Linda M Smith-Resar, M.D.
- Professor of Medicine

https://www.hopkinsmedicine.org/profiles/results/directory/profile/0004790/linda-smith-resar
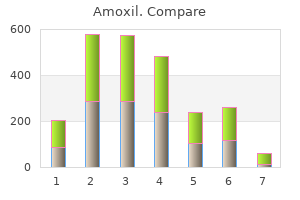
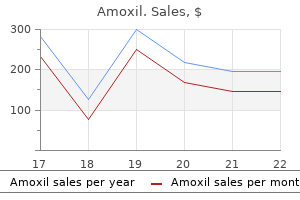
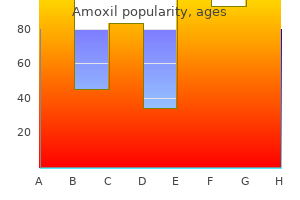
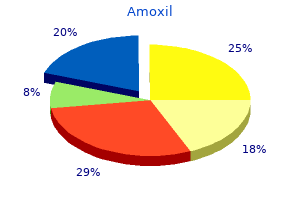
In 47 of the 55 high-fertility countries antibiotic resistance can boost bacterial fitness order amoxil now, fertility declines were smaller than the world median decline of 3 infection 4 weeks after hysterectomy discount 1000 mg amoxil with amex. Among high-fertility countries antibiotic resistant uti in elderly buy amoxil canada, fertility declined only in eight countries at an accelerated pace 7 bacteria amoxil 500 mg sale, namely in Jordan oral antibiotics for acne reviews purchase amoxil overnight, Kenya infection 3 english patch cheap amoxil 250 mg visa, Mayotte, State of Palestine, Rwanda, Tajikistan, Yemen, and Zimbabwe. Many middle-income countries that have only recently reached below-replacement fertility levels have undergone far more rapid transitions than was historically the case for countries that completed their fertility transitions earlier. The countries with more recent and more rapid drops in fertility have less time to adapt to the macro socio-economic changes resulting from the rapid changes taking place in the age-structure of their populations. Contrary to the global trend of declining fertility, several below-replacement fertility countries (32) experienced modest fertility increases over the past 15 years. However, despite these trend reversals, no country with below-replacement fertility has yet returned to the replacement level or above. The highest levels of adolescent childbearing are found in Niger, Mali, Angola, Mozambique and Chad, with adolescent birth rates higher than 150 live births per 1, 000 women, and even higher than 200 live births per 1, 000 women in the case of Niger. Between 1990-1995 and 2010-2015, adolescent birth rates declined faster than total fertility. Between 1990-1995 and 2010-2015, the global proportion of births to adolescent mothers declined 1. Accelerated progress has been made in all regions except Latin America and the Caribbean, especially in Central and South America, where adolescent fertility as a share of all births actually increased from 13. Along with the transition to lower total fertility, the world has witnessed dramatic changes in the age pattern of childbearing. Conversely, in countries of Latin America and the Caribbean and in the middle and low-income countries of xiii Asia and Oceania, births are taking place now at younger ages than before, a trend caused by declines in high parity births without significant changes in the spacing between births. More than half of the projected population growth is due to population momentum (namely, 26 of the 40 percentage points), 8 percentage points of the change are due to above-replacement fertility, and 6 percentage points are credited to anticipated mortality declines. In Africa, above-replacement fertility will account for 87 per cent of the projected population increase, adding more than 900 million people over this period. In high-fertility countries, total fertility is projected to decline towards the replacement level, from 2. All regions, except for Africa, are expected either to remain below or to reach the replacement level of fertility by the end of this century. The future pace of fertility decline, however, is inherently uncertain, and whether fertility will in fact decline more or less rapidly than in previous periods, particularly in sub-Saharan Africa, is a subject of on-going debate. In the current projections, 21 African countries are expected to complete their transitions only after 2100. Consequently, high-fertility countries will continue to have growing and youthful populations, even if the projected fertility declines materialize. Countries dipping just below the replacement level in 2010-2015 are expected to follow trajectories similar to below-replacement fertility countries, with fertility continuing to decline to levels well below replacement, and then at some low point to bounce back and start to rise gradually towards a level that is still below replacement. Projections suggest that the lower the present level of fertility, the faster their future increase is likely to be. High-quality and timely data are key to making policy decisions and to monitoring progress towards the achievement of the Sustainable Development Goals. A review of empirical data suggests that our knowledge about fertility levels and trends is based on insufficient or otherwise inadequate empirical evidence. In more than half of the countries and areas of the world, recent fertility estimates are not based on complete vital registration data. The greatest challenges are in Africa and Oceania, where timely fertility estimates based on complete vital registration exist for only 12 per cent and 38 per cent of countries or territories, respectively. Special efforts need to be directed toward strengthening civil registration and vital statistics, toward scaling up national statistical capacities, and toward strengthening and modernizing statistical systems so that they can produce and disseminate timely and reliable demographic data on fertility and births. Globally, total fertility has declined at unprecedented rates and to unprecedented levels, reaching a median level of 2. Also, low fertility in Europe, Northern America, Eastern Asia, and parts of Oceania and Latin America is a cause of concern due to population ageing and, in some cases, population decline. Population ageing, an inevitable consequence of low levels of fertility and increased longevity, presents another set of issues for the achievement of the 2030 Agenda for Sustainable Development, including insufficient coverage or adequacy of social protection schemes for the rapidly increasing number of older persons in the world. Estimates of some parameters of the fertility transitions, including the level and pace of fertility decline at different stages of the fertility transition, are provided for all countries of the world, including for countries that commenced their fertility transitions prior to 1950. The discussion of changes 3 in fertility levels and age patterns of childbearing at the regional level and for individual countries is supplemented with an extensive set of annex plots. This report presents an in-depth analysis of past, present and projected levels and trends of adolescent fertility at the global, regional as well as national levels. The report further extends previous publications by quantifying the effect of fertility on population growth over the period from 2010 to 2050, with a focus on those countries where fertility is the driving factor behind population growth or decline. The report also includes a chapter on empirical data sources and methods for fertility estimation to address the call of the 2030 Sustainable Development Agenda for strengthening data production and the use of better data in policymaking and monitoring. Drawing on a recently established database of empirical fertility data, the 2015 World Fertility Data (United Nations, 2015c), this report provides estimates of gaps and timeliness in the empirical fertility data used as a basis for producing estimates of fertility levels and trends. Many countries classified as part of developing regions now have very low fertility. The best estimates of fertility are obtained from a universal and well-functioning civil registration and vital statistics system (United Nations, 2014). In such a system, all births are registered shortly after occurrence and a birth certificate is issued for every child born. The information from the birth certificates is then used for the production of vital statistics. The population exposures needed for computations of fertility rates are based on annual population estimates, which are derived from the population by age and sex enumerated in population censuses, and births, deaths, and migration for intercensal or postcensal periods. In countries with operating population registers population censuses are not regularly conducted, since statistics in such countries are based on the continuous collection of information on both population and vital events. In these countries, annual population estimates are based on the data recorded in the population registers. For countries with a reliable civil registration and vital statistics system, as is the case in most developed countries and in some developing countries, age-specific fertility rates and derived indicators. They are based almost entirely on complete data collected on births and population estimates in a country, with minimal assumptions required. The term "direct" is used to qualify a broader class of estimation methods that rely mostly on the reporting of demographic events, rather on information only indirectly related to an estimate or obtained based on a statistical model. Even in countries with accurate and complete birth registration, population estimates used as denominators for computing fertility rates are frequently revised. For example, in 2012 the Australian Bureau of Statistics revised population estimates back to 1990, which in turn led to retrospective revisions of fertility rates back to that year. The updated estimates of fertility are higher than previously estimated, due to the downward revision of the population figures. Population registers tend to produce population data of better quality than censuses. Nevertheless, population estimates based on registers might still be affected