Stefan C. Bertog, MD
- Interventional Cardiology Veterans Administration Medical Center,
- University of Minnesota, Minneapolis, MN, USA
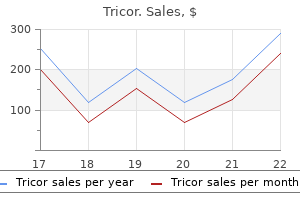
Chief cholesterol levels stress purchase tricor 160 mg with visa, Developmental Disabilities Branch National Center on Birth Defects & Developmental Disabilities Centers for Disease Control & Prevention Advocacy/Consumer Mindy Aisen cholesterol journal articles purchase tricor with a visa, M cholesterol ranges hdl cheap tricor 160mg visa. Co-Director cholesterol levels symptoms order tricor 160 mg without prescription, National Center for Family/Professional Partnerships Children & Youth with Special Health Care Needs Director cholesterol free diet chart in urdu purchase discount tricor on-line, National Programs cholesterol reducing food chart order tricor with a mastercard, Family Voices, Inc. Clinical Instructor of Pediatrics, University of Rochester Medical Center Medical Director, Excellus BlueCross BlueShield Julie Ward Director, Health Transportation & Policy Disability Policy Collaboration the Arc & United Cerebral Palsy Professional/Clinical Robert Baumann, M. Professor of Neurology and Pediatrics, University of Kentucky American Academy of Neurology Brian Faux, M. Co-Director, Cerebral Palsy Program Medical Director, Gain Analysis Laboratory Alfred I. Developmental Pediatrics University of Virginia Health System A-3 Academic Peter Blasco, M. Director, Neurodevelopmental Clinical & Training Programs Oregon Health & Science University Suzanne Bronheim, Ph. Associate Professor of Pediatrics National Center for Cultural Competence, Georgetown University Deborah Gaebler-Spira, M. Professor of Pediatrics and Physical Medicine & Rehabilitation Northwestern Feinberg School of Medicine Director, Cerebral Palsy Program Rehabilitation Institute of Chicago Susan Harris, Ph. Professor Emerita of Physical Therapy University of British Columbia Laurens Holmes, Jr. Board Certified Public Health Clinical Epidemiologist Cerebral Palsy Research, Training & Education Program A. Assistant Professor of Pediatrics Johns Hopkins School of Medicine Director, Center for Spina Bifida & Related Conditions Kennedy Krieger Institute Jeffrey Okamoto, M. Professor of Physical Therapy & Rehabilitation Sciences Drexel University College of Nursing & Health Professions Peter Rosenbaum, M. Literature Search and Retrieval Process the state of the existing literature will help to identify which systematic reviews will be helpful to guide future research. Therefore, the purpose of our literature search was to identify existing systematic reviews, guidelines and meta-analyses only. Therapeutic areas, research foci and outcomes not identified in our search, but considered important by stakeholders may be priorities for future systematic reviews. We also employed indexing terms when possible to exclude undesired publication types. We searched PubMed from 1999 forward and employed search strategies to retrieve reviews and guidelines on cerebral palsy, including spastic diplegia, quadriplegia, and hemiplegia; congenital diplegia, quadriplegia, and hemiplegia; static encephalopathy; and choreoathetosis. After input from the stakeholder identified additional areas of particular interest, we conducted a second search and added additional documents. Our second search included search strategies regarding issues deemed important by stakeholders, such as psychotherapy, physical fitness, quality of life, pain, comorbidities, transitions, cultural diversity, follow-up studies, and technologies. Search Terms and Article Selection Our search was executed on May 21, 2010, and was updated on October 15, 2010. Below (Tables B-1 and B-2) are our search terms and the yield from the PubMed database for both dates. Since we are not conducting a full review at this time, and therefore not reviewing original research, we identified 151 relevant articles that consisted of guidelines, consensus statements, meta-analyses, and systematic reviews. We identified 2, 602 primary literature citations, 527 of which were added from our second search. Existing Guidelines, Consensus Statements, and Meta-Analyses From an electronic database literature search, we retrieved guidelines, consensus statements, and meta-analyses for the treatment and prevention of cerebral palsy. Diazepam and tizanidine are effective in the short-term for generalized spasticity, although one study warns that benzodiazepines may cause 7, 12 physiologic addiction and tolerance and require an increased dose. Furthermore, there is insufficient data on dantrolene and oral baclofen, although studies differ on the use of intrathecal baclofen, with one study citing insufficient data on intrathecal baclofen, and another 7, 9 recommending its use as the treatment of choice for spastic tetraparesis. Notably, there is little data regarding functional outcomes and side effects for any of the pharmacologic treatments. One guideline and one consensus statement specifically address rehabilitation therapies, physical therapy, physiotherapy, and occupational therapy. These guidelines and statements were composed by a Mac Keith Multidisciplinary Meeting and the Italian Society of Physical & 4, 5 Rehabilitation Medicine with the Italian Society of Child and Adolescent Neuropsychiatry. The Mac Keith consensus statement focuses on postural therapy and the timing of postural 4 therapy, as well as on monitoring hips for subluxation. The Italian guidelines recommend 5 consideration of therapies based on the characteristics of the subject. Three guidelines and consensus statements focus on spasticity and surgical interventions, with two publications from 1, 9, 10 University of Florida and another from the Semmes-Murphy Clinic. These papers recommend that surgery be completed early in life if possible (4-7 years), that tendon lengthening be used to manage some severe spasticity and soft-tissue complications, and that 1, 10 tendon transfer be used sparingly and only by well-trained surgeons. Four guidelines and consensus statements address spasticity from a holistic perspective, discussing aspects of pharmacology, surgery, rehabilitation, etc. These papers come from the Committee on Children with Disabilities, Washington University School of Medicine with the St. Practice guidelines & consensus statements Reference Year Organization Population Intervention(s) Summary Focus 7 Delgado et al. Practice guidelines & consensus statements (continued) Reference Year Organization Population Intervention(s) Summary Focus 2 Tilton and Maria 2001 University of children with pharmacotherapy: oral essential elements of a comprehensive approach to treatment Florida spasticity (baclofen, tizanidine, include