mainly based on the emergence of pain relief as a specialty. Knowing this, it seems obvious that referring to a multidisciplinary pain team or pain centre should be considered in an early phase of the consultation (18). The pelvic floor muscles should be tested and will often be found overactive, which means that they contract when relaxation is needed. More specific myofascial trigger points are found in the pelvic floor, but also in the lower abdominal musculature. Treatment consists of applying pressure to the trigger point and stretching the muscle (22, 23) (see Chapter 9). In the literature, there is consensus on postponing surgery until there is no other option. All the studies that have been done were cohort studies but their success rates were high. The size of effect was so remarkable that it is recommended that randomised studies are performed to obtain better proof. The three cohort studies that are found were consistent in the indication criteria, the diagnostic methods applied, and the surgical approach used. They included patients with chronic scrotal pain who did not respond to conservative treatment. Ultrasound showed no abnormalities and a spermatic cord block showed pain relief of > 50%. The cord is transected in such a way that all identifiable arterial structures, including testicular, cremasteric, deferential arteries and lymphatic vessels are left intact. The complication of testicular atrophy was seen in 3-7% of the operated patients (24-26). The laparoscopic route for denervation seems feasible but the results are unclear (27). Epididymectomy shows the best results in patients with pain after vasectomy, or pain on palpation of the epididymis and when ultrasound shows multiple cysts. These results are also from cohort studies but the fact that assessment can help in predicting the chance of success makes further studies worthwhile. One study in our search has yielded different results, namely, that post-vasectomy patients fared worse and that ultrasound did not help in predicting the result of the operation. There have been no studies than can help in making a rational decision on whether to perform orchiectomy. Some studies have shown good results but the quality of these studies was limited. A We recommend informing about the risk of post-vasectomy pain when counselling patients planned A for vasectomy. To reduce the risk of scrotal pain, we recommend open instead of laparoscopic inguinal hernia repair. A We recommend that during inguinal hernia repair all the nerves in the spermatic cord are identified. A For patients who are treated surgically, we recommend microsurgical denervation of the spermatic A cord. For patients who do not benefit from denervation we recommend to perform epididymectomy. C figure 8: assessment and treatment algorithm for scrotal pain syndrome Assessment Treatment Semen culture General treatment options for chronic pelvic pain chapter 10 Grade A recommended Microsurgical denervation of the spermatic cord Uroflowmetry Inform patients undergoing vasectomy about the risk of pain Ultrasound scrotum (see text) For surgeons: open hernia repair yields less scrotal pain Pelvic floor muscle For surgeons: identify all nerves during hernia repair testing Phenotyping Epididymectomy, in case patient did not benefit from denervation Grade B recommended Orchiectomy is a last resort option, when everything else has failed Other comments Ultrasound has no clinical implications on the further treatment although physicians tend to still use ultrasound to reassure the patient 3. Anatomic variability of the ilioinguinal and genitofemoral nerve:implications for the treatment of groin pain. Chronic pain 5 years after randomized comparison of laparoscopic and Lichtenstein inguinal hernia repair. A review of the efficacy of surgical treatment for andpathological changes in patients with chronic scrotal pain. International guidelines for prevention and management of post-operative chronic pain following inguinal hernia surgery. Laparoscopic extraperitoneal inguinal hernia repair versus open mesh repair: a prospective randomized controlled trialSurgery 5: 464-72. Five-year follow-up of patients undergoing laparoscopic or open groin hernia repair: A randomized controlled trial. Laparoscopic extraperitoneal inguinal hernia repair versus open mesh repair: long-term follow-up of a randomized controlled trial. Five-year follow-up of a randomized trial to assess pain and numbness after laparoscopic or open repair of groin hernia. Value of diagnostic ultrasound in patients with chronicscrotal pain and normal findings on clinical examination. Pelvic floor electromyography in men with chronic pelvic painsyndrome: a case-control study. A prospective, randomized, placebo controlled, double-blind studyof pelvic