by inaccurate data on international migration. Similarly, foreigners living habitually in the country and who are included in the population register, will still be included erroneously if they return to their home countries without notifying the authorities. It is not unusual to find coverage rates of international emigration below 50 per cent (Poulain and Herm, 2013). Additional sources of errors in population registers may include incorrect records of age or other demographic characteristics of foreign-born persons. When vital registration systems fail to record all births that take place during a given period of time or population censuses fail to enumerate every individual, their coverage is said to be incomplete. Using incomplete data to produce fertility estimates requires adjustments to births and population estimates. In the case of population censuses, adjusted population estimates are usually produced by conducting a post enumeration survey. The coverage and completeness of civil registration is often assessed by a dual registration approach or by using alternative sources of information on vital events. In countries with incomplete civil registration systems, data from incomplete vital statistics are frequently supplemented by data from household surveys to derive final estimates of fertility. More detailed accounts of methods for assessing the quality of population and vital statistics are given in Preston and others (2001), Bogue and others (1993), Shryock, Siegel, and Associates (1980). Moriyama (1990) describes an array of methods historically used to evaluate the quality of population and vital statistics in the United States. Yet many countries still face difficulties in establishing a well-functioning civil registration and vital statistics system. Only 53 per cent of countries or areas globally reported basic data on births by age of mother from complete civil registration and vital statistics systems. In some countries, vital registration is incomplete for a variety of reasons: many births go unregistered if they take place at home; newborns who die shortly after birth may not be registered; registration fees may provide a disincentive for individuals to register births; local registration offices may fail to transfer birth records to the national statistical office; the national office may lack resources to process transferred records and produce vital statistics. In addition, there could be long delays between the occurrence of a birth and its registration. For example, birth registration could be delayed by parents until 4 the child reaches school age. In countries with incomplete vital registration, the main sources of information on fertility levels and trends are population censuses and nationally-representative household surveys. Because population censuses aim to enumerate all individuals in a country and to record information on various topics, normally only a very limited set of questions about fertility is included. Typical questions asked in a population census are about a) lifetime or cumulated fertility (children ever born), and b) recent fertility. The data on recent births collected in censuses are used to derive estimates of current fertility, but these estimates are often implausibly low due to errors resulting from omissions of births, recall problems, misinterpretation of the reference period before the census, and significant non-response rates, amongst other problems (United Nations, 1983). These challenges led to the development of demographic methods for estimating fertility by incorporating information that indirectly relates to the quantity in question, commonly known as methods for indirect estimation (United Nations, 1983, Moultrie and others, 2013). Two independent questions on fertility included in population censuses, a question on lifetime fertility and a question on recent births, make consistency checks between current and cumulative fertility possible. Under fairly general assumptions about fertility trends and typical errors, direct estimates based on recent births can be adjusted by incorporating information on lifetime fertility. This was the original idea behind the P/F (parity/fertility) ratio method (Brass, 1964). A more flexible mechanism for collecting fertility data are sample household surveys. Due to their smaller sample sizes, data on fertility can be collected more frequently and questions can be more detailed and targeted than in population censuses. Questions on key demographic characteristics such as education characteristics of the mother are commonly included in the questionnaires making it possible to study fertility differentials by socio economic factors. Full birth histories have become the dominant source for producing estimates of fertility levels and trends for countries without well-functioning civil registration and vital statistics systems. Birth histories are usually collected from a random sample of women of reproductive age, commonly defined as ages 15 to 49. Typically, data are collected from all women in this age group, but in some countries the collection of data has been restricted to married women only. Green squares on the vertical line in 2010 designate mothers interviewed in this survey; the position of a square corresponds to the age of the mother. For example, the oldest mother interviewed in this survey was aged 48 as shown by the highest green square in 2010. She was born in 1962 as illustrated by the diagonal green line going from age 48 in 2010 to age 0 in 1962. Births recorded in this survey are shown as red circles on the life lines of their mothers. The oldest mother in this figure, for example, gave birth three times, at ages 25, 29 and 32. Direct computation of fertility rates from birth histories is fairly straightforward and well documented (Croft, 1991; Rutstein and Rojas, 2006). To compute an age-specific fertility rate for a defined period of time and age group one needs to compute the number of births and time lived by all mothers in the age group (population exposure). Total fertility is then computed by summing age-specific fertility rates over age. For this period, the estimate of the total fertility rate is based virtually entirely on empirical data. As one moves back in time from the date of the survey, empirical fertility rates are available only for progressively lower age groups (red triangle in figure I. A common assumption for deriving fertility estimates for age groups with no data, and, consequently, estimates of trends in total fertility, is that the age pattern of fertility is unchanged before the survey.
Patients removed from the ventilator are 9 provided with alternative forms of medical intervention and/or palliative care usp 51 antimicrobial preservative effectiveness discount amoxil online american express. Triage Charts for Step 3 Criteria for each color code at the 48 and 120 hour assessments are presented below oral antibiotics for mild acne purchase amoxil uk. Decision-Making Process for Removing a Patient from a Ventilator 10 There may be a scenario where there is an incoming red code patient(s) eligible for ventilator treatment and a triage officer/committee must remove a ventilator from a patient whose health is not improving at the 48 infection no fever cheap amoxil 1000 mg with visa, 120 virus new york purchase cheap amoxil on-line, or subsequent 48 hour time trial assessments antibiotic walking pneumonia generic amoxil 250mg without prescription, so 10 While there may be yellow color code patients waiting for ventilator therapy antibiotic resistance diagram generic amoxil 500 mg with mastercard, all red code patients must be attended to first. Already ventilated yellow code patients would not be removed from the ventilator with the arrival of an incoming yellow code patients since both of these patients have equivalent likelihoods of survival. If there are no patients in the blue category, then a triage officer/ committee proceeds to the yellow code patients. Interface between Pediatric and Adult Patients In an influenza pandemic, the same triage officer/committee may need to allocate ventilators to both adult and pediatric patients. When either selecting or removing a patient in a patient pool that consists of both children and adults, a triage officer/committee is not permitted to compare the health of patients. Palliative care is provided to all patients throughout the triage process, regardless of prognosis. Conclusion the triage process requires regular reassessments of the status of the pandemic, available resources, and of all patients. As new data and information about the pandemic viral strain become available during a pandemic, the pediatric clinical ventilator allocation protocol may be revised accordingly to ensure that triage decisions are made commensurate with updated clinical criteria. Using clinical criteria, patients who are deemed most likely to survive with ventilator treatment have an opportunity for ventilator therapy to maximize the number of survivors. The neonatal clinical ventilator allocation protocol applies to all patients 28 days old and younger in all hospitals Statewide. The attending physician and triage officer/committee should have experience working with neonates. Patients with exclusion criteria do not have access to ventilator therapy and instead are provided with 2 alternative forms of medical intervention and/or palliative care. If medical information is not readily available or accessible, it may be assumed a patient is free of exclusion criteria and may proceed to the next step of the clinical ventilator allocation protocol. Physicians may also consider