a) recognition that there are multiple treatment and benzodiazepine) & modalities available b) an initial multidisciplinary evaluation of botulinum toxin the patient with regular re-evaluations to meet the changing needs of the patient c) individualized treatment plan d) plan with concise, explicit, short and long-term goals embraced by patient, family, and health care providers factors affecting choice of therapeutic modality: focal or generalized spasticity, comorbidities, cost, age, dosing, compliance adherence, side effects, prior reaction, past options C-9 Table C-2. Contents (up to April 2007) botulinum neurotoxin should be offered as a treatment option for the treatment of spasticity in adults and children future research: Studies should investigate factors that predict which patient subgroups have optimal response. Final outcome is posture/gait improvement, but formal evidence is still lacking in order to establish the real benefit of physical and occupational therapy in the rehabilitation of equinus foot patients. More work is technology assessment reports, or needed to tackle methodological weaknesses, such as guidelines. Agency for Healthcare Research and Quality, and the Department of Health and Human Services. Choreoathetosis Slide 4 Search Terms A second search added content identified in the stakeholder calls 1. Description of the Treatment Targets and the Organizing Framework A simplified conceptual framework can be very helpful for organizing the large body of knowledge that has been reported about cerebral palsy. Because of the current structure of available scientific research and for the sake of practicality we will focus on each treatment target separately. Other: Cognition, Seizures, Audiology, Optometry/Ophthalmology, Brain Imaging, etc. Furthermore, we fit the information for each treatment target into the following organizing framework: 1. The focus on treatment targets does not preclude the future analysis of a framework category going across multiple treatment targets. For example, do variations in the diagnostic criteria for spasticity cause delays in seeking rehabilitative therapies and negatively affect functional independence The fruitful discussion of stakeholders within the Issues Exploration Forum will identify practical questions like this that could warrant systematic review or further investigations. Botulinum toxin type A in the treatment of lower limb spasticity in cerebral palsy. Current evidence for the use of botulinum toxin type A in the management of children with cerebral palsy: a systematic review. Evidence of the effects of intrathecal baclofen for spastic and dystonic cerebral palsy. Botulinum toxin type A for the treatment of the spastic equinus foot in cerebral palsy. A systematic review of the effectiveness of strength-training programs for people with cerebral palsy. Clinical utility of botulinum toxin in the treatment of cerebral palsy: comprehensive review. Effectiveness of repeated treatment with botulinum toxin type A across different conditions. European consensus table 2006 on botulinum toxin for children with cerebral palsy. Upper-limb injections of botulinum toxin-A in children with cerebral palsy: a critical review of the literature and clinical implications for occupational therapists. Constraint-induced movement therapy in the treatment of the upper limb in children with hemiplegic cerebral palsy: a Cochrane systematic review. Oral antispastic drugs in nonprogressive neurologic diseases: a systematic review. Botulinum toxin type A injection for management of upper limb spasticity in children with cerebral palsy: a literature review. Effects of botulinum toxin type A on upper limb function in children with cerebral palsy: a systematic review. Assessment: Botulinum neurotoxin for the treatment of spasticity (an evidence-based review): report (continued) of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Surgical treatment for the thumb-in-palm deformity in patients with cerebral palsy. Botulinum toxin A as an adjunct to treatment in the management of the upper limb in children with spastic cerebral palsy. Effectiveness of physical therapy interventions for children with cerebral palsy: a systematic review. Effect of cardiorespiratory training on aerobic fitness and carryover to activity in children with cerebral palsy: a systematic review. A systematic review of the effectiveness of treadmill training and body weight support in pediatric rehabilitation. Efficacy of ankle-foot orthoses on gait of children with cerebral palsy: systematic review of literature. Efficacy of electrical stimulation to increase muscle strength in people with neurological conditions: a systematic review. An assessment of gait analysis in the rehabilitation of children with walking difficulties. Botulinum toxin type A in the management of equinus in children with cerebral palsy: an evidence-based economic evaluation. Systematic review of progressive strength training in children and adolescents with cerebral palsy who are ambulatory. Effects of partial body weight supported treadmill training on children with cerebral palsy. Treadmill training with partial body-weight support in children with cerebral palsy: a systematic review. Evaluating interventions to improve gait in cerebral palsy: a meta-analysis of spatiotemporal measures. The effect of lower limb functional electrical stimulation on gait of children with cerebral palsy. Assessment: Botulinum neurotoxin for the treatment of spasticity (an evidence-based review): report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Progressive resistance exercise in physical therapy: a summary of systematic reviews. Exercise programs for children with cerebral palsy: a systematic review of the literature. A systematic review of the effectiveness of treadmill training for children with cerebral palsy. Existing systematic reviews by treatment target (continued) Treatment Systematic Reviews Target Upper Extremity Anttila H, Malmivaara A, Kunz R, et al. Effectiveness of physiotherapy and conductive education interventions in children with cerebral palsy: a Therapy focused review. Management of upper limb dysfunction in children with cerebral palsy: a systematic review. Effectiveness of adaptive seating on sitting posture and postural control in children with cerebral palsy. Constraint-induced movement therapy in the treatment of the upper limb in children with hemiplegic cerebral palsy. Bound for success: a systematic review of constraint-induced movement therapy in children with cerebral palsy supports improved arm and hand use. A systematic review of upper extremity casting for children and adults with central nervous system motor disorders.