electromagnetic therapy for the treatment of chronic pelvic pain syndrome with 1 year offollowup. Integration of myofascial trigger point release and paradoxicalrelaxation training treatment of chronic pelvic pain in men. Myofascial dysfunction associated with chronic pelvic floor pain: management strategies. Microsurgical denervation of the spermatic cord for chronic orchialgia: long term results from a single center. Microsurgical denervation of the spermatic cord as primary surgical treatment of chronic orchialgia. Vasectomy reversal for the post-vasectomy pain syndrome: aclinical and histological evaluation. Urethral pain syndrome is often associated with negative cognitive, behavioural, sexual or emotional consequences, as well as with symptoms suggestive of lower urinary tract, sexual, bowel or gynaecological dysfunction. The intimate relation of the urethra with the bladder (both covered with urothelium) makes it plausible that pathology seen in the bladder is also found in the urethra and causes the same symptoms. It is obvious that what might cause pain in the bladder could be responsible for urethral pain. This means that the specific testing with potassium is used to support the theory of epithelial leakage (1, 2). Another possible mechanism is the neuropathic hypersensitivity following urinary tract infection (3). Symptoms recorded in patients with urethral pain syndrome can also be classified as referred pain from other organs or from the myofascial system. In a small group of patients with urethral pain, it has been found that grand multiparity and delivery without episiotomy were more often seen in patients with urethral syndrome, using univariate analysis (4). One trial comparing two forms of laser reported good results, but did not compare with sham treatment (6). The majority of publications on treatment of urethral pain syndrome have come from psychologists. Thirteen women were randomly selected for psychotherapy, but the method was not blind or free of possible bias. Psychotherapy was 12-16 weekly 1-h sessions, with additional fortnightly group discussion, and focused on associations between urinary symptoms and emotion. Assessment of symptoms at 6 months and four years after the end of treatment (with loss of two patients from each arm) showed substantial improvement in total urinary symptoms and additionally in pelvic pain, with 9/11 psychotherapy patients with normal levels of urinary function at 6 months, and 8/11 with normal levels at 4 years. The trial had significant weaknesses; in particular, the non-blind assignment to treatment condition, the non-standardised measures, and, for the purposes of this review, the combination of all urinary symptoms so that treatment effects on pain were obscured. The authors have noted that the lack of any credible intervention with controls makes it difficult to conclude that it was the particular treatment, rather than the general provision of treatment, which brought about recorded improvement. However, the results can be taken as encouraging the trial of psychological methods, using orthodox outcome measures and more rigorous methodology. Recommendations gR We recommend to start with general treatment options for chronic pelvic pain (see chapter 10). A We recommend that patients with urethral pain syndrome are treated in a multidisciplinary and B multimodal programme. When patients are distressed, we recommend referring them for pain-relevant psychological B treatment to improve function and quality of life. Intravesical potassium sensitivity in patients with interstitialcystitis and urethral syndrome. The role of a leaky epithelium and potassium in the generation of bladder symptoms in interstitial cystitis/overactive bladder, urethral syndrome, prostatitis and gynaecological chronic pelvic pain. The aim is to try and determine a remediable cause and treat it using the most effective available therapy. However, in 30% of cases, no cause is ever determined and this presents a therapeutic challenge to the attendant physician (1). The nature, frequency and site of the pain, and its relationship to precipitating factors and the menstrual cycle, may provide vital clues to the aetiology. A detailed menstrual and sexual history, including any history of sexually transmitted diseases and vaginal discharge is mandatory. Clinical pelvic examination should be a single digit examination if possible, but in most cases a gentle double digit examination is tolerable and sometimes necessary. The usual bimanual examination can generate severe pain so the examiner must proceed with caution. The degree of tenderness of the muscles and on the perineum (perineal body, levators and obturator internus) should be determined. Pelvic imaging, using ultrasound scanning or magnetic resonance, can