severe, end-stage chronic medical conditions when assessing mortality risk. For most patients who are sick with only influenza and have no other comorbidities, the single organ failure is limited to their lungs. In some instances, a patient may require ventilator therapy because of influenza and not because of the chronic care disease itself. If resources are available, patients in the yellow category also have access to ventilator treatment. Finally, a triage officer/committee must determine how to define what the cutoffs should be for highest, high/uncertain, moderate, and low risk of mortality risk categories because there are no evidence-based data early in a pandemic. Step 3: Periodic Assessments for Continued Ventilator Use (Time Trials) Periodic clinical assessments at 48 and 120 hours using physician clinical judgment are conducted on a patient who has begun ventilator therapy to evaluate whether s/he continues with the treatment. The results of the time trial clinical assessments are provided to a triage officer/ committee. Instead, a triage decision should examine all clinical variables so that an overall health assessment of a patient can be made. Thus, this factor may only play a role in the triage decision if the appropriate data are available. Using the results of these three variables, a triage officer/ committee assigns a color code (blue, red, yellow, or green) to the patient. Thus, the extent of change in the three variables indicates whether a patient is improving, worsening, or experiencing no change in health status. After 120 hours, a patient must demonstrate a pattern of further significant improvement in health to be placed in the red color code. A triage officer/committee determines whether a patient continues with ventilator therapy based on the extent of change in the three clinical variables. When assigning a patient a color code, a triage officer/committee must determine how to define what the cutoffs should be for highest, high/uncertain, moderate, and low risk of mortality risk categories because there are no evidence-based data early in a pandemic. The official assessments only occur after 48 and 120 hours (and subsequent 48 hours) of ventilator therapy. Decision-Making Process for Removing a Patient from a Ventilator 10 There may be a scenario where there is an incoming red code patient(s) eligible for ventilator treatment and a triage officer/committee must remove a ventilator from a patient 10 While there may be yellow color code patients waiting for ventilator therapy, all red code patients must be attended to first. First, a blue code patient(s) is the first patient(s) eligible for ventilator removal. If there are several patients in the blue (or yellow) category, a triage officer/committee is not permitted to compare the health of patients within the same color category. A patient may only be removed from a ventilator after an official clinical assessment has occurred or where the patient develops a medical condition on the exclusion criteria list. If all ventilated patients at the 48, 120, and subsequent 48 hour time trial assessments receive a red color code, then none of these patients discontinue ventilator therapy. The incoming red code patient(s) remains in an eligible patient pool and receives alternative forms of medical intervention and/or palliative care until a ventilator becomes available. Interface between Neonatal and Pediatric Patients In an influenza pandemic, the same triage officer/committee may need to allocate ventilators to both neonatal and pediatric patients. Because the patient pool consists of only children, young age would not be a consideration. Instead, a random process should be used to choose the patient for ventilator therapy when there are more patients than ventilators available. In addition, a random selection method is conducted each time a ventilator becomes available. As new data and information about the pandemic viral strain become available during a pandemic, the neonatal clinical ventilator allocation protocol may be revised accordingly to ensure that triage decisions are made commensurate with updated clinical criteria. Influenza A is responsible for most human influenza disease, causes avian influenza, and is the source of all past influenza pandemics in humans. Influenza B is a disease of humans only, while inluenza C causes milder illness in both humans and swine and occurs uncommonly. Influenza A infects humans, birds, pigs, horses, whales, seals, and has recently been recognized in felines. A pandemic is a global outbreak that occurs when a new, highly pathogenic strain of influenza type A virus emerges in the human population and spreads easily from person-to-person worldwide, aided by the lack of human immunity to the novel strain. Past influenza pandemics have led to high levels of illness, death, social disruption, and economic th loss. Influenza in Bird Populations All birds are believed susceptible to infection with avian influenza. Recent research has shown that viruses of low pathogenicity can quickly mutate into highly pathogenic viruses. In the absence of prompt control measures backed by good surveillance, epidemics can last for years. For example, an epidemic of H5N2 avian influenza, which began in Mexico in 1992, started with low pathogenicity, evolved to the highly fatal form, and was not controlled until 1995. Mechanism of Transmission to Humans Influenza A viruses are genetically labile and well adapted to elude host defenses. As a result of these uncorrected errors, the genetic composition of a virus changes during passage through humans and animals, and the existing strain is replaced with a new antigenic variant. These changes in the antigenic composition of influenza A viruses are known as antigenic drift. As populations will have no immunity to the new subtype, and as no existing vaccines can confer protection, antigenic shift has historically resulted in highly lethal pandemics. For this to happen, a subtype of avian influenza needs to acquire genes from human influenza viruses that enable person-to-person transmission. Conditions favorable for the emergence of antigenic shift are thought to involve humans living in close proximity to domestic poultry and pigs. Close contact with live infected poultry was the source of human infection, and the virus was shown to have jumped directly from birds to humans. The strain circulating in Asia appears highly pathogenic for humans, and immunity in the human population is generally lacking. Human cases of H5N1 have been reported officially in Vietnam, Thailand, and Cambodia. Probable person-to-person transmission was identified in Thailand involving transmission from an ill child to her mother and aunt. However, the strain has not yet been shown to be easily transmitted between humans, and sustained person-to-person transmission has not occurred. However given that the virus responsible for human-to-human transmission will be a novel strain, the specifics of its clinical presentation will not be known until the outbreak actually occurs. Virus isolation studies carry higher risks of inadvertent transmission and require even more stringent precautions. Antiviral Agents There are 2 key uncertainties that challenge planning for administration of antiviral agents in the event of an avian influenza outbreak among humans. First, it is unclear how much antiviral drug will be available in the event of a large-scale outbreak. Second, the influenza strain responsible for the outbreak and its profile of antibiotic resistance may not be fully known in advance. There are 2 classes of antiviral agents for influenza: adamantanes (amantadine and rimantadine), and neuraminidase inhibitors (zanamivir and oseltamivir). The drugs differ in cost, routes of administration, adverse events, contraindications, and potential for antiviral resistance. However, there are no controlled studies of patients infected with influenza A(H5N1). Candidate vaccines against H5N1 subtype were developed during 2003 for protection against the strain that was isolated from humans in Hong Kong in February of that year. Poultry Workers Birds that are infected with avian influenza viruses can shed virus in saliva, nasal secretions, and feces. Activities that could result in exposure to avian influenza-infected poultry include euthanasia, carcass disposal, and cleaning and disinfection of premises affected by avian influenza. Health Care Providers Human influenza is transmitted primarily via large respiratory droplets, and isolation precautions for typical human influenza include Standard plus Droplet Precautions. These precautions should be continued for 14 days after onset of symptoms or until either an alternative diagnosis is established or diagnostic test results indicate that the patient is not infected with influenza A virus. Although this will not protect against H5N1 influenza A, it will help avoid simultaneous infection with other influenza strains and may thereby decrease the risk of genetic reassortment. Interim Recommendations for Infection Control in Health-Care Facilities Caring for Patients with Known or Suspected Avian Influenza. Fatal avian influenza A (H5N1) in a child presenting with diarrhea followed by coma. In: Principles and Practice of Infectious Diseases, 6th edition; Gerald Mandell et al, Eds. Each of the guidelines is presented in this section; the remainder of the document provides detailed information about each guideline including the rationale, considerations and pertinent background material. Pandemic Flu Calls (Figure 1) illustrates a sample call flow decision to be made in a period of pandemic influenza vs.