Normal voiding is accomplished by voluntary relaxation of the pelvic floor and urethra definition cholesterol and triglycerides buy tricor with amex, accompanied by sustained contraction of the detrusor muscle cholesterol in shrimp and oysters buy generic tricor 160 mg on-line, leading to complete bladder emptying cholesterol medication kidney failure discount tricor on line. Innervation the lower urinary tract receives its innervation from three sources: (i) the sympathetic and (ii) parasympathetic divisions of the autonomic nervous system cholesterol japanese food buy cheap tricor 160mg online, and (iii) the neurons of the somatic nervous system (external urethral sphincter) cholesterol reading discount 160 mg tricor mastercard. The autonomic nervous system consists of all efferent pathways with ganglionic synapses that lie outside the central nervous system cholesterol test explained cheap tricor amex. The sympathetic system primarily controls bladder storage, and the parasympathetic nervous system controls bladder emptying. The somatic nervous system plays only a peripheral role in neurologic control of the lower urinary tract through its innervation of the pelvic floor and external urethral sphincter. The sympathetic nervous system originates in the thoracolumbar spinal cord, principally T11 through L2 or L3 (see Chapter 6). The ganglia of the sympathetic nervous system are located close to the spinal cord and use acetylcholine as the preganglionic neurotransmitter. The postganglionic neurotransmitter in the sympathetic nervous system is norepinephrine, and it acts on two types of receptors: receptors, located principally in the urethra and bladder neck, and receptors, located principally in the bladder body. Stimulation of receptors increases urethral tone and thus promotes closure, whereas adrenergic receptor blockers have the opposite effect. The parasympathetic nervous system originates in the sacral spinal cord, primarily in S2 to S4, as does the somatic innervation of the pelvic floor, urethra, and external anal sphincter. Sensation in the perineum is also controlled by sensory fibers that connect with the spinal cord at this level. For this reason, examination of perineal sensation, pelvic muscle reflexes, and pelvic muscle or anal sphincter tone is relevant to clinical evaluation of the lower urinary tract. The parasympathetic neurons have long preganglionic neurons and short postganglionic neurons, which are located in the end organ. Both the preganglionic and postganglionic synapses use acetylcholine as their neurotransmitter, acting on muscarinic receptors. Because acetylcholine is the main neurotransmitter used in bladder muscle contraction, virtually all drugs used to control detrusor muscle overactivity have anticholinergic properties. Bladder storage and bladder emptying involve the interplay of the sympathetic and parasympathetic nervous systems. Neuropathology at almost any level of the neurourologic axis can have an adverse effect on lower urinary tract function. Micturition Micturition is triggered by the peripheral nervous system under the control of the central nervous system. It is useful to consider this event as occurring at a micturition threshold, a bladder volume at which reflex detrusor contractions occur. The threshold volume is not fixed; rather, it is variable and can be altered depending on the contributions made by sensory afferents from the perineum, bladder, colon, rectum, and input from the higher centers of the nervous system. The micturition threshold is, therefore, a floating threshold that can be altered or reset by various influences. The spinal cord and higher centers of the nervous system have complex patterns of inhibition and facilitation. The most important facilitative center above the spinal cord is the pontine-mesencephalic gray matter of the brainstem, often called the pontine micturition center, which serves as the final common pathway for all bladder motor neurons. Transection of the tracts below this level leads to disturbed bladder emptying, whereas destruction of tracts above this level leads to detrusor overactivity. The cerebellum serves as a major center for coordinating pelvic floor relaxation and the rate, force, and range of detrusor contractions, and there are multiple interconnections between the cerebellum and the brainstem reflex centers. Above this level, the cerebral cortex and related structures exert inhibitory influences on the micturition reflex. Thus, the upper cortex exerts facilitative influences that release inhibition, permitting the anterior pontine micturition center to send efferent impulses down the complex pathways of the spinal cord, where a reflex contraction in the sacral micturition center generates a detrusor contraction that causes bladder emptying. A normal lower urinary tract is one in which the bladder and urethra store urine without pain until a socially acceptable time and place arises, at which point voiding occurs in a coordinated and complete fashion. Lower urinary tract disorders include disorders of storage (such as urinary incontinence), emptying (such as urinary hesitancy and retention), and sensation (such as urgency or pain). Abnormal Storage Incontinence (symptom) the complaint of any involuntary leakage of urine Stress urinary incontinence (symptom) the complaint of involuntary leakage on effort or exertion, or on sneezing or coughing Stress urinary incontinence (sign) Observation of involuntary leakage from the urethra, synchronous with exertion/effort, or sneezing or coughing Urgency urinary incontinence (symptom) the complaint of involuntary loss of urine associated with urgency Mixed incontinence Complaint of involuntary loss of urine associated with urgency and also with effort or physical exertion or on sneezing or coughing Continuous urinary incontinence Complaint of continuous involuntary loss of urine Frequency the number of voids per day, from waking in the morning until falling asleep at night Increased daytime urinary frequency Complaint that micturition occurs more frequently during waking hours than previously deemed normal by women (traditionally defined as more than seven episodes) Nocturia Complaint of interruption of sleep one or more times because of the need to micturate (each void is preceded and followed by sleep) Nocturnal enuresis Complaint of involuntary loss of urine that occurs during sleep Urgency Compliant of sudden, compelling desire to pass urine, which is difficult to defer Postural urinary incontinence Compliant of involuntary loss of urine associated with change of body position, for example, rising from a seated or lying position Insensible urinary incontinence Compliant of urinary incontinence where the women has been unaware of how it occurred Coital incontinence Compliant of involuntary loss of urine with coitus. This symptoms might be further divided into that occurring with penetration or intromission and that occurring at organism. This definition does not take into account the wide variation in this symptom and the disruption it causes. For example, half of young nulliparous women report occasional minor urine leakage; for most this is neither a bother nor a symptom for which they would seek treatment. These women often dramatically alter their lives because of leakage, curtailing activities, social outings, and intimacy. In between these two extremes lies another one-third of adult women who report leakage at least weekly, but without the same degree of life altering severity as the women previously noted. The total annual cost to care for patients with incontinence in the United States is estimated at $11. In the United States, much of this cost is borne directly by women in the form of incontinence pads and excess laundry costs. Despite the burden imposed by leakage, many women do not discuss this symptom with a health care professional. For some women, this is because the leakage does not bother them, whereas others are embarrassed and suffer in silence. Still others do not raise this issue because they mistakenly