Michael Maresh MD, FRCOG
- Consultant Obstetrician
- St Mary's Hospital for Women
- Manchester, UK
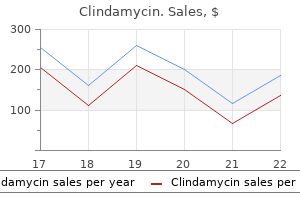
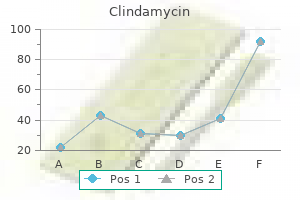
On the other hand infection klebsiella buy cheap clindamycin 150 mg online, most tests aimed at indicating liver damage resulting from prolonged alcohol abuse often suffer from low specificity because many liver diseases have non-alcoholic origin antibiotics prophylaxis buy clindamycin overnight delivery. However treatment for uti medications buy generic clindamycin 300mg line, considering that many patients fail to provide an accurate history of their true alcohol consumption antibiotics hurting stomach generic 150mg clindamycin visa, this creates a validity problem 02 antibiotic generic 300mg clindamycin amex. Hence best antibiotics for mild acne order clindamycin from india, besides the use of sensitive and specific markers of prolonged heavy drinking, there is a definite need to develop and evaluate labora tory methods to monitor recent alcohol consumption in a more objective way. The body water in men makes up about 60% of their body weight and the corresponding figure for women is ~50%, although there are large inter-individual differences in these average figures depending on age and, especially, the amount of adipose tissue. Accordingly, the most specific and direct way to demonstrate that a person has been drinking alcohol is to determine the concentration of ethanol in a sample of blood, breath, urine, or saliva. However, because the presence of alcohol in these body fluids decreases over time owing to metabolism and excretion taking place, the time frame for identifying drinking in this way is rather limited. Breath-alcohol tests should become a standard procedure if a patient is required to refrain from drinking as part of rehabilitation and/or treatment or because of workplace regulations concerning the use of alcohol. Most of the currently available hand-held breath-alcohol analyzers have an analytical sensitivity of about 0. Careful control of calibration and maintenance of these breath-test instru ments is important to ensure obtaining valid and reliable results. However, obtaining a sample of blood is an invasive procedure and the concentration of alcohol, if present, is not available immediately after sampling. The analysis of alcohol in blood is therefore less practical than breath-testing for clinical purposes as a rapid screening test for recent drinking. When absorption and distribution of alcohol in body fluids and tissues are complete, a close correlation exists between the concentrations measured in saliva, blood, and urine. The concentrations of ethanol reaching the saliva glands reflect the arterial blood alcohol concen tration at the time of sampling, which makes saliva more suitable than urine for clinical and other purposes. The acetaldehyde is trapped with semicarbazide to drive the reaction to completion. The length of the resulting blue-colored bar is directly proportional to the concentration of alcohol in the saliva sample and a direct readout of the concentration of alcohol is obtained about 1 min after starting the reaction. Note that each subject emptied the bladder before starting to drink alcohol in the form of neat whisky in the amounts shown. Small quantities of ethanol are excreted through the skin by passive diffusion and also secreted through the sweat glands. Alcohol and other volatiles are extracted with water and the concentration determined provides a cumulative index of alcohol exposure. The biotransformation of ethanol, and of methanol, is shown schematically in Figure 5. The oxidation of ethanol to acetaldehyde takes place in the cytosol compartment of the hepatocyte and the acetaldehyde is swiftly oxidized to acetate in the mitochondria. Raised concentrations of the intermediary products of ethanol oxidation have been pro posed as a way to test for alcohol consumption. However, measuring acetaldehyde is not very practical to confirm recent drinking because of the extremely low concentrations present (<1% of the ethanol concentration), and also the fact that the necessary analytical procedures are much more challenging than those for the analysis of alcohol. An additional problem arises if the blood contains ethanol because acetaldehyde is formed artifactually even after sampling. The blood acetate concentration appears to be independent of the blood-ethanol concentration, and instead increases with the devel opment of metabolic tolerance to alcohol. These alcohols might be ingested with food or drink, such as fresh fruits or fruit juices, or they could be formed by fermentation of dietary sugars through the action of micro-organisms inhabiting the gut. Note that the concentration of methanol in blood remains fairly constant at about 1 mg/dL until the concentration of ethanol reaches a low level. The existence of an effective first-pass metabolism ensures that only vanish ingly small concentrations of ethanol and methanol reach the peripheral circulation. Thereafter, methanol is cleared with a half life of 2 to 3 h, which means that methanol can be detected in body fluids long after the concentration of ethanol has returned to base-line or endogenous levels. Such a test might be useful in forensic investigations when the causes and ac countability for