See Esophageal varices; Portal hypertension and meseneric adenitis and enteritis associated with treatment for uti back pain cheap 1000mg amoxil mastercard, 357 varices bacteria resistant to antibiotics discount amoxil 1000mg with amex. Visceral malignancy Vascular congestion antibiotic 93 3196 discount amoxil online amex, omental infarct associated with virus jumping species discount amoxil 1000 mg without a prescription, 90 primary antibiotic infection buy amoxil 1000 mg with amex, sclerosing mesenteritis vs antibiotics for acne breakout discount amoxil amex. There have been many recent advances in the understanding of its molecular genetics and biology, and in the diagnosis and management of its manifestations. Yet, diagnosis, evaluation, prevention and treatment vary widely and there are no broadly accepted practice guidelines. Barriers to translation of basic science breakthroughs to clinical care exist, with considerable heterogeneity across countries. Despite continuous destruction of renal parenchyma, compensatory hyperfiltration of the 5, 6 surviving glomeruli maintains renal function within the normal range for decades. Many therapeutic targets have been identified and tested in animal models and several clinical trials demonstrate encouraging results. Additional information about the conference can also be found online at: kdigo. Pre symptomatic screening of at-risk children is not currently recommended based on the potential for adverse psychological consequences, denial of future insurance coverage, and the lack of evidence that such screening would improve outcomes. The possible implications of a positive diagnosis should be discussed beforehand and results clearly explained to the patient and to their parents in the case of minors. The implications of a positive diagnosis should be discussed beforehand and results clearly explained to the patients and their parents in the case of minors. Otherwise, the differential diagnosis needs to be broadened to include other cystic kidney diseases (see Table 2). There is no consensus on a diagnostic algorithm that integrates clinical findings with renal imaging and molecular genetic testing. Newborns or children with renal cysts comprise a heterogeneous diagnostic group of 8 common and rare cystic disorders. Consultation with a specialist with expertise in hereditary renal disease is strongly encouraged as genetic testing is often required. Cerebellar and spinal disease mutations in hemangioblastoma; retinal angiomas; serous 20% cystadenomas and neuroendocrine tumors of pancreas; pheochromocytoma; renal cell carcinoma. Simple renal cysts Acquired None Common; increase in number and size with age; normal renal function; normal-sized kidneys. The hallmark of mosaicism is the presence of more than one 28 genetically distinct cell line in an individual. The difference between somatic and germline mosaicism is based on the findings of genetically distinct populations of cells in 10 29 the somatic and germline tissues, respectively. Mosaicism is a well-recognized cause of variable disease expressivity in more than 30 Mendelian disorders but one that is very difficult to diagnose by Sanger sequencing. However, Sanger sequencing of an affected offspring of the mosaic individual may uncover the pathogenic mutation. Marked discordant renal disease severity among affected family members has been 32-35 well documented suggesting a role for both genetic and environmental modifiers. Molecular genetic testing is not required for most patients but may be considered in cases of equivocal or atypical renal imaging findings. The most 12 common approach is the biopsy of cleavage-stage embryos in which one blastomere is removed from the embryo on day 3 of development. An alternative biopsy 44, 45 method (blastocyst biopsy) targets the trophectoderm on day 5 of development. This approach removes multiple cells for analysis without sacrificing any part of the embryo proper. It is usually combined with cryopreservation and thawed embryo transfer to allow more time for the genetic testing. Ideally, 46 treatment should start early, when the kidney parenchyma is relatively preserved. Nevertheless, treatments in later stage disease are also important to preserve kidney function and their efficacy and safety should also be determined. However, kidney volume in 3, 4, 47, 48 relation to age can identify patients with progressive disease. When approved disease-modifying therapies become available or if lifestyle modifications are shown to alter disease progression, repeated imaging may become an informative tool. Other imaging parameters Standardized reporting of imaging findings should also include the exact number of cysts when there are less than 10 in each kidney and the liver; minimal and maximal size of cysts in both organs; presence of complex cyst(s) and exophytic cyst(s); and the dominant pattern. Other studies have underlined the importance of the non-cystic tissue as an indicator of disease severity. Importantly, when developing novel medical treatments, it should be investigated whether such treatments interfere with tubular creatinine secretion. Its origin and glomerular versus 69 tubular pattern have not been thoroughly ascertained. In patients with nephrotic range proteinuria, the presence of a second kidney disorder and a renal biopsy should be considered if access to renal parenchyma is feasible. They can also be used to improve patient care but there are 71 gaps in knowledge about their usefulness. In accordance with this guideline, blood pressure targets should be individualized taking comorbidities into account. Calcium channel blockers may lower intracellular calcium concentration in collecting duct cells. This may result in an increase in tubular cell proliferation and fluid secretion, 90 in turn leading to accelerated cyst growth and kidney function decline. For instance, in patients with angina, beta-blockers may be preferred, and in subjects with prostate hypertrophy, alpha-blockers would be appropriate. The approach to hypertension screening is dependent on country-specific circumstances. There is no consensus at what age such screening should be started, nor what the frequency should be. Screening from the age of 5 years onward, with an interval of 3 years in cases in which no hypertension is found, seems prudent. However, many of these studies were underpowered, had short periods of follow-up or included patients in early disease stages at low risk for progression and with relatively stable renal function, in whom it is difficult to detect potential beneficial effects. Prescribing a protein restricted diet should be done with appropriate patient education, preferably by a renal dietician, and patients on such a diet should be monitored for malnutrition, especially those patients with high total kidney and liver volumes, for whom dietary intake of nutrients may become insufficient. Given the theoretical background and the evidence from experimental data, we advise patients to increase their water intake. Some have advised to increase the intake of water to achieve an average 113 urine osmolality of 250 mOsm/kg. Whether an increase in water intake can be 114 sustained over long periods of time remains to be determined. The risk of hyponatremia has to be considered, particularly in patients who have impaired kidney function and are also on a sodium restricted diet and receiving diuretics or drugs that can inappropriately stimulate the release of vasopressin or potentiate its action, such as 113 serotonin reuptake inhibitors and tricyclic antidepressants. Because the study was not randomized, lasted only one year, and the patients in the high water group had a higher salt intake (reflected by higher urine sodium excretion), it needs to be interpreted with caution. Mice tolerate much higher doses and blood levels than rats and humans, and these high doses of rapalogs were consistently 122, 123 effective in orthologous and nonorthologous mouse models. Several strategies to overcome the systemic toxicity and limited renal bioavailability of rapalogs deserve 128-130 further study. These trials were of short duration and included a relatively small number of patients. A favorable effect was noted on the secondary outcome of kidney function, but this endpoint also did not reach statistical significance. Until the results of larger trials become available, somatostatin analogues should not be prescribed for renoprotection outside of a research study. Hematuria and cyst hemorrhage Cyst hemorrhage or gross hematuria occur in approximately 60% of patients. Cyst hemorrhage can be associated with fever and differentiation from cyst infection may be difficult. Gross hematuria can result from cyst hemorrhage, nephrolithiasis, infection and rarely renal cell or urothelial carcinoma, but often no specific cause can be identified. Hematuria is positively associated with increased kidney volume and cyst wall calcifications. Hematuria can be asymptomatic or painless, or it can associate with acute pain syndromes necessitating medical attention and narcotic analgesics. Episodes of cyst hemorrhage or gross hematuria are usually self-limited and resolve within 2 to 7 days. If symptoms last longer than 1 week or if the initial episode of hematuria occurs after age 50 years, investigation to exclude neoplasm should be undertaken. Rarely, bleeding can be persistent or severe, sometimes with extensive subcapsular or retroperitoneal hematomas, requiring hospitalization. Increased urinary stasis and metabolic factors (reduced urine pH, ammonium excretion and urinary 143-146 citrate) account for the increased frequency of stones. Whether nephrolithiasis associates with an increased risk for renal insufficiency, as it has been reported in the 147 general population, is uncertain. Information on indications and results of surgical interventions for nephrolithiasis are limited to reports of center experiences and therefore subjected to substantial bias. Flexible ureterorenoscopy with laser fragmentation has also been used safely and effectively 151, 152 with less risk for traumatic nephron loss. Management of renal cyst infection Recent meta-analyses highlight the course and successful management of both renal 153 and liver cyst infections. Blood and urine cultures may be negative and cyst aspiration for culture should be considered if a complex cyst in the right setting is identified. Lipid-permeable anti-microbial agents such as 28 fluoroquinolones and trimethoprim-sulfamethoxazole, depending on sensitivity (if 158 available), remain the standard treatment for cyst infections. Once antibiotic therapy has been initiated, there is wide variability regarding duration of treatment and indications and timing of percutaneous or surgical draining; however extended antibiotic therapy is often warranted. It has a negative impact on sleep, activity, mental status, and social relationships. Health care providers often fail to discuss pain during encounters with patients, leading to suboptimal management. Careful history taking and physical exam (location 160, 161 and characterization of the pain) are the initial steps. Differential diagnosis should be sought by a multidisciplinary workup with radiologists, physical therapists, and pain specialists. Pre-medication therapy needs to be initiated with consultation of the patient and physical therapist. Percutaneous cyst aspiration is helpful as a diagnostic procedure to determine whether a more permanent intervention such as cyst 162, 163 sclerosis or laparoscopic cyst fenestration is worth pursuing. Celiac plexus 164 blockade, radiofrequency ablation, and spinal cord stimulation have also been used. Thoracoscopic sympathosplanchnicectomy may be helpful in some patients with disabling pain but it is invasive and has potential complications such as pneumothorax 165 and orthostatic hypotension. Laparoscopic renal denervation has been helpful in a 166 small series of patients. Counseling for both parents should also discuss the risk of passing on the disease to their offspring, and the risks to both the baby and mother should pregnancy take place. Utilization of appropriate antihypertensive medications documented to be safe in pregnancy is important. Nevertheless, pregnancy induced hypertension and preeclampsia occur more frequently. As for patients with other kidney disease etiologies, a direct comparison of the prognosis of transplanted and non-transplanted patients is difficult, due to strong selection bias. Appropriate individual and family counseling is required to support decision making in such situations. Therefore the indication should be based on a risk-benefit analysis and kidneys should not be routinely removed prior to transplantation. Hand assisted laparoscopic nephrectomy may be better tolerated, although conversion to open nephrectomy may be necessary for very large 186-188 cystic kidneys. Possible indications include recurrent and/or severe infection, symptomatic nephrolithiasis, recurrent and/or severe bleeding, intractable pain, and suspicion of renal cancer. Insufficient space for insertion of a kidney graft may represent an indication for native nephrectomy, but establishing this need is difficult and practices 32 174, 182, 184, 189 vary widely, with pre-transplant nephrectomy rates between 3% and 100%. While no direct comparisons of different strategies are available, on average less than 174, 189, 190 one third of patients in published series undergo pre-transplant nephrectomy, a figure that may serve as a benchmark for transplant programs. The decision for or against nephrectomy should also take into account that native kidney size typically 191 declines after transplantation. Space considerations are usually an indication for unilateral rather than bilateral nephrectomy. Experience with both, prior and 189, 192 simultaneous nephrectomy has been reported but both practices have not been directly compared in a prospective and randomized fashion.
Safe amoxil 500 mg. Monotherapy Vs Combination Antimicrobial Therapy of Sepsis.
Raccoons could be infected were relatively resistant to infection treatment for uti in goats safe 1000mg amoxil, and while quail experimentally with an avian H4N8 virus virus games online cheap amoxil 650mg with amex, 286 striped skunks transmitted this virus efficiently to other birds antimicrobial vs antibacterial soap cheap amoxil online, pigeons and (Mephitis mephitis) with H4N6 and H3N8 viruses antibiotic 3 pills buy amoxil overnight, and Pekin ducks did not infection from cat scratch buy amoxil 650mg fast delivery. A parakeets shed high titers in oropharyngeal secretions in number of influenza viruses (H3N3 yeast infection 8 weeks pregnant order discount amoxil on line, H3N8, H7N7, H4N5, one study. Worldwide eradication of the reported human infections caused by Asian lineage H5N8 Asian lineage H5 viruses is not expected in the near viruses, although four infections with H5N6 viruses have future. However, People and other mammals are usually infected with asymptomatic, naturally infected cats appeared to excrete avian influenza viruses during close contact with infected these viruses only sporadically, and there was no evidence birds or their tissues, although indirect contact via fomites that they transmitted them to other cats. Likewise, the H7N9 virus cases where ingestion probably occurred, but additional 399 in China does not appear to spread readily between people, routes of exposure also existed. Some authors have also speculated about the possibility Host-to-host transmission of avian influenza of virus transmission between mammals and birds in wild viruses in mammals ecosystems, based on evidence from Qinghai Lake, China, Infected animals and people shed avian influenza where H5N1 viruses related to those previously found in wild plateau pikas192 were isolated from dead migratory viruses in respiratory secretions. Fecal shedding has been reported occasionally, although its significance is still birds in 2009-2010, although this clade had not been found 407, 408 in wild aquatic birds at this location in 2007. The persistence of these viruses can be ethanol, quaternary ammonium compounds, aldehydes influenced by many factors such as the initial amount of (glutaraldehyde, formaldehyde), phenols, acids, povidone virus; temperature and exposure to sunlight; the presence of iodine and other agents. Other physical, a few days in individual birds, and up to 2 weeks in the chemical or biological factors in natural aquatic 2, 3, 79 429, 430, 442, 443 flock. A 21-day incubation period, which takes into environments may also influence persistence. One unusual H10 virus isolated longer on feathers than other objects in two reports: at least from waterfowl affected the kidneys and had a 50% 445 mortality rate in some intranasally inoculated chickens. Marked depression, decreased feed and water 32 signs, with death often occurring within 1-2 days. Some intake, and other systemic, respiratory and/ or neurological species at the facility did not seem to be affected. Egg production decreases experimentally infected common reed buntings (Emberiza or stops, and depigmented, deformed and shell-less eggs 484 schoeniclus). Both symptomatic and no clinical signs and inefficient virus replication in dogs subclinical infections have been reported in felids. One cat inoculated with an Asian lineage H5N8 virus, while cats had a fever, depression, dyspnea, convulsions and ataxia, had mild and transient signs, including fever and marginal 24, 25, 29 weight loss. One of the latter cats was apparently well up to 24 hours before its Mammals infected with other subtypes death. Fatal illnesses with conjunctivitis and severe Infections with influenza A viruses, apparently of avian respiratory signs were described in experimentally infected 233, 235, 237, 403, 488 origin, have been associated with outbreaks of pneumonia cats. Asymptomatic infections were reported 1, 101, 203, 489, 490 or mass mortality in seals. The clinical signs in in housecats in an animal shelter that had been accidentally 191 some outbreaks included weakness, incoordination, exposed to a sick, H5N1-infected swan. In another outbreak, captive milder or asymptomatic, suggesting that co-infections may lions, tigers, leopards and Asiatic golden cats were lethargic 31 have increased the severity of the illness. An influenza and had decreased appetites (without respiratory signs) for 32 virus was also isolated from a diseased pilot whale, which 5-7 days, but recovered. Most experimentally infected dogs There are only a few reports of naturally acquired or remained asymptomatic or had relatively mild signs such as experimental infections in other mammals, except in animal fever (which was transient in some studies), anorexia, 34, 237, 238 models for human disease (ferrets and mice). More severe virus caused respiratory signs (sneezing, coughing, and respiratory signs (cough, labored breathing), with one fatal nasal and ocular discharges) and elevated mortality in mink infection, were reported only in dogs inoculated directly 1, 31 34 during an outbreak in Europe. A study that infected both dogs and cats among mink in China was characterized by mild respiratory found that the cats were more susceptible and developed 204 signs, with no reported deaths. One group isolated 13 severe clinical signs, while dogs were likely to have few or 488 H9N2 viruses from sick and healthy dogs in a study from no signs despite shedding virus. Bloody nasal discharge, severe Post Mortem Lesions Click to view images pulmonary congestion and edema, and congestion of the spleen, kidney and liver were reported in a naturally Low pathogenic avian influenza in birds infected dog. Samples from of the head, wattle and comb; excess fluid (which may be internal organs. Cross However, clinical protection is not necessarily correlated reactivity between influenza viruses can be an issue in with reduced virus shedding, and some birds can become serological tests. Some animals valuable species such as zoo birds from highly virulent infected with avian influenza viruses may fail to develop 58, 291, 518 viruses such as H5N1. For mammals, prevention involves avoiding close contact with infected birds or their tissues. Keeping Control susceptible animals indoors may be helpful during outbreaks in birds. Disease reporting A quick response is vital for containing avian influenza Morbidity and Mortality outbreaks, and in some cases, for minimizing the risk of zoonotic transmission. Unusual mortality among wild birds should also greater than 95%, typically with much higher rates in birds from aquatic environments than terrestrial species. These detected in 8% of 25 cats in Egypt, and 73% of 11 cats in H5N1 viruses tend to reemerge during colder seasons in an unpublished study from Thailand. Fatal infections with these viruses have been reported occasionally in other species such as raccoon Mammals dogs, palm civets and mink, but little more is Pigs seem to be infected fairly regularly by avian 27, 28, 31, 33 known. Other avian influenza viruses have caused influenza viruses from birds, often with only minor outbreaks in mink. However, an H9N2 Low levels of exposure have been reported for outbreak among mink in China was reported to be mild, H5N1, H9N2 and other subtypes in some endemic areas, 204 with no elevated mortality. Mink on some other Chinese with seroprevalence to these viruses typically ranging from 204, 254 farms also had antibodies to H9N2 viruses. The < 1% to 5% and occasionally higher, and virus detection severity of influenza in mink is thought to be influenced by rates of <1% to 7. His initial symptoms two cases was fatal; the other patient required mechanical included a persistent high fever and headache, but no signs ventilation, but recovered after treatment with oseltamivir of respiratory disease. The virus isolated from this case had and antibiotics (details of the third case have not been accumulated a significant number of mutations, while published). This patient was hospitalized but upper respiratory signs, fever, and in some cases, recovered without antiviral treatment. A 20-year-old gastrointestinal signs (mainly vomiting and abdominal pain) 108, 328-334 woman infected with an H6N1 virus in China developed a and mild dehydration. All of these patients, persistent high fever and cough, progressing to shortness of including a 3-month-old infant with acute lymphoblastic 334 breath, with radiological evidence of lower respiratory tract lymphoma, made an uneventful recovery. She made an uneventful recovery after treatment influenza-like upper respiratory signs were also reported in 330 with oseltamivir and antibiotics. The third patient, 48 hours after the clinical signs begin, although they may who was 55 years of age, recovered after mechanical also be used in severe or high-risk cases first seen after this ventilation and treatment with various drugs including time. The other two patients also received used antiviral drug, appears to increase the chance of oseltamivir. H5N1 vaccines for humans have been developed adamantanes (amantadine, rimantadine), and neuraminidase in the event of an epidemic, but are not in routine use. In some confirmed, asymptomatic or mild cases have also been cases, recommendations may include antiviral prophylaxis recognized. H5 avian influenza viruses, but were unable to find virological evidence of any avian influenza viruses during Morbidity and Mortality influenza-like illnesses. However, it is possible that some severe cases have also Between 1997 and September 2015, there were nearly been missed or attributed to other diseases; thus, the net 850 laboratory-confirmed human infections with Asian effect of any undiagnosed cases is uncertain. Increased numbers of human infections published cases in the older adults was fatal; the other have been noted recently in Egypt, possibly due to the person recovered with intensive treatment. In the majority of cases, there was no virological evidence of Other avian influenza viruses exposure among patient contacts who developed influenza With the exception of the H7N9 viruses in China, most like signs. Some initial serological studies found no H7N9 327 workers infected with an H10N7 virus in Australia, but reactivity among poultry market workers, healthcare staff, 261, 417, 419, 599-601 H10N8 viruses caused fatal infections in two elderly patient contacts and other populations. However, several surveys have now detected antibody titers A young woman infected with an H6N1 virus in China had to H7N9 viruses in up to 17% of poultry workers or live evidence of lower respiratory tract complications, but bird market workers, with two studies documenting recent 316, 317 354, 547-549 recovered with treatment. These studies report unrecognized infections may be suggested by the that seroprevalence rates are low (1%) in the general 547, 548 occurrence of antibodies to various subtypes, generally at a population, with one survey also documenting low 354 low prevalence, in people who are exposed to poultry or seroprevalence in veterinarians (2%). Susceptibility (and/or reactivity with other H7 viruses that may circulate in seroconversion) might differ between viruses: 3. As a result, some authors have suggested that the were identified in serum samples collected during H7N1 overall case fatality rate in all symptomatic cases might be 606 epidemics from 1999-2002. Rare seroconversion to H6, as low as <1% to 3%, if milder cases are also accounted for; H7 and H12 viruses was reported in prospective studies of however, such estimates currently have a high degree of 260, 550 adults with poultry exposure in Cambodia and rural uncertainty. H9N2 avian influenza viruses Clinical cases caused by Eurasian lineage H9N2 Internet Resources viruses have mainly been reported in children. Fact Sheet immunocompromised infant, have been mild, and were Avian Influenza followed by uneventful recovery. Avian bird market workers in Hong Kong, and 48% of poultry Influenza workers in Pakistan. Ecology of influenza virus Terrestrial Animals in wild bird populations in Central Asia. Understanding the complex pathobiology of high pathogenicity avian influenza viruses in birds. Summary and assessment as of 4 September N, Payungporn S, Theamboonlers A, Chutinimitkul S, 2015. Studies of pathogenic avian influenza virus (H5N1) outbreak in captive H5N1 influenza virus infection of pigs by using viruses wild birds and cats, Cambodia. Chen Y, Zhong G, Wang G, Deng G, Li Y, Shi J, Zhang Z, the pathogenicity of avian and swine H5N1 influenza viruses Guan Y, Jiang Y, Bu Z, Kawaoka Y, Chen H. Genetic analysis of influenza A virus (H5N1) Avian influenza prevalence in pigs, Egypt. Avian flu finds new mammal a novel reassortant H5N1 avian influenza A virus in a zoo hosts. Genetic and biological characterization lesions and antigen of highly pathogenic avian influenza of two novel reassortant H5N6 swine influenza viruses in virus A/Swan/Germany/R65/06 (H5N1) in domestic cats mice and chickens. Hai-Xia F, Yuan-Yuan L, Qian-Qian S, Zong-Shuai L, Feng and reassortant virus genotypes. Manual of characterization of a novel influenza A virus H5N2 isolated diagnostic tests and vaccines for terrestrial animals [online]. Vet Sci Tomorrow introduction of a pair of di-basic amino acid residues at the [serial online]. Available at: cleavage site of the hemagglutinin and consecutive passages. Influenza virus evolution, host influenza virus of H10 subtype that is highly pathogenic for adaptation, and pandemic formation. Origins and evolutionary genomics with engineered polybasic cleavage site displays a highly of the 2009 swine-origin H1N1 influenza A epidemic. Avian influenza virus hemagglutinins H2, H4, H8, and H14 Experimental infection of dogs with avian-origin canine support a highly pathogenic phenotype. Review of the highly R, Prakairungnamthip D, Suradhat S, Thanawongnuwech R, pathogenic avian influenza outbreak in Texas, 2004. History and epidemiology of swine influenza in immunity to influenza A virus: where do we stand North Atlantic migratory bird flyways Asian H5N1 high pathogenicity avian influenza. Use of vaccination in genomic diversity to optimize surveillance plans for North avian influenza control and eradication. Genetic structure of avian influenza viruses from ducks of the Atlantic flyway of North 76. Surveillance of pathogenic avian influenza viruses isolated from northern Charadriiformes in northern Australia shows species pintails (Anas acuta) in Alaska: examining the evidence variations in exposure to avian influenza virus and suggests through space and time. Interspecies transmission of influenza viruses from gulls in the northern hemisphere. Emergence of a new swine H3N2 North American gull influenza virus lineage: drift, shift and and pandemic (H1N1) 2009 influenza A virus reassortant in stability. Are seals frequently A viruses and detection of antibodies in common herons infected with avian influenza viruses Chen H, Deng G, Li Z, Tian G, Li Y, Jiao P, Zhang L, Liu Z, gulls, the Netherlands, 2006-2010. Tolf C, Bengtsson D, Rodrigues D, Latorre-Margalef N, sea ducks in the Western Hemisphere. Genomic analyses detect Eurasian-lineage surveillance of influenza A virus in Portuguese waterfowl. Prevalence and subtypes of influenza A viruses Complete genome sequence of a reassortant H14N2 avian in wild waterfowl in Norway 2006-2007. Evidence that life history characteristics of wild birds influence infection and exposure to influenza A viruses. Influenza A viruses in American white pelican (Pelecanus Influenza Other Respir Viruses. Influenza A viruses in wild birds of the Howey A, Wilcox B, Hall J, Niles L, Dey A, Knutsen G, Pacific flyway, 2005-2008. Vaccination of chickens against H5N1 H1N1 and H3N2 triple reassortant influenza avian influenza in the face of an outbreak interrupts virus vFiebig2011iruses. Pathogenicity of a highly pathogenic pathogenic avian influenza A(H5N8) viruses, South Korea, avian influenza virus, A/chicken/Yamaguchi/7/04 (H5N1) in 2014. Wild bird surveillance around outbreaks of Kong-origin H5N1 avian influenza virus in four passerine highly pathogenic avian influenza A(H5N8) virus in the species and budgerigars.
The most frequent etiology of acute pancreatitis in pregnancy is biliary caused by gallstones or sludge (Wang et al virus kids are getting cheap 250mg amoxil with mastercard. Rarely it could be best natural antibiotics for acne order amoxil australia, also bacteria joke generic amoxil 1000 mg amex, caused by hyperparathyroidism bacteria yersinia enterocolitica purchase amoxil 500 mg with mastercard, connective tissue diseases bacteria weight loss safe amoxil 650mg, abdominal surgery antimicrobial 10 purchase amoxil 1000mg fast delivery, infections (viral, bacterial or parasitic), blunt abdominal injuries or could be iatrogenic caused by medications (diuretics, antibiotics, antihypertensive drugs) (Wang et al. In pregnancy gallstones and sludge induce most of the cases of acute pancreatitis, they cause duct obstruction with pancreatic hyperstimulation that increases pancreatic duct pressure, trypsin reflux and activation of trypsin in the pancreatic acinar cells. This leads to enzyme activation within pancreas and causes autodigestion of the gland, followed by local inflammation. Pregnancy does not primarily predispose the pregnant woman to pancreatitis, but it does increase the risk of cholelithiasis and biliary sludge formation (Ramin et al. Theoretical reasons for the association of pregnancy and biliary tract diseases include increased bile acid pool size, decreased enterohepatic circulation, decreased percentage of chenodeoxycholic acid, and increased percentage of cholic acid and cholesterol secretion and bile stasis (Scott, 1992). Moreover, the steroid hormones of pregnancy decrease gallbladder motility (Ramin et al. Progesterone is a smooth muscle cell inhibitor that provokes gallbladder volume increase and slows emptying (Ramin et al. Estrogens increase cholesterol secretion and minimally alter gallbladder function (Ramin et al. Also in the third trimester when the acute pancreatitis is most frequent, the uterus is enlarged and intrabdominal pressure on the biliary ducts is increased (Berk et al. Clinical features Acute pancreatitis presents essentially in the same way during pregnancy as in the non pregnant state. However, it is difficult to diagnose acute pancreatitis by history and physical examination because of similarity to many acute abdominal illnesses. The symptoms of gallbladder disease can be present or can precede the clinical presentation of acute pancreatitis. The symptoms include abdominal pain (colicky or stabbing) which may radiate to the right flank, scapula and shoulder. Other symptoms of gallbladder disease include anorexia, nausea, vomiting, dyspepsia, low-grade fever, tachycardia and fatty food intolerance (Ramin et al. Abdominal tenderness is often found; in diffuse peritonitis muscle rigidity can be present. In severe pancreatitis the general physical examination may reveal abnormal vital signs if there are third-space fluid losses and systemic toxicity. Due to hypovolemia tachycardia up to 150/min and low blood pressure could be found. Also, because of severe retroperitoneal inflammatory process temperature may increase. Dyspnea, tachypnea and shallow respirations resulting with hypoxemia may be present. Acute fetal hypoxia activates some compensatory mechanisms for redistribution of blood that enable fetus to achieve a constancy of oxygen consumption in the fetal cerebral circulation and in fetal myocardium. Redistribution of blood to vital organs enable fetus to survive for moderately long period of limited oxygen supply, but during more severe or sustained hypoxemia, these responses were no longer maintained and decompensation with fetal tissue damage and even fetal death may occur (Crisan et al. Some physical findings point to a specific cause of acute pancreatitis: jaundice in biliary origin, spider angiomas in alcoholic or xanthomas and lipemia retinalis in hyperlipidemic pancreatitis. Diagnosis Acute pancreatitis in pregnancy is diagnosed by symptoms already described, by laboratory investigations and imaging methods. The total serum amylase level rises within 6 to 12 hours of onset of the disease, usually remain elevated for three to five Acute Pancreatitis During Pregnancy 49 days. Serum lipase is elevated on the first day of ilness and remains elevated longer than the serum amylse. Specificity of serum lipase is greater than amylase, lipase level is normal in salivary gland disorder, tumors, gynecologic conditions and familial macroamylasemia. Calculation of an amylase to creatinine clearence ratio may be helpful in pregnancy, ratio greater than 5% suggests acute pancreatitis (Augustin&Majerovic, 2007). Treatment consists of fluid restoration, oxygen, analgetics, 50 Acute Pancreatitis antiemetics and monitoring of vital signs. Important additional measures during pregnancy include fetal monitoring, attention to the choice of medications and positioning of the mother to avoid inferior vena cava constriction. Ten percent of patients have severe course, and they are best managed in an intensive care unit. The third space fluid sequestration is the most serious hemodynamic disorder leading to hypovolemia and organ hypoperfusion resulting in multiple organ failure. In volume-depleted patients the essential treatment modality is initial infusion of 500 to 1000 mL of fluid per hour (Gardner et al. Monitoring of hydration, cardiovascular, renal and respiratory functions is important for early detection of volume overload and electrolyte disturbances (Forsmark & Baillie, 2007). Many pharmacological agents (somatostatin, octreotide, n-acetyl-cystein, gabexate mesylate, lexipafant and probiotics) have been investigated in acute pancreatitis, but because most of them have failed to show a positive effect they should be avoided in pregnancy. Cessation of oral feeding has been thought to suppress the exocrine function of pancreas, and to prevent further pancreatic autodigestion. Mild cases of acute pancreatitis do not need nutritional support, as the clinical course is usually uncomplicated and a low-fat diet can be started within 3 to 5 days. Treatment of severe necrotising pancreatitis should include enteral feeding by nasojejunal tube and if needed, should be supplemented by parenteral nutrition (Meier et al. Prophylactic use of antibiotics is very controversial and the choice of antibiotic in pregnancy is difficult. There are concerns with regarding to the antibiotic being tranplacentally transferred to the fetus with a risk of teratogenicity. The use of prophylactic antibiotics in severe acute pancreatitis remains controversial. The available evidence demonstrates that antibiotic prophylaxis might have a protective effect against non-pancreatic infections, but failed to show a benefit on reduction of mortality, infected necrosis and need for surgical intervention (Bai Y et al. Due to the lack of evidence on beneficial effect of antibiotics, an even more conservative approach is recommended in pregnancy. Risk of conservative treatment include risk to the fetus due to recurrent episodes, complications of gallstones, risk of malnutrition caused by lack of oral intake. Conversely, surgical treatment carries risk to the fetus from surgery and anaesthesia and risk specific to laparoscopic surgery. Laparoscopic cholecystectomy (once considered contraindicated during pregnancy) (Gadacz & Talamini, Acute Pancreatitis During Pregnancy 51 1991), is today, probably, the best treatment for the patients failed to respond to conservative management or because of recurrent episodes (Cosenza et al. Benefits of laparoscopy during pregnancy appear similar to those non pregnant patients including less postoperative pain, less postoperative ileus, significantly reduced hospitalization, decreased narcotic use and quick return to a regular diet and faster recovery. Other advantages of laparoscopy include less manipulation of the uterus and detection of other pathology that may be present and because of early mobility reduced risk of postoperative deep vein thrombosis (Date et al. Cholecystectomy is considered safe at all stages of pregnancy, and may be performed in any trimester of pregnancy without any increased risk to the mother or fetus (Cosenza et al. Historical recommendations to delay surgery until the second trimester or gestational age limit of 26 to 28 weeks of pregnancy have been refuted. Laparoscopy in pregnancy was conected with the fear of damage to the gravid uterus upon Veress or troacar insertion, technical difficulty in performing the surgery with the presence of an enlarged, gravid uterus and the concern of fetal acidemia due to decreased uterine blood flow because of increased intraabdominal pressure from insufflation and possible fetal carbon dioxide absorption (Wang et al, 2009). Recent reports suggest that the risk of fetal wasting and teratogenicity from gastrointestinal operation during pregnacy is minimal (Barone et al. However, some precautions should be followed: the use of an open technique for the insertion of the umbilical port, avoiding high intraperitoneal pressures, using of left lateral position to minimize aortocaval compression, avoiding rapid changes in the position of the patient and using electrocautery cautiously and away from uterus (Date et al. While sterile necrosis is treated conservatively, infected necrosis requires the use of antibiotics and surgical necrosectomy. Patients with infected necrosis should be treated surgically within 3 to 4 weeks after the onset of symptoms. Minimal invasive surgical techniques are new in the management of acute pancreatitis with only a few relatively small series reported to date (Van Santvoort et al. A diagnostic and therapeutic alghorytm for acute pancreatitis in pregnancy is proposed in Diagramm 1 (Stimac & Stimac, in press) 5. Outcome Prognosis for women with mild disease who respond to conservative management is excellent for mother and fetus. However, for more severe form of disease, mother mortality and fetal morbidity and mortality rates increase. In 1973 Wilkinson reviewed 98 cases of acute pancreatitis during pregnancy, 30 patients died (Wilkinson, 1973). Recently, the percentage of fatal outcomes of acute pancreatitis has been less than 5% (Talukdar & Vege, 2009) and is similar in pregnancy (Hernandez et al, 2007). The mechanisms of demise include, also, placental abruption and profound metabolic disturbance, including acidosis. This highlights the importance of regular fetal monitoring and consideration of delivery if the maternal disease is deteriorating. Diagnostic and therapeutic alghorithm acute pancreatitis in pregnancy Acute Pancreatitis During Pregnancy 53 6. Conclusions Acute pancreatitisis is a rare entity in pregnancy, mainly caused by gallbladder disorders, in which symptoms of cholelithiasis and biliary sludge in many cases precede the symptoms and clinical picture of acute pancreatitis. Diagnosis is based on clinical presentation, laboratory investigations and imaging methods performed with precaution because of potential radiation risk to the fetus. Although treatment of acute pancreatitis during pregnancy is similar to general approach in acute pancreatitis patients, a multidisciplinary team consisting of gastroenterologist, gastro intestinal surgeon, radiologist and obstetrician should be included in the treatment and follow up of these patients. A review of the management of gallstone disease and its complications in pregnancy. Antibiotic prophylaxis is not protective in severe acute pancreatitis: a systematic review and meta-analysis. Videoscopic assisted retroperitoneal debridement in infected necrotizing pancreatitis. Acute pancreatitis in pregnancy: a review of 98 cases and a report of 8 new cases. Sanchez-Ramirez2 and Mariana Gomez-Najera3 1Instituto de Nutricion Humana, Centro Universitario de Ciencias de la Salud, Departamento de Clinicas de la Reproduccion Humana, Crecimiento y Desarrollo Infantil, Universidad de Guadalajara. Guadalajara Jalisco, 2Universidad de Colima, Facultad de Medicina, Colonia Las Viboras, Colima, Col 3Division de Pediatria, Hospital de Gineco-Pediatria # 48, Centro Medico del Bajio, Avenida Mexico e Insurgentes, Colonia Los Paraisos, Leon Guanajuato Mexico 1. Introduction Decades ago acute pancreatitis was thought to be an unusual disease in children; therefore the diagnosis was delayed or even misdiagnosed. Recent published information regarding its incidence, etiological factors and clinical characteristics suggest two important issues: its prevalence and incidence seem to increase in the last decade and the concept of a benign entity has been challenged by the high proportion of cases with necrotic-hemorrhagic lesions demonstrated by image studies and the relatively frequent occurrence of relapses (1, 2). It is not clear if these published data mean an actual increasing incidence or reflect the fact that pediatricians are testing more frequently for this disease. Definition the National Library of Medicine defines pancreatitis as an inflammatory disorder of the pancreas. According to its evolution, pancreatitis may be classified as acute when it lasts days or a few weeks and is a reversible process. The term recurrent is used when more than one episode of acute pancreatitis occurs. Chronic pancreatitis implies the presence of pancreatic morphologic changes and losses of the exocrine and endocrine function that are not reversible. Pathophysiology and etiology Pancreatitis results from injury and inflammation of the pancreas that may be extended to peri-pancreatic tissues and remote organs. The process requires an initiating event that 56 Acute Pancreatitis triggers the acinar cells and activates the intracellular trypsinogen and other digestive enzymes. The resultant acinar cell damage produces pancreatic edema and a local inflammatory response associated with the release of inflammatory mediators (6, 15-17). In most cases of pancreatitis more than one etiological factor may be indentified; from this point of view pancreatitis is better defined as a complex multifactorial disease (Figure 1). Studies performed in adults have described that the prevalence of the etiological factors have changed with time: the frequency of alcoholic induced chronic pancreatitis has decreased, biliary tract disease accounts for a higher percentage and etiologies as autoimmune and particularly hereditary/genetic pancreatitis are reported with increasing frequency (17-19). The etiological factors identified in some pediatric series are described in Table 1; the most common are biliary tract disease (cholelitiasis, lithogenic bile, choledocal cyst, sphincter of Oddi dysfunction), abdominal trauma, drug ingestion and viral infections. The family history of pancreatitis is an important etiological factor that has to be asked, since hereditary pancreatitis may be defined as two patients with history of pancreatitis within one generation or more than two patients in more than one generation (20). Recent evidence suggests that a significant proportion of cases with idiopathic pancreatitis, particularly recurrent and chronic, may be associated to mutations. This means that trypsin activation and prolonged survival inside the acinar cell leads to pancreatitis due to a Pancreatitis in Children 57 premature trypsinogen activation and persistent trypsin activity as being key initiators of pancreatic injury, because all of the zymogens are activated by trypsin and thereby increase susceptibility to acute and chronic pancreatitis (29). Family Drug Sistemic Author Year n Biliary Anatomic Trauma Metabolic Infectious GeneticIdiopathic history ingestion disease Mao-Meng 2002 61 11. The detection of mutations in the genes associated to pancreatitis is important since it has been demonstrated by other authors that the interaction of environmental and genetic factors. The majority of the cases with mutations in genes associated to pancreatitis get ill in childhood. However, in a significant number of cases the definite signs of chronic pancreatitis may be found only after a long follow-up period. In addition, it has been demonstrated a geographical variation regarding etiology, particularly genetic variants. The genetic variants (20) performed in pediatric population are very few compared to the studies performed in adult population. The mutations associated to pancreatitis that have been identified in some pediatric series are described in Table 2. It is important to highlight that genetic testing in children with pancreatitis is not only useful for diagnosis but also as a predictive factor as it helps to identify individuals at risk for a more severe course of the disease. Clinical, laboratory and image data A summary of studies that report the frequency of the symptoms and signs in children with pancreatitis is presented in Table 3. The most common symptoms were abdominal pain followed by vomiting; in our series, ileus reached almost one-half of the cases studied (1, 39, 40). Abdominal pain is less commonly observed in children younger than 2 years, since it may be manifested by irritability (24, 41).