believe the only treatment option is surgical. Studies show that there is little relationship between the volume of urine lost and the distress that it causes a patient (10). The degree to which women are bothered by leakage is influenced by various factors, including cultural values and expectations regarding urinary continence and incontinence. If the leakage is distressing to the patient, evaluation and treatment should be offered. Incontinence can almost always be improved and frequently can be cured, often using relatively simple, nonsurgical interventions. Types of Disorders Stress Urinary Incontinence Stress urinary incontinence occurs during periods of increased intra-abdominal pressure. Stress urinary incontinence is the most common form of urinary incontinence in women and is particularly common in younger women. In a survey of 144 collegiate female varsity athletes, 27% reported stress incontinence while participating in their sport (11). The activities most likely to produce urinary loss were jumping, high-impact landings, and running. Limiting their activities may eliminate the incontinence problem, but it does so at a certain cost to their quality of life. Other women learn to cope with stress incontinence by adopting new body postures during physical activities that prevent them from leaking or by strengthening their pelvic muscles to compensate for increased exertion. Other women may be profoundly relieved to find out that the small amount of leakage they experience from time to time is not abnormal. In any case, the interaction of these three biopsychosocial factors opens up a variety of strategies for the management of stress incontinence. Surgical intervention is only one strategy, and it addresses only the biologic competence of the sphincteric mechanism rather than either of the other factors that interact to produce the clinical problem. Urgency Urinary Incontinence and Overactive Bladder Although stress incontinence is the most common type of urinary continence in all women, urgency incontinence is the most common form of incontinence in older women (12). Urgency urinary incontinence is the involuntary leakage of urine accompanied by or immediately preceded by urgency. The new joint report from the International Urogynecological Association and International Continence Society recommended this symptom be called urgency urinary incontinence to differentiate between the normal urge experienced when the bladder is full from the abnormal response that may require treatment. This is a symptom-based diagnosis; the cause may or may not be detrusor overactivity, based on urodynamic observation characterized by involuntary detrusor contractions during the filling phase. Women may have other related problems such as urgency, nocturia, and increased daytime frequency. The definition of nocturia is quantifiable: the woman wakes one or more times a night to void (8). Increased daytime frequency occurs when the patient considers that she voids too often. Most women have experienced these symptoms during times of voluntary delays in voiding or increased fluid intake. However, urinary urgency implies more than just the feeling that all normal women have if they voluntarily delay voiding beyond a reasonable time (8). When a woman presents for treatment, she generally reports an intrusive, bothersome, persistent need to urinate that takes her attention away from other activities. Increased daytime frequency is often brought up as an issue when a woman experiences a change in her own voiding pattern. Data from a broader sample of women in the United States suggest that the median number of voids per day is eight, and 95% of so-called normal women void 12 or fewer times per day (14). Overactive detrusor function is defined as a urodynamic diagnosis characterized by involuntary detrusor contractions during the filling phase, which may be spontaneous or provoked. It is divided into neurogenic detrusor overactivity, resulting from a relevant neurologic condition and idiopathic detrusor overactivity, when there is no clear cause (15). The term overactive bladder syndrome is defined as urinary urgency, usually accompanied by frequency and nocturia, with or without urgency urinary incontinence, in the absence of urinary tract infection or other obvious pathology (8). It is important to note that a woman with severe urgency and a sense of impending leakage who remains dry may have the exact same bladder pathology as one with severe urgency and concomitant leakage. A woman with a strong urethral sphincteric mechanism may be able to avoid leakage during uninhibited bladder contractions, and although one with a strong sphincter may remain dry, she still may be disturbed by the urgency and impending sense of leakage. Mixed Incontinence As implied by the name, women with mixed incontinence have symptoms of both stress and urge urinary incontinence. Younger women are more likely to have stress incontinence alone, whereas in older women mixed and urge incontinence predominate. In a review of 15 population-based studies of women of all ages with urinary incontinence, a median of 49% (range 24% to 75%) had stress urinary incontinence, 21% (range 7% to 49%) had urge urinary incontinence, and 29% (range 11% to 61%) had mixed urinary incontinence (16). Functional and Transient Incontinence Functional incontinence is more common in elderly women and refers to incontinence that occurs because of factors unrelated to the physiologic voiding mechanism. A woman who cannot get to the bathroom quickly enough may often become incontinent. Functional incontinence can be related to such factors as decreased mobility, musculoskeletal pain, or poor vision. Factors leading to transient urinary incontinence are, as the name implies, medically reversible conditions. These factors argue strongly for the inclusion of a thorough medical evaluation as part of the workup of any patient with urinary incontinence. Extraurethral Incontinence Although most urinary incontinence represents unwanted urine loss through the urethra (transurethral incontinence), urine loss can also occur through abnormal openings. The congenital causes of urinary incontinence are not common and usually are easy to diagnose. The most extreme cases are caused by bladder exstrophy, in which there is a congenital absence of the lower anterior abdominal wall and anterior portion of the bladder, resulting in the entire bladder opening directly to the outside (19). Before the advent of modern reconstructive surgery, these infants usually died very early in life from sepsis. Ectopic ureter, a subtle congenital anomaly causing extraurethral urine loss, generally is detected early in life, but occasionally may escape detection until adolescence or early adulthood (20). In infancy, an ectopic ureter should be suspected when a mother seeks care for her baby, whom she says is never dry. Most commonly, the ectopic ureter drains into the vagina, but occasionally, it may drain into the urethra distal to the point of continence. A traumatic opening between the urinary tract and the outside is called a fistula. Vesicovaginal fistulas, located between the bladder and urethra, are most common, but fistulas may occur between the vagina, uterus, or bowel, and the urethra, ureter, or bladder. This was true in the Western world 150 years ago, but advances in the provision of basic obstetric services and advanced obstetric intervention have virtually eliminated this problem in developed countries. Obstructed labor can occur in rural areas where girls are married young (sometimes as early as 9 to 10 years of age) and where transportation is poor and access to medical services is limited. In such circumstances, pregnancy often occurs shortly after menstruation begins and before maternal skeletal growth is complete. When labor begins, cephalopelvic disproportion is common and little can be done to correct fetal malpresentations. Women may be in labor as long as 5 to 6 days without intervention, and if they survive, they usually give birth to a stillborn infant.