provide useful information about pelvic anatomy and pathology. Any areas of tenderness detected can provide information related to the possible presence of current or pre-existing visceral disease (2, 3). Often it is combined with cystoscopy (7, 8) and/or proctoscopy to help identify the site of multi-compartment pain. Psychological considerations around laparoscopy There have been three diverse studies of laparoscopy. Improvement was related to beliefs about pain and its meaning in terms of serious disease, and not to medical variables (9). In another study, showing women a photograph of their pelvic contents taken during laparoscopy during post-laparoscopy feedback did not improve pain ratings or beliefs about pain more than feedback without a photograph (10).
In con clusion diabetes 7 day meal plan purchase line glucotrol xl, the vast majority of patients in cancer and Anticonvulsants palliative care may be treated well with opioids with They reduce neuronal excitability and suppress par out the use of transdermal systems (which are also oxysmal discharge of the neurons by stabilizing neu considerably more expensive! As mentioned above type 2 diabetes diet uk purchase glucotrol xl 10 mg online, earlier tolerance to the nau are indicated above all for continuous burning pain diabetes mellitus results in generic 10mg glucotrol xl with amex, seating side eects of opioids will then develop diabetic diet for kids cheap 10 mg glucotrol xl visa. The latter seem to have a synergistic eect no eective adjuvant medication to counteract it blood sugar home test order glucotrol xl on line. In carbamaze Antidepressants induce analgesia by increasing pine and oxcarbazepine diabetes 60 buy glucotrol xl in india, regular blood tests. Additionally, antidepressants elevation of liver enzymes, idiosyncratic drug reactions, modulate the opioid system in the central nervous sys and hyponatremia. Some side eects can be used for the benet of the a non-immunological hypersensitivity to a substance, patient, such as the sedating eect of amitriptyline for without any connection to pharmacological toxicity. If the patient is in an advanced stage of syncratic reaction, if liver transaminases are above ca. Elderly patients should not be medicated with Antidepressants tricyclic antidepressants because of multiple drug inter Antidepressants were the rst coanalgesics used after actions and an increased rate of falls. For all other pa it was found that they eectively reduced pain in poly tients it has to be remembered that the analgesic eect neuropathy, even in patients who were not depressed. Furthermore, antidepressants are also useful in treating The most frequent side eects are due to the tension type headache and as a prophylactic treatment anticholinergic properties of antidepressants (mostly of in migraine headache. Contrary to common belief, there the tricyclic class) via the muscarinic receptors. Explain to patients that they are receiving the the best evidence exists for amitriptyline, all tricyclic medication for pain, since they might read the package antidepressants are considered equally eective. Drug Proles, Doses, and Side Eects 357 Because tricyclic antidepressants may impair the problem). Always identify and treat the underlying liver function, it is advisable to check the liver enzymes cause along with giving symptomatic treatment with regularly. In advanced cancer patients, delirium may irregularities and polytope extrasystoles. Neuroleptics (like benzodiazepines) have no an Steroids algesic ecacy and therefore should never be used for Steroids are widely used in cancer pain therapy, es the indication of pain. Pain needs analgesics and not se pecially in patients with an advanced stage of disease. Because of their anti-inammatory eects, Terefore, they have direct eects on opioid-induced steroids may be also used in chronic inammatory dis nausea and are very valuable antiemetics (a dose of 0. They all have a low neuroleptic po scheme, but in acute pain exacerbation because of mas tency, but a good sedating eect, and therefore may be sive cancer progression, a common approach would be used as sleeping pills in cancer patients. Side eects can prove to be benecial for the Antipsychotics are associated with a wide range patient, such as euphoria and an increased appetite in of side eects. Other toms (rigidity and tremor) due to blockage of dopamine typical side eects such as osteoporosis, skin thinning, receptors. In this case the temperature regu steroids, and do not use steroids unless critical in the lation centers fail, resulting in a medical emergency, as noncancer patient. Most of the above-mentioned side eects are Neuroleptics fortunately rare and not of relevance in the period of the Neuroleptics are psychoactive drugs that are commonly end of life. Do Benzodiazepines not underestimate the distress for the patient and family Benzodiazepines are a group of drugs with varying in the presence of delirium. Try to identify the reason sedative, anxiolytic, anticonvulsant, and muscle relax for the delirium. The main indication for these drugs in infection, renal failure, dehydration, or electrolyte im pain management and the palliative care management balances. In rare instances, it may also be a side eect of is the treatment of anxiety and intractable dyspnea. For trait anxiety in terminal ill ceptor, the most prevalent inhibitory receptor within ness, unitrazepam subcutaneously once daily is a very the entire brain. The anticonvulsant properties of ben eective choice (normally in a dose range between 0. During the course of therapy with benzodiaze Benzodiazepines are well-tolerated and safe. Diazepam can be administered orally, real contraindication in the palliative setting if used with intravenously, intramuscularly, or as a suppository. Many of the terms were already estab their system for classication, to issue an updated list of lished in the literature. Subsequent revisions are intended to be specic and explanatory and to serve and additions were prepared by a subgroup of the Com as an operational framework, not as a constraint on fu mittee, particularly Drs. In 1984, in particular diverse specialties including anesthesiology, dentistry, response to some observations by Dr. Devor, a fur neurology, neurosurgery, neurophysiology, psychiatry, ther review was undertaken both by correspondence and psychology. Tose The terms and denitions are not meant to pro taking part in that review included Dr. Devor, the other vide a comprehensive glossary, but rather a minimum colleagues just mentioned, and Dr. Mumford, Sir standard vocabulary for members of dierent disci Sydney Sunderland, and Dr. It is important to recognize that al the activation of the endogenous opioid system and the lodynia involves a change in the quality of a sensation, spinal modulation of pain signalling through activation whether tactile, thermal, or of any other sort. Tere are a number of dif nal modality is normally nonpainful, but the response ferent approaches to diagnosis and treatment in modern is painful. Tere is thus a loss of specicity of a sensory acupuncture that incorporate medical traditions from modality. By contrast, hyperalgesia represents an aug China, Japan, Korea, and other countries. In allodynia the stimulus mode mostly as a complementary treatment to mainstream and the response mode dier, unlike the situation with medicine. This distinction should not be confused by certain types of joint pain, back pain, and headache syn the fact that allodynia and hyperalgesia can be plotted dromes may benet from acupuncture. Allodynia might be provoked by Addiction is a chronic relapsing condition character the touch of clothes, such as in patients with posther ized by compulsive drug-seeking and drug abuse and by petic neuralgia. Addiction from coanalgesics, local treatment with local anesthetics is the same irrespective of whether the drug is alcohol, and/or capsaicin might be of help. Anesthesia dolorosa Every addictive substance induces pleasant states or re lieves distress. Continued use of the addictive substance Pain in an area or region that is anesthetic. Terefore, induces adaptive changes in the brain that lead to toler neurodestructive techniques in pain management ance, physical dependence, uncontrollable craving, and, should be limited to the few indications where anesthe all too often, relapse. For example, in long Absence of pain in response to stimulation that would term opioid therapy, dependence is a normal result, and normally be painful. As with allodynia, the stimulus is the only clinical implication is that dose reduction has dened by its usual subjective eects. Allodynia is pain due to a stimulus that does not nor Acute and cancer-related pain are commonly treat mally provoke pain. Chronic nonmalignant pain requires a multi and hyperesthesia, the conditions seen in patients with disciplinary approach encompassing various pharma lesions of the nervous system where touch, light pres cological and nonpharmacological. The increase of peripheral ated with surgery, childbirth) and some selected chronic neuronal activity is transmitted centrally and results pain syndromes. In general, the oral route of application in sensitization of second and third-order ascend is preferred, but in emergency situations and periopera ing neurons. The general, high-quality pain management is possible with mechanisms of action of antiepileptics include neuro out them. Tricyclic antidepressants have the highest are currently under intense investigation but are not yet eectivity. Local anesthetics are used for local and of monitoring plasma drug concentrations is not to regional anesthetic techniques. As with all Various antiepileptics (carbamazepine, phenytoin, val coanalgesic treatment options for neuropathic pain, proate, gabapentin, lamotrigine, and pregabalin) have patients should be told before the start of therapy that been used for neuropathic pain and more recently for the treatment goal may only be a 50% pain reduction. Together with antidepres Studies have demonstrated that even with optimized sants, they are the most eective coanalgesics. The most treatment, only half of all patients with neuropathic common adverse eects are impaired mental function pain will achieve this goal. In migraine prophylaxis, the (somnolence, dizziness, cognitive impairment, and fa numbers are higher. Serious side may be increased mortality from sudden arrhythmia, eects have been reported, including hepatotoxicity, and in patients with recent myocardial infarction, ar thrombocytopenia, and life-threatening dermatological rhythmia, or cardiac decompensation, tricyclics should and hematological reactions. Tricyclics also block histamine, cho tions should be monitored to avoid toxic blood levels. In consequence, dis triptyline, imipramine, and clomipramine) and pref orders of anxiety can be the result of chronic pain, but erential norepinephrine reuptake inhibitors. One consequence of chronic pain can be agoraphobia, The reuptake inhibition leads to a stimulation of en for example, if the patient is afraid to leave the house dogenous monoaminergic pain inhibition in the spinal because the pain attack might occur on the street, and cord and brain. In consequence, the pa receptor antagonist, sodium-channel-blocking, and tient tends more and more to avoid leaving the house. The antiepileptic drug pregabalin also has some are serious medical illnesses that aect pain patients anxiolytic eect without the risk of addiction of ben more frequently than the average population. Unlike the brief anxiety caused by a stressful mended in a number of textbooks, there is no indication event such as a business presentation or waiting for for anxiolytics as pain killers. Arthritis is the inammation of a joint, with typical In the case of chronic pain, both in developing symptoms including stiness (especially in the morn and developed countries there is an increased preva ing), warmth, swelling, redness, and pain. The prevalence increases when pain oc tion control comes before pain management to avoid curs at multiple sites. In biopsychosocial models of ex among the drugs of rst choice for severe arthritis. Within the experience of tegrated into palliative care by oering relatives support anxiety there is an unspecic feeling of excitement and after the death of the patient. Terefore, palliative care tension as well as unpleasantness and the experience does not stop with the death of the patient. It works as a stimulatory (pronociceptive) neurotransmitter when A disturbance of the brain function that causes confu it is released centrally, and as a proinammatory me sion and changes in alertness, attention, thinking and diator when it is released peripherally. If opioids are nomic changes (changes in the color of the skin, chang suspected to be the cause of delirium, a switch (rota es in temperature, changes in sweating, and swelling). The pathophysiology of causalgia includes local inammation and reorganization processes in the Dependence central nervous system. If causalgia is suspected, diag Physical dependence is a state in which the continuous nosis and treatment should be left to a pain specialist. As a consequence, when opioids have been ad some patients after stroke and may limit the quality of ministered for a prolonged period of time (> 3 weeks) life considerably. All other treatment options are supported only but tapered with a daily dose reduction. Chronic pain Depression Chronic pain is diagnosed if pain persists longer than 6 Depression is a risk factor for pain chronication. For clinical practice it is probably more help tain screening questions aid in diagnosis. Common ful to dene chronic pain as pain that is complicated ndings are sleeping problems, unrest, a lack of ener by certain risk factors according to the biopsychosocial gy that is pronounced in the rst half of the day, and concept of pain chronication: central sensitization to loss of interest. A psychopathological result should howev Approaches to medical treatment that are outside er always form the basis and include an evaluation of of mainstream medical training received in medical suicidal tendency. In accordance with the ndings of 364 Andreas Kopf an investigation by Tang et al. It should always be specied is usually the strongest predictor of desire for death.