accidents are evaluated. By intravenous infusion of ethanol to reach and maintain a blood-ethanol concentra tion of about 100 mg/dL effectively blocks the metabolism of methanol into its toxic metabolites formaldehyde and formic acid. These other substances, which are produced as byproducts of the fermentation process, are collectively known as congeners and impart the smell and flavor to the alcoholic beverage. Different threshold limits depicting abnormal values need to be applied for women and men separately. The abnormal transferrin pattern appears to be fairly specific for alcohol abuse, and recovers during periods of abstinence with a half life of ~1. However, after prolonged heavy drinking, increased levels of transferrin molecules lacking 2 to 4 of the sialic acid residues (di-, mono-, and a-sialotransferrin, respectively), 86 and apparently also the entire carbohydrate chains, 87 appear. False positive results may be found in non-alcoholic subjects with primary biliary cirrhosis (a condition predominantly seen in women) or chronic active hepatitis, in subjects with the uncommon transferrin D variant, and in a rare defect in glycoprotein metabolism. Because the isoforms lacking 1 to 4 terminal sialic acid residues are progressively less negatively charged, and thereby have higher isoelectric points than tetra-sialotransferrin (pI ~5. Some studies have shown that the relative amount is more accurate, 100-102 but others recommend use of an absolute amount, 81, 82, 103, 104 or no marked differences have been found. However, some of the results are based on experiments using very high, unphysiological concentrations of acetaldehyde, and the relevance of these findings in vivo has been a matter of debate. Moreover, most of the methods used for quantification are probably too complex and unreliable for routine purposes. The concentration of methanol in blood after drinking is also raised owing to the congener present in the alcoholic beverages consumed. Recent studies have shown that this metabolic interaction between methanol and ethanol can help to distinguish between acute and chronic drinking practices. Indeed, this concentration threshold (>1 mg/dL) is assumed to indicate continuous heavy drinking and therefore as a marker of chronic alcoholism. The routine analysis of methanol as well as other biochemi cal markers of alcohol abuse is common practice in Germany to decide on whether treatment or punishment is more appropriate for rehabilitation of convicted drunk drivers. As already indicated, most of the currently available standard laboratory tests lack sufficient sensitivity and/or specificity to warrant their use as the sole evidence of heavy drinking. A useful approach is to combine markers that are independently associated with alcohol consumption. By contrast, in studies on single individuals and when screening people from the general population, most tests are less satisfactory, mainly because of a considerable overlap between values for alcoholics and moderate drinkers, and, furthermore, because many other medical and environmental conditions can cause positive test results. Assuming that the prevalence of excessive drinking is 10%, a marker with 90% sensitivity and specificity will correctly identify 9 of the 10 heavy drinkers in a study population of 100, but, at the same time, incorrectly identify 9 of the 90 healthy subjects as having drinking problems. Thus, the chance of a correct classification under these conditions is only 50% (the positive predictive value). For most of the currently available laboratory markers of alcohol abuse, a single abnormal result is therefore difficult to interpret until confirmed in a repeated test or by complementary testing to exclude other potential causes. Because the various biochemical markers have different life-spans, the time since the last drink should always be considered when evaluating the sensitivity of a test. After discharge from the hospital, blood sampling should be continued for monitoring excessive drinking on a routine basis in connection with each return visit to the clinic. The optimal frequency of testing is dependent in part on the life-span of the marker in question. The use of repeated testing also makes it possible to use individualized instead of popu lation reference limits for each biochemical marker, thereby considerably improving the reliability of results. However, because of inter individual variations, subjects with very low baseline values probably need to drink much larger amounts of alcohol than those with higher baseline values in order to exceed the critical threshold limit. By introducing individualized cutoffs, detection of relapse drinking can be significantly improved. Unequivocal evidence for a genetic component in alcoholism and addiction came from the widely publicized adoption and twin studies. Later research on the inheritance of alcohol dependence lead to the definitions of type 1 and type 2 alcoholism subtypes which have now become widely accepted. This inborn Antabuse-like reaction creates an aversion to alcohol which influences drinking behavior and decreases the risk of becoming dependent on alcohol and developing alcoholic liver disease. Self-reports of drinking practices during interview or in diagnostic questionnaires are widely used for this purpose, but people with