Fiber therapy should also be used with caution in patients with cognitive dysfunction (dementia) cholesterol juice recipes buy generic tricor 160mg, difficulty with ambulation list of cholesterol lowering foods diet purchase tricor 160 mg with amex, and underlying neurogenic disease for fear of worsening the condition cholesterol levels nz heart foundation tricor 160 mg free shipping. There is no evidence to substantiate the recommendation for extra water intake with fiber supplements (161) average cholesterol during pregnancy generic 160 mg tricor amex. Laxatives Laxatives are commonly used to treat constipation and disordered defecation free cholesterol test orange county cheap tricor generic. Bulk-Forming Laxatives these come in natural forms (psyllium) as well as synthetic form (Metamucil cholesterol derivatives purchase cheap tricor, Konsyl, Citrucel) and are felt to be the safest laxatives. Hyperosmolar Laxatives these consist of poorly absorbed substances that increase intraluminal osmolarity and water absorption. Emollient Laxatives these agents are divided into two subsets: docusate salts and mineral oil. The docusate salts have hydrophilic and hydrophobic properties similar to detergents. They soften stool and decrease surface tension by increasing stool water and lipid content. Examples include docusate calcium (Surfak), docusate potassium (Dialose, Kasof), and docusate sodium (Colace, Comfolax). They also improve the absorption of other laxatives and are combined in preparations with stimulant laxatives such as Correctol, Peri-Colace, and Feen-a-Mint. The limited absorption of mineral oil allows it to penetrate and soften the stool. Prolonged daily use can lead to decreased absorption of the fat-soluble vitamins A, D, E, and K. Use of mineral oil should be avoided in elderly and debilitated patients, as well as in those with esophageal motility disorders because of the potential for aspiration pneumonia. Saline Laxatives these usually contain magnesium cations and phosphate anions that are relatively nonabsorbable and produce an osmotic gradient with increased water absorption. Examples include magnesium citrate, magnesium hydroxide (Milk of Magnesia), magnesium sulfate, sodium phosphate, and biphosphate (Phospho-soda, Fleet enema). Stimulant Laxatives these are found in three basic types: castor oil, anthraquinones, and diphenylmethanes. A metabolite of castor oil, ricinoleic acid, increases intestinal motility and secretion. Anthraquinones (cascara sagrada, senna [Senokot], casanthranol [aloe], and danthron) are absorbed by the small intestine and stimulate motility by increasing intraluminal fluid and electrolyte content. Diphenylmethanes (phenolphthaleins [Feen-a-Mint, Correctol] and bisacodyl [Dulcolax]) have a mechanism of action similar to anthraquinones. These agents are potent and are intended for short-term use in cases refractory to bulk or osmotic laxatives. It has been a long-standing belief that prolonged use can lead to a dilated atonic colon known as cathartic colon syndrome, melanosis coli, or neuronal degeneration. A recent article refutes the theory that stimulant laxatives damage the autonomic nervous system when used at recommended doses (151). Prokinetic Agents Medications that stimulate gastrointestinal motility primarily through neuromodulation of acetycholine levels include metoclopramide, cisapride, cholinergic agonists (bethanechol), cholinesterase inhibitors (neostigmine), and serotonin agonists. Behavioral Approaches Behavioral techniques such as biofeedback and bowel regimens may have a role in certain conditions associated with constipation and defecatory dysfunction. Overall, these approaches have far less application to disordered defecation than to fecal incontinence. Bowel regimens in conjunction with laxatives, suppositories, and enemas can facilitate emptying by optimizing the gastrocolic reflex and increased peristaltic activity. The efficacy of bulking agents for this condition is controversial, and many studies, including meta-analyses, exhibit an effect similar to placebo. However, patients may experience exacerbation of bloating and abdominal discomfort with fiber therapy. They can be useful as adjunctive treatment options, but can also exacerbate abdominal pain and discomfort. No episodes of ischemic colitis or cardiac toxicity have been reported with the use of this medication, and the most common side effects are diarrhea and headache. Colonic Inertia and Slow-Transit Constipation Patients with slow-transit constipation tend to respond poorly to fiber supplementation, although most have already tried an empiric trial of fiber before testing to confirm the diagnosis (160). Some patients may benefit from regular toileting, either in the morning or after meals when there is increased colonic motor activity. Biofeedback may have modest short-term benefits, but the long-term effect is questionable (168). It is also reasonable to attempt a trial of any of the laxatives listed in Table 28. Stimulant laxatives are commonly used, but questions remain about the development of neuronal degeneration with prolonged usage. Data regarding laxative use for this condition have failed to show a significantly better response than placebo. Currently there is only one available prokinetic agent, tegaserod, approved for the treatment of constipation that improves colonic transit. They have not been shown to have greater efficacy when compared with placebo, and their role in the treatment of dyssynergic defecation remains uncertain. Specific treatment for this condition tends to focus on biofeedback because of studies indicating that this is an acquired behavioral disorder of defecation. Modalities such as diaphragmatic muscle training, simulated defecation, and manometric or electromyography-guided anal sphincter and pelvic muscle relaxation have been employed independently or combined with other techniques. These techniques have yielded symptomatic improvement in approximately 60% to 80% of patients. Many patients with dyssynergic defecation also have abnormal rectal sensation, so rectal sensory conditioning may provide additional benefit (33, 49, 169, 170). Others have tried botulinum toxin injections to paralyze the puborectalis and anal sphincter muscle. Small case series have shown modest early improvement, but the results do not appear to be long lasting (171, 172). A recent randomized trial of 48 participants comparing botulinum toxin to biofeedback retraining found better initial improvement with the botulinum toxin (70% vs. Pessary for Treatment of Pelvic Organ Prolapse Pessaries of various shapes and sizes have been used for centuries to treat pelvic organ prolapse (174). They are a safe alternative to surgery, with the most common complications being increased vaginal discharge and erosion or ulceration of the vaginal wall. Although pessaries represent a common therapeutic modality, there are limited data regarding fitting and management (175). Even less is known about which type of pessary is better for enteroceles and rectoceles, although the site of prolapse does not appear to affect the ability to retain a pessary (176). Some of the space-occupying pessaries, such as the Gellhorn and cube, use a suction mechanism to maintain vaginal retention, whereas others, like the donut, do not. In theory, space occupying pessaries and those that exert forces against the posterior wall and vaginal apex (donut, inverted Gehrung) should aid in treatment of rectoceles and enteroceles. However, there are few data regarding the efficacy of pessaries for relieving symptoms of disordered defecation. The only randomized crossover trial comparing different types of pessaries (ring and Gelhorn) found improvement in quality-of-life measures with each pessary that did not differ. More research is needed to determine the role of pessaries for treatment of rectoceles and enteroceles as well as symptoms that are likely to be improved using a pessary. Surgical Treatment Following is a review of the efficacy of various surgical treatments for specific conditions associated with constipation and disordered defecation. Slow Transit/Colonic Inertia Subtotal colectomy with ileosigmoid or ileorectal anastomosis is considered by many to be the surgical treatment of choice for slow-transit constipation refractory to medical management. Most surgeons restrict the use of this surgical procedure to the most extreme cases and typically operate on fewer than 10% of patients. Strict criteria for surgery include the following: chronic, severe, disabling symptoms unresponsive to medical therapy; slow transit in the proximal colon; no evidence of pseudo-obstruction; and normal anorectal function (162). An extensive review of colectomy for slow-transit constipation analyzed 32 studies from 1981 to 1988 and found satisfaction rates ranged from 39% to 100% (180). Superior outcomes occurred in those who had a complete physiologic evaluation and proven slow-transit constipation. Patients with anismus had higher rates of recurrent symptoms and lower satisfaction levels (181). Poorer outcomes occurred with ileosigmoid and cecorectal anastomosis than with ileorectal anastomosis. None of the studies had a comparison group, and outcomes were variable and lacking validated measures. A quality-of-life study revealed that the score correlated poorly with frequency of bowel movements. However, a lower score was seen in those patients who had persistent abdominal pain, diarrhea, fecal incontinence, and permanent ileostomies. Overall satisfaction with the procedure was very high and correlated with the quality-of-life score (183). Surgical alternatives to subtotal colectomy include ileostomy, cecostomy with antegrade continence enemas, and sacral nerve stimulation. Subtotal colectomy has never been directly compared with ileostomy, but those who had a permanent diversion after subtotal colectomy had lower quality-of-life scores. Patients undergoing cecostomy with antegrade continence enemas can expect to have satisfactory function approximately half of the time, with most requiring additional revision procedures secondary to stomal complications (184). Pelvic Organ Prolapse the variety of surgical treatment techniques for the repair of rectocele include posterior colporrhaphy, defect-directed repair, posterior fascial replacement, transanal repair, and abdominal repair with sacral colpopexy. In cases of perineal descent, abdominal sacral colpoperineopexy is the procedure of choice. Suture rectopexy can be performed in conjunction with sacral colpoperineopexy if rectal prolapse is present. Despite the routine use of these procedures, data are limited regarding symptomatic improvement of disordered defecation. Greater detail regarding the specific techniques for many of these procedures is provided in Chapter 27 this section will focus on surgical outcomes, including anatomic cure of prolapse, improvement of defecatory dysfunction symptoms, and morbidity associated with the procedure. Posterior Colporrhaphy Posterior colporrhaphy has been the surgical procedure for rectocele repair preferred by gynecologic surgeons for more than 100 years. Traditional posterior colporrhaphy narrows the vaginal caliber through plication of the rectovaginal septum and usually includes a perineorrhaphy, which narrows the introitus. Despite it broad use, there are few data regarding long-term anatomic success, symptomatic improvement, and sexual function following the procedure. In these studies, the procedure was ineffective at treating constipation, vaginal digitations (splinting), and fecal incontinence. As early as 1961, high rates of dyspareunia have been reported with this procedure in as many as 50% of patients (208). However, a recent prospective case series of 38 women undergoing posterior colporrhaphy along with concomitant procedures for rectocele and obstructed defecation revealed markedly different results (209). Fascial plication was performed without levator plication, and perineal body reconstruction rather than routine perineorrhaphy was employed when indicated. There was significant improvement in preoperative and postoperative symptoms for constipation (76% vs. There was no difference in fecal incontinence and only one case of de novo dyspareunia. The authors attribute their improved anatomic and functional outcomes and combined improvement in dyspareunia to exclusion of levator plication, perineorrhaphy, and excision of vaginal epithelium. An additional benefit may be derived during mobilization of the vaginal epithelium, when scar tissue from prior episiotomy or surgery is divided. They also found that preoperative defecating proctography was of limited value and have stopped its routine use as part of the preoperative evaluation for women with symptomatic rectoceles and obstructive defecation. Defect-Directed Repair the goal of a defect-directed repair or site-specific repair is to restore normal anatomy (36). This procedure can be combined with a perineal body reconstruction, if necessary, but usually does not routinely involve perineorrhaphy. Anatomic cure rates range from 82% to 100%, which are similar to those for posterior colporrhaphy. All studies reported low rates of de novo dyspareunia with good functional and anatomic outcomes, but the long-term durability of the procedure is unknown. All but one of these studies included concomitant prolapse and urinary incontinence procedures. Participants completed validated pelvic floor instruments at baseline and 6 months, 1 year, and 2 years after surgery.
Interventions included weight bearing activity cholesterol medication in the news buy tricor 160 mg low cost, use of static or dynamic standing cholesterol ratio and treatment tricor 160mg amex, vitamin D and calcium cholesterol range chart uk order tricor in india, oral or intravenous bisphosphonates high cholesterol foods healthy buy cheap tricor on line, 118 and growth hormone cholesterol test eating the day before cheapest generic tricor uk, vibrating platforms cholesterol test blood donation discount tricor 160 mg otc, vitamin K, and acupuncture. There is a paucity of validated Uncertainty/controversy regarding 112 outcomes outcome measures for sialorrhea treatment. The best way to 114 treatment incorporate those nutrients into a gastrostomy-diet is also uncertain. Assessment of pain in patients with communication difficulties or cognitive impairment 6 complicates both treatment and research. Data from typically developing children suggests that cognitive behavioral methods may be helpful as well, 120 especially for acute pain, abdominal pain, and chronic headaches. Framework F: Pain Issue Examples Availability of a strategy to Strategies to address pain include medication, relaxation, biofeedback, cognitive-behavioral therapy, training in coping skills, 120 reduce burden-Treatment hypnosis, exercise, distraction, and imagery. Variations in issues of Variations in expression of pain by patients make assessment challenging, especially when a patient has communication 6 diagnosis difficulties or cognitive impairment. Variations in diagnosis of pain may be aided by possible pain assessment tools including self-report, physiological pain, 120 behavioral pain, and distress measures. Conductive education therapy targets cognition and motor skills, but limited information is available to guide practice because there are no standard characteristics of the program, definite parameters, or baseline skill level 124 for the study population. As the children age, problems with speech and other forms of communication can further complicate communication. Sensory Sensory impairments can contribute to difficulties communicating and interfere with cognitive development (Table E-8). Variations in age distributions None Variations in sociodemographic None measures E-45 Table E-8. However, the routine signals may make it difficult for the child to acquire a full range of 125 communication skills and take an active independent role in interaction. The few available studies indicate possible utility for assessing baseline and change over time. The manifestation of poorer functioning can also be associated with right-sided versus 123 left-sided hemiplegia. Examples of functional independence and achieving functional independence through transition from pediatric to adult care are of great importance to stakeholders from patients and families to health care providers. Basic recommendations from professional societies on transition planning for adolescents with special health care needs are rarely based on statistical evidence of efficacy; rather, they build on commonly accepted principles of transition. It is patient centered, and its cornerstones are flexibility, responsiveness, continuity, comprehensiveness, and 135 coordination. Issue Examples Availability of a strategy to Physiotherapy and speech therapy should begin as early as possible in life; it should be intensive (1 hour of therapy 4 times 5 reduce burden-Treatment more per week) and continuous, at least in early life. After 3 years, a child is eligible for special-education from a local educational agency. Learning disability was present in 40%, epilepsy in 33%, and severe visual impairment in 19% of the children. A lack of periodic health care, including breast 136 examinations and routine gynecologic care has also been reported. Also possible to have neurogenic bladder dysfunction and may require urologic consultation. Variations in clinical practice None Variations in provision of Organizations: None services Professionals: None Specialty, Primary: None Other: None Private: None Public: None E-49 Table E-9. Notably, few of the therapies have greater than case series evidence to support their use. However, there is preliminary evidence, primarily from in vitro studies and rat studies that neonatal models of hypoxic 140-142 ischemic brain injury may improve with injection of genetically engineered stem cells. Robotics Robotics have been used for several years to aid upper body mobility and dexterity for stroke 143, 144 rehabilitation. Robots have also been employed to assist with treadmill 145-148 therapy and improve the functional tasks of standing and walking. Patients stand stationary or perform dynamic movements while on the vibration platform. One hypothesis posits that the vibration platforms are able to stimulate muscle spindles and alpha-motoneurons 152 that initiate a muscle contraction. Virtual reality One systematic review of virtual reality says that the use of virtual reality (either immersion or desktop versions) has conflicting evidence of positive effects on body structures and 154 functions. There is a moderate level of evidence that virtual reality does not positively impact activity and participation. There is a moderate level of evidence that virtual reality therapy positively impacts personal factors such as motivation, volition, and interest. Welcome Pam Curtis opened the meeting, welcomed the stakeholders to the Issues Exploration Forum on Cerebral Palsy. She thanked the participants for their time and participation on the conference calls and extranet discussion. She reviewed the goals of the forum including (a) to take topics that the participants have recommended and develop a prioritized list for comparative effectiveness research with a focus on evidence synthesis, and (b) to remain mindful of the need for evidence generation in this area. Pam Curtis reviewed the meeting materials, logistics, announcements, and the process to date including results of the first two conference calls and extranet discussion board. The initial list of 88 research topic ideas generated from the conference calls and extranet discussion was presented for initial prioritization in the week prior to the meeting. He reviewed search terms and methods that identified the existing systematic reviews, guidelines and meta-analyses, noting that methods did not include review of primary research. The review consisted of published literature rather than beginning from a clinical perspective. Therefore, the input of the stakeholders was and will be key to identify what the literature does not include and to make recommendations of what topics are needed for future systematic reviews. She stressed that what is not available in systematic reviews is more important than what is there, and enables the identification of research gaps of great importance. Preliminary Prioritization of Topics to Date Pam Curtis reviewed the results of the poll to prioritize topics generated prior to the meeting. Items receiving initial high prioritization included lack of standards of care, lack of coordination of care, lack of longitudinal studies, the need for evidence-based care management frameworks, and the comparative effectiveness of treatments for spasticity. She also described the rationale for assignment of participants to small groups to ensure that the greatest possible number of concepts was discussed and a diversity of perspective was represented in each group. Participants were assured that there would be an opportunity to discuss all issues following the small group sessions. Small Group Discussions the participants divided into four small groups for further discussion on the themes of health care delivery, methods, quality of life, and interventions. The health care delivery work group discussed issues related to standards of care as well as translation and application of evidence. The Methods Work Group should consider these issues and highlight the need to use observational data or practice-driven data, the need to include small studies in systematic reviews, the importance of using mixed populations, and the need for long-term studies. The current process is a step backward since those experts apparently were not consulted before beginning the forum. The Methods small group confirmed and refined the following four topics as priorities for future methods work. The interventions workgroup discussed issues including surgical, feeding, communication, and durable medical equipment, lack of standardization of care, challenges of existing methodology, lack of primary evidence for synthesis, the need for standardized outcomes measurements and the need for guidelines and best practices for all interventions. There is no standardization of what outcomes should be measured and how to measure them. No consensus or guidance on optimal timing and clinical indicators for surgical interventions exists. In addition, there is no comparative evidence regarding surgical interventions versus non-surgical interventions. There is a need for systematic guidance for care plans for children with augmented communication. Payers will require this research before paying for devices that are multi-purpose and may be used not only for disability purposes. The quality of life workgroup discussed transition, life span approaches to care, long-term effects of earlier treatments. In this area in particular, needs should not be driven by researchers or clinicians alone. This should also include issues related to transition of children into the adults system. What additional information is needed to justify for insurer and/or school systems to pay for services Reports from Small Groups A participant from each small group reported on key discussion points and recommended topics. They noted the lack of evidence, and that much of the research is on single interventions. All areas of research should look at outcomes across the lifespan and include a broad perspective. Academic centers could do the research to determine the optimal patients, timing, and reasons for specific interventions. A care path was recommended for patients and families to assist in predicting the course of disease and to help frame choices about treatment and quality of life. Systematic reviews are currently limited but can help identify gaps in literature that lead to opportunities for knowledge generation. Surveillance and registries can assist and allow for needed subgroup analyses, for tracking relevant data, and for allowing for larger numbers of participants. This group believed it important to prioritize interventions that occur across populations and have a dynamic effect over time. Interventions are delivered as a package of care and should be studied in their complexity. For example, surgery may be offered along with other interventions such as Botox injections. Existing evidence is outdated and does not allow for combinations of interventions and long term impacts. Feeding and nutrition interventions are of great importance and should be given top priority. Outcomes should focus on function and include social inclusion, optimal participation, and functioning especially as related to independent living. Systematic barriers to access and disparities, especially in treatments and devices including communication technologies, should be identified and addressed. Translation, dissemination and implementation of evidence-based information should be available to all impacted populations including patients, families, clinicians, and payers. There is a lack of clear and consistent measurement of quality of life, yet this measure should be included in the equation for all decision-making. There should be a comparative effectiveness review of community supports versus other interventions (Botox, surgery, etc. Social preparation, educational preparation, and psychological preparation all need to be considered in transition phases. Final Prioritization Pam Curtis noted that there were several themes that emerged from the small groups. In addition, the specific activities or studies prioritized by small groups seemed to readily group into four research activities: 1. These include issues of mobility, (wheelchairs, use of standers), feeding/eating/nutrition, communication/speech, care coordination, social supports vs. Methods and Evidence Generation: this category includes the call for networks of centers that could conduct research including clinical practice research, longitudinal studies, sub-group analyses, and multivariate analyses. There was also a call for registries, standardization of outcomes measures, and involvement of consumers and families as partners in research, F-8 3. Development of a Framework and other research activities: this category includes the need for a framework and care pathway, common definitions, consensus on best practices, convening panels on issues such as pain, and meetings of payers to discuss evidence and commonly denied services. Wrap Up and Next Steps Pam Curtis and Shilpa Amin thanked the group for their participation. Botulinum toxin A as an adjunct to Consensus statement on the physical treatment in the management of the upper management of spasticity. Assessment: Botulinum neurotoxin for Neurology and the Practice Committee of the treatment of spasticity (an evidence the Child Neurology Society. Evolution of the neurosurgical effectiveness of therapy for children with management of spasticity.
Purchase generic tricor on line. http://good-cholesterol.blogspot.com.