alcohol-related problems may deliberately deny or underreport the actual amounts they consume, at least in the early stages of misuse. For this reason, erroneous classification of patients and underdiagnosis of alcohol misuse is common. The perfect biochemical test should be specific for alcohol and also exhibit high sensitivity to hazardous drinking. Furthermore, the test should be inexpensive and performed quickly on a readily available specimen such as urine, saliva, or blood. Measuring ethanol in body fluids or breath is of course the most highly specific test, but because ethanol is eliminated fairly rapidly from the body the sensitivity is low. Most of the currently available laboratory markers perform well when selected populations are being compared, but they are less satisfactory in randomly selected individuals. Although no single marker covering all forms of alcohol use and abuse is likely to be found, combining the most sensitive and specific markers can be very informative. Alcohol is a licit drug, and acceptable levels of consumption vary between countries and societies. Furthermore, a consumption pattern that might be harmless for one individual may be harmful for another, not taking into account the tolerance to alcohol that develops after prolonged misuse (see section 5. Biochemical markers of alcohol use and abuse furnish indirect ways to evaluate harmful effects of alcohol, and to recognize those at risk of becoming alcoholics. However, it should be pointed out that biochemical markers cannot be used to determine the absolute level of consumption, that is, the amounts of alcohol actually ingested. The dopaminergic hypothesis of drug abuse has been proposed by a number of researchers. Dopamine transport occurs with the binding of one molecule of dopamine, one chloride ion, and two sodium ions to the transporter, the transporter then translocates from the outside of the neuronal membrane into the inside of the neuron. This changes the conformation of the chloride ion binding site, thus dopamine transport does not occur. This blockade of dopamine transport potentiates dopaminergic neurotransmission and may be the basis for the rewarding effects of cocaine. While the stimulating and reinforcing effects of cocaine have been recognized for quite some time, it was not until recently that the mechanism(s) for these effects was elucidated. Areas of the brain with the greatest amount of dopaminergic innervation, such as the caudate, putamen, and nucleus accumbens, also demonstrate the greatest amount of binding, whereas moderate amounts of binding can be observed in the substantia nigra and ventral tegmental areas. The question of why these compounds are non addictive while cocaine is quite addictive remains unanswered. The homozygous mice were hyperactive compared to normal mice and, as expected, cocaine did not produce any effect in the locomotor activity of the homozygous mice. The mechanism of action for amphetamine was further defined with the work of Giros et al. This suggests that meperidine may predominantly act at the high affinity transporter site. Neither acute nor chronic morphine administration inhibited binding at the serotonin transporter in the striatum or anterior basal forebrain, suggesting that transporter down-regulation was selective to brain regions important for the reinforcing and/or motivational properties of opiates. Administration of ethanol has been demonstrated to release dopamine in vivo129-131 and in vitro. In addition, a transesterification product of ethanol and cocaine has been discovered, benzoylecgonine ethyl ester or cocaethylene was first described by Hearn et al. Addi tionally, cocaethylene has been demonstrated to produce greater lethality in rats and mice than cocaine. This effect was blocked by the nicotinic antagonists hexamethonium and mecamylamine. Recently it was reported that a series of cocaine analogs that potently inhibited cocaine binding also inhibited [3H]nicotine and [3H]mecamylamine binding. This finding provides an additional potential interaction between the nicotinic and dopaminergic neuronal systems. The short-acting barbiturates, for example, do not interact with the dopamin ergic system, yet they are quite addictive. Some drugs that interact with the dopaminergic system, such as cocaine, are quite addictive, while other drugs, such as mazindol, are not. Clearly factors other than simple interaction with the dopaminergic system are involved, and a simple answer to drug addiction may not be possible. Nonetheless, the dopaminergic system does play a role in the abuse liability for some, if not most, drugs: the stimulants, opiates, marijuana, nicotine, and ethanol, all interact directly or indirectly with the dopaminergic system. In addition, there is a temporal component in that while mazindol interacts with the dopaminergic system, its entry into the brain is slow compared to that of cocaine. Using these powerful new tools that have become available, we may be able to understand the reasons drug abuse occurs and develop strategies to prevent drug abuse. The disposition of [3H]norepinephrine, [3H]dopamine and [3H]dopa in various regions of the brain, J. Effects of 9-tetrahydrocannabinol on potassium-evoked release of dopamine in the rat caudate nucleus: an in vivo electrochemical and in vivo microdialysis study, Brain Res.
Diseases
- Ovarian cancer
- Coenzyme Q cytochrome c reductase deficiency of
- Leukodystrophy reunion type
- Heavy metal poisoning
- Meadows syndrome[disambiguation needed]
- Behr syndrome
- Englemann disease
- Fumaric aciduria
Stress Management at a later date virus making kids sick 300mg clindamycin for sale, particularly if weight loss has been successful antibiotics for sinus infection z pack buy 150mg clindamycin fast delivery. Management of stress is important on a short-term basis because stress hormones increase blood glucose levels antimicrobial activity of xylitol generic 150mg clindamycin with visa. Diet Chronic emotional upsets may lead to missed injections or other compliance problems antibiotics for acne after accutane buy clindamycin with paypal. When this happens antibiotic vaginal infection discount 150mg clindamycin fast delivery, counseling the mainstays of dietary treatment are discussed in detail in for the family and child becomes an important part of Understanding Diabetes (see references) bacteria 1 negative hpf order 150mg clindamycin visa. This allows the family to look of overtreatment of low blood glucose levels (hypoglycemia), for patterns and make changes in insulin dosage. Two than 50% of the values are above the desired range for age or other nutritional factors include adjusting insulin levels for more than 14% below the desired range, the insulin dosage meals and maintaining a consistent schedule of nighttime usually needs to be adjusted. Children with diabetes should be evaluated by a to be eaten and the amount of exercise contemplated. Ideal glucose levels collections or first-morning voids (expressed per milligram of after 2 or more hours of fasting. Normal values differ with the methodology of the laboratory but are generally below 20 mcg/min (or 30 mcg/ Age (y) Glucose Level mg creatinine). This is usually the first test to become aAt least half of the values must be below the upper limit to have a good abnormal in the autoimmune thyroiditis commonly associ HbA1c value. The values should also be below the upper limits for age when ated with type 1 diabetes. In recent years antiendomysial and transglutaminase antibodies, reliable predictors of celiac disease, have been shown to be more common in children with diabetes as well adjust insulin dosages according to changes in growth and as in their siblings. As with insulin pump therapy, additional education, hydroxylase autoantibody, a marker of increased risk of usually at a specialty diabetes center, is required. Laboratory Evaluations only about one third of these antibody-positive individuals. Type 2 diabetes is not an autoimmune disease, and the In addition to home measurements of blood glucose and islet antibody tests are negative. An elevated insulin or C blood or urine ketone levels, the HbA1c level should be peptide level is also helpful, indicating that insulin produc measured every 3 months. Hypoglycemia children to reduce the risk of hypoglycemia because their Hypoglycemia (or insulin reaction) is defined as a blood brains are still developing and they may not relate symptoms glucose level below 60 mg/dL (or 3. Low HbA1c values are generally associated with a greater risk for hypoglycemia (see the following section). The common symptoms of hypoglycemia receive treatment at home by telephone management. Juices are hunger, weakness, shakiness, sweating, drowsiness (at an and other fluids to help wash out the ketones and to prevent unusual time), headache, and behavioral changes. If hypoglycemia is left untreated for several also occur in those with known diabetes who do not check hours, brain damage or death can occur. Repeated episodes ular blood glucose monitoring, controlled snacking, compli of ketoacidosis usually result from missed insulin injections ance of patients and parents, and good education are all and signify that counseling may be indicated, and that a important in preventing severe hypoglycemia. If the blood glucose level is still below 60 mg/dL venous blood pH, blood glucose, and an electrolyte panel. Initial treatment is with physiologic than 10 years) fail to recognize the symptoms of low blood saline (0. For these individuals, by continued signs of dehydration, this is repeated during the glucose control must be liberalized to prevent severe hypoglyce second hour. School personnel, sports coaches, and baby treatment should not exceed 40 mL/kg because of the danger sitters must be trained to recognize and treat hypoglycemia. Families must be educated to check blood or urine ketone Maintenance fluids are as discussed in Chapter 43. If moderate or significant lar insulin is usually given intravenously at a rate of 0. If the glucose level falls below 250 the total daily insulin dosage is given subcutaneously as H or mg/dL (13. The half-life of intravenous insulin is 6 eventually developed renal failure or loss of vision. Thus it is often better to continue intravenous pressure below the 90th percentile for age, and abstinence insulin until subcutaneous insulin can begin acting. In addition to body depletion, serum sodium 3 years or longer (see section on laboratory evaluations, concentrations may be falsely lowered by hyperglycemia, earlier). Similarly, laser treatment to coagulate proliferat quately by the use of physiologic and half-physiologic saline in ing capillaries prevents bleeding and leakage of blood into the rehydration fluids, as discussed earlier. This treatment helps Serum potassium levels may be elevated initially because to prevent retinal detachment and to preserve useful vision of inability of potassium to stay in the cell in the presence of for many people with proliferative diabetic retinopathy. Potas sium should not be given until the serum potassium level is known to be low or normal and the pH is above 7. Associated clinical symptoms are progression of long-term complications in insulin-dependent rare, unpredictable, and may be associated with demise. Cerebral edema may be related to overhydration with hypo Diabetes Prevention Program Research Group: Reduction in the tonic fluids, although the cause is not well understood. It is incidence of type 2 diabetes with lifestyle intervention or now recommended that no more than 40 mL/kg of fluids be metformin. Glaser N et al: Risk factors for cerebral edema in children with given in the first 4 hours of treatment. Report of the Expert Committee on the Diagnosis and Classifica include elevation of the head of the bed, hyperventilation, tion of Diabetes Mellitus. For many years after Garrod first described them metabolite can also be supplemented (eg, glucose adminis in 1908, these conditions were considered rare. This chapter focuses on when to consider meta these disorders can now be treated effectively. Even when bolic disorder in the differential diagnosis of common pedi treatment is not available, correct diagnosis permits parents atric problems. A few of the more important disorders are to make informed decisions about future offspring. The pathology is almost always due either to accumula tion of enzyme substrate behind a metabolic block or to deficiency of the reaction product. The clinical manifestations of inborn errors vary widely Inborn errors must be considered in the differential diagno with both mild and severe forms of virtually every disorder. Pharmacologic doses of a alopecia or abnormal hair, retinal cherry-red spot or retinitis cofactor such as a vitamin can sometimes be effective in pigmentosa, cataracts or corneal opacity, hepatomegaly or restoring enzyme activity. Alternatively, some strategies are splenomegaly, coarse features, skeletal changes (including designed to cope with the consequences of enzyme defi gibbus), neurologic regression, and intermittent or progres ciency. Other features that may be important include restriction of precursor in the diet (eg, low-phenylal in the context of a suspicious history include failure to thrive, anine diet for phenylketonuria), avoidance of catabolism, microcephaly, rash, jaundice, hypotonia, and hypertonia. Acute crises may be brought on by intercurrent infec point to disorders of creatine. Some inborn errors suggest a detected by magnetic resonance imaging can suggest specific diagnosis of nonaccidental trauma (eg, glutaric acidemia groups of disorders (eg, cortical migrational abnormalities in type I) or poisoning (eg, methylmalonic acidemia). Acidosis or common laboratory tests used to diagnose these diseases and altered mental status out of proportion to systemic symp offers suggestions about their use. Laboratory studies are almost always needed for the Laboratory measurements should include electrolytes, am diagnosis of inborn errors. Serum electrolytes and pH should monia, lactate, glucose, blood pH, and urine ketones and be used to estimate anion gap and acid-base status. Serum and urine amino hospitals but care is needed in obtaining samples appropri acid, urine organic acid, and serum acylcarnitine analysis ately. Amino acid and organic acid studies must be per should be performed on samples collected before oral intake formed at specialized facilities to ensure accurate analysis is discontinued and sent later for analysis if indicated by the and interpretation. The physician should know what conditions a test can detect and when it can detect them. A result that substances, and urine ketones should be measured in all is normal in one physiologic state may be abnormal in patients with vomiting and encephalopathy before any treat another. Samples for serum amino acids, hypoglycemic upon prolonged fasting should be positive for serum acylcarnitine profile, and urine organic acid analysis ketones. In such a child, the absence of ketones in the urine should be obtained early and frozen pending the results of suggests a defect in fatty acid oxidation. In the presentation of a Reye-like syndrome Samples used to diagnose metabolic disease may be (ie, vomiting, encephalopathy, and hepatomegaly), amino obtained at autopsy. Samples must be obtained in a timely acids, acylcarnitines, carnitine levels, and organic acids fashion and may be analyzed directly or stored frozen until a should be assessed immediately. Hypoglycemia with inap particular analysis is justified by the results of postmortem propriately low urine or serum ketones suggests the diagno examination, new clinical information, or developments in sis of fatty acid oxidation defects. Studies of other family members may help establish the diagnosis of a deceased patient. Hypoglycemia demonstrate that parents are heterozygous carriers of a Duration of fasting, presence or absence of hepatomegaly, particular disorder or that a sibling has the condition. Mental Retardation nitine profile, carnitine levels, ammonia, and uric acid Some inborn errors can cause mental retardation without should be measured. Measurements of serum efficient in the neonate, and ketonuria in a hypoglycemic or amino acids, urine organic acids, and serum uric acid should acidotic neonate suggests an inborn error. In the older child, be obtained in every patient with nonspecific mental retarda inappropriately low urine ketone levels suggest an inborn tion. Metab should be considered when acidosis occurs with recurrent olites obtained during the acute episode can be very helpful vomiting or hyperammonemia and when acidosis is out of and avoid the need for a formal fasting test. Hyperammonemia gap metabolic acidosis are lactic acidosis, ketoacidosis (including abnormal ketone body production such as in Symptoms of hyperammonemia may appear and progress ketothiolase deficiency), methylmalonic acidemia or other rapidly or insidiously. Decreased appetite, irritability, and organic acidurias, intoxication (ethanol, methanol, ethylene behavioral changes appear first with vomiting, ataxia, lethargy, glycol, and salicylate), and uremia. If renal bicarbonate loss is found, then presence of hyperammonemia, and serum ammonia should a distinction must be made between isolated renal tubular be measured whenever hyperammonemia is possible. Inborn errors associated with renal as carnitine-acylcarnitine translocase deficiency) or, in the tubular acidosis or renal Fanconi syndrome include cystino premature infant, transient hyperammonemia of the new sis, tyrosinemia type I, carnitine palmitoyltransferase I, and born. Serum glucose and ammonia levels quantitative serum amino acids (eg, citrulline), plasma car and urinary pH and ketones should be examined. Samples nitine and acylcarnitine esters, and urine organic acids and for amino acids and organic acids should be obtained at orotic acid. Respiratory alkalosis is usually present in urea once and may be evaluated immediately or frozen for later cycle defects and transient hyperammonemia of the newborn, analysis, depending on how strongly an inborn error is while acidosis is characteristic of hyperammonemia due to suspected. Acidosis are difficult to interpret in the acutely ill patient, but in the Inborn errors may cause chronic or acute acidosis at any absence of shock, high levels of lactic acid suggest primary age, with or without an increased anion gap. Blood lactic acid and pyruvic acid Sample should be collected without a tourniquet, kept on ice, and analyzed immediately. Carnitine and acylcarnitine profile Blood or plasma may be analyzed for total, free, and esterified carnitine; normal values are for the healthy, nonfasted state. Profiling in cultured fibroblasts after fat loading can be helpful in diagnosis of certain conditions. Urine mucopolysaccharides Variations in urine concentration may cause errors in screening tests. Some patients with Morquio disease and many with Sanfilippo disease do not have abnormal mucopolysacchariduria. Enzyme activity in whole blood may become normal after transfusion or vitamin therapy. Other metabolic Patients with severe acidosis, hypoglycemia, and hyperam disorders for which newborns are frequently screened monemia may be very ill; initially mild symptoms may include maple syrup urine disease, homocystinuria due to worsen quickly, and coma and death may ensue within cystathionine synthase deficiency, and biotinidase defi hours. Expanded newborn screening using tandem mass patients can recover completely, even from deep coma. All spectrometry detects several disorders of amino acid, organic oral intake should be stopped.
Generic clindamycin 150 mg fast delivery. What is ANTIMICROBIAL? What does ANTIMICROBIAL mean? ANTIMICROBIAL meaning definition & explanation.
Replacement of such losses should be similar in type and amount to the fluid being lost treatment for dogs eating cane toads purchase clindamycin no prescription. Correction of pre existing defi cits and correction of ongoing losses shall be discussed antibiotic resistance video youtube cheap clindamycin 300mg overnight delivery, wherever relevant (see section on Diarrhoea) going back on antibiotics for acne buy clindamycin 150 mg visa. Maintenance requirements in children A guideline for estimating daily fluid and electrolytes requirement in a normal child under normal conditions is: Water-100 ml/100 Kcal/day; sodium-1-3 mEq/100 Kcal/day; potassium-1-2 mEq/100 Kcal/day antibiotic resistance how to prevent buy clindamycin 300mg with visa. Hence antibiotic resistant bacteria evolution buy cheap clindamycin 150 mg on-line, the fluid requirement based on caloric requirement for different weight groups can be calculated as follows: Weight Fluid requirements 3-10 kg 100 ml/kg/day 10-20 kg 1000 + 50 ml/kg/day for each kg >10 zeomic antimicrobial purchase line clindamycin. Refer to the section on newborn care for guidelines on fluid therapy in neonates and those weighing <3. The most commonly employed intravenous maintenance fl uid employed in children is N/5 (0. Normal fluid requirements of newborns Age Total fluids Glucose/Dextrose Electrolyte (days) (ml/kg/day) I 60 10% Dextrose in water None 2 70-80 do None 3 80-90 do Sodium2-3mmol/kg/day Potassium2mmol/kg/day 4 90-100 do do 5 100-110 do do 6 110-120 do do From day 3 onwards, fluid containing glucose-electrolyte mixture can be provided using commercially available paediatric maintenance intravenous solutions provided 5% weight loss has been documented. However, in babies <1500 g, the fluid requirement after day 7 need to be increased by 10-20 ml/kg/day till a maximum of 150 ml/kg/day. Conditions that increase fluid requirement o o Fever: For every 1 C increase over 37. Conditions that decrease fluid requirement Congestive cardiac failure: Fluid requirements are reduced to two-thirds of the normal need for that age. Potassium should be added with caution or omitted in suspected cases of acute renal failure. Clinical features Drowsiness, seizures and coma Hypotension, and circulatory failure. Correction of asymptomatic hyponatraemia should be gradual (increase the Na+ by 0. Acute symptomatic hyponatraemia is treated with administration of 3% sodium chloride 1 2 ml/kg/h till symptoms resolve. The deficit is calculated as follows: Sodium defi cit = [desired Na+ present Na+] weight 0. Clinical features Altered sensorium weakness, irritability, Focal neurologic deficits, and even coma or convulsions. Replace water deficit as assessed by degree of dehydration over a period of 48 hours with a solution containing 40 mEq/L of sodium. Monitor serum sodium closely to ensure a gradual fall (and prevent rapid fall) in serum sodium. Clinical features Paraesthesias, weakness, Ascending paralysis, Respiratory failure Tetany. Moderate hyperkalaemia (serum K+ 6 to 7 mEq/L or peaked T waves) is managed by administering a glucose insulin infusion (0. Dialysis has to be done in case the hyperkalaemia is refractory to therapy as in renal failure. It may be due to: (a) Deficiency of iron, folic acid, vitamin B12, copper, protein, etc. Anaemia due to excessive blood loss massive oesophageal variceal bleeding, rectal polyps, etc. The following section describes the differential diagnosis of cases of anaemia according to preliminary investigations results: 1. Elevated foetal haemoglobin (HbF) on blood electrophoresis confi rms the diagnosis. Lead poisoning and pyridoxine responsive anaemia, sideroblastic anaemia and copper defi ciency are rare. Megaloblastic anaemia of B12 and folate defi ciency is common and may have associated neutropenia and/or thrombocytopenia. Other causes of macrocytic anaemia are liver diseases, hypothyroidism, thiamine defi ciency and some inborn errors of metabolism. Bone marrow infi ltration such as leukaemia and other neoplasms, storage disorders, myelofi brosis, etc. Treatment Iron deficiency anaemia is very common between the age of 9 month and 1 year because of transition of diet and is also known as physiological anaemia of infancy. Regular supplementation of iron in dose of 1 mg/kg/day is recommended in children after 6 month of age and in premature babies, after 4 months of age. If any child does not respond to oral therapy, then he should be investigated for other cause of anaemia such as Nonpharmacological After the period of exclusive breastfeeding (6 months), cereal based diet should be added. Give packed cell transfusion, usually 2-3 ml/kg at one time under close monitoring to severely anaemic children (Hb <4-5 g/dl). Frusemide (1 mg/kg/dose) may be administered, if there is evidence of cardiovascular overload. Ferrous Sulphate/Ferrous gluconate/Ferrous fumarate 2-3 mg/kg/day of elemental iron in 2-3 divided doses to be given between meals for 8-12 weeks after normal Hb concentration for age is achieved. Older children who can take tablets Iron Folic acid tablets and Tab Vitamin B12 Usual Iron preparations have 35-50 mg elemental iron per 5 ml of syrup or per ml of drops. Parenteral iron therapy may also be used in severely anaemic child not likely to take oral therapy because of socioeconomic reasons. When parentral iron is required, the total dose may be calculated: Dose of iron required (mg) = wt (kg) 2. Such extreme forms are rare; most cases suffer from mild and moderate nutritional defi cit. Other micronutrient defi ciencies including magnesium, copper, zinc, vitamins B, C, D and K. These children are at high risk of death and they require urgent attention and management in the hospital. Mild and moderately under-nourished children are best treated in their own home surroundings. Domiciliary treatment of malnourished children by their mother is economical, offers in-built advantage of practical health education, and is associated with minimal recurrence risk. The parents should be advised to increase the food intake of the child by all available means. The child should receive adequate amount of calories and protein in the diet, which should be prepared from the locally available, inexpensive foods. The child should be kept under surveillance by using a growth chart and effort should be made that he does not slip down to severe malnutrition. Prepare for follow-up after recovery these steps are accomplished in two phases: an initial stabilisation phase where the acute medical conditions are managed; and a longer rehabilitation phase. Severe malnutrition Severely wasted children and those with oedema need hospitalization. Other indications for admission in an undernourished child are severe dehydration, severe diarrhoea, hypothermia, shock, systemic infection, severe anaemia, jaundice, bleeding, age less than one year, or persistent loss of appetite. If electric gadgets are not available, cover the child Hypothermia (rectal temperature well. Give 2-hourly Hypoglycaemia (blood sugar <54 mg/dl) feeds, day and night, at least for the first day. Starter classification) formula is given in alternate hours during this period until the child is rehydrated. Check respiratory rate, pulse rate, urine output and frequency of stools and vomiting. If there is no improvement or worsening after the fi rst hour of the fluid bolus, consider septic shock and treat accordingly (. Potassium can be given as syrup potassium chloride; the most common preparation available has 20 mEq/15 ml. If oral commercial preparation is not available give injection magnesium sulphate (50% which has 2 mEq/ml) orally as magnesium supplements mixed with feeds for 2 weeks. Give 10 ml/kg slowly over 4-6 hours and Severe anaemia (haemoglobin<4 g/dl) give Inj. Give same dose, on Day 0, 1 and 14 if there is clinical evidence of vitamin A deficiency. Signs of improvement During these seven days, a child with kwashiorkor will lose weight and a marasmic child gains little or nothing because the tissue gains are masked by excess body water loss. Starting point: Child has started showing signs of recovery of appetite and change of expressions. Clinical features Skeletal deformities like genu valgum/genu varum, (416) Broadening of wrists, Susceptibility to fractures, Weakness, hypotonia and disturbances in growth. Most often it is nutritional (lack of exposure to sunlight and inadequate dietary intake) and occurs between 2 months to 2 years of age. Radiological picture shows that epiphyseal growth plate is increased in thickness, cupped with hazy metaphyseal borders. Serum calcium is generally normal or low, phosphate is low or normal and alkaline phosphatase is raised in nutritional rickets. Treatment Nonpharmacological Encourage the child to play outdoors/increase exposure to sunlight. If no response to therapy after 4 weeks refer to a higher centre for evaluation of non-nutritional rickets. Calcium supplementation (elemental calcium) 1-3 years 700 mg/day; 4-8 years 1000 mg/day; 9-18 years 1300 mg/day Reference 1. Clinical features Involuntary discharge of urine after the age at which bladder control should have been established (5 years). Pharmacological Indicated only in children > 6 years where sufficient trial of nonpharmacological management has failed with following: Tab. Imipramine: 6-8 year (25 mg), 9-12 year (50 mg), >12 year (75 mg) once a day at bedtime. Refer the patient to a higher centre, if organic cause is suspected or when diagnosis is in doubt. Clinical features Cold for 2-4 days followed by cough, wheeze and rapid respiration. Investigations Normal or minimal increase in total leucocyte counts with relative lymphocytosis. Treatment Nonpharmacological For associated nasal block, normal saline drops in both nostrils as and when required, especially before feeds, and use of home remedies (ginger, honey, tulsi) for control of cough and plenty of liquids orally. Pharmacological Treatment of mild disease (ambulatory treatment at home) No antibiotics. Paracetamol 10-15 mg/kg 4-6 hourly for fever (for details see section on Fever in Chapter 1). Hospitalize immediately, if any of the following develop: Chest indrawing, Poor feeding, Cyanosis, Altered sensorium Convulsions If there is no improvement or deterioration at any time during the illness, the patient should be managed as severe disease. Oxygen administration by oxygen hood or nasal catheter and intravenous fl uids, if child is not able to feed. Monitor improvement in respiratory rate, lower chest indrawing, diffi culty in feeding, excessive crying, cyanosis and oxygen saturation, if available, every 4-6 hours till there is signifi cant improvement. Prednisolone Treatment of Respiratory Syncytial Virus Infection: A Randomized Controlled Trial of 147 infants. Randomized Placebo-Controlled Trial of Nebulized Corticosteroids in Acute Respiratory Syncytial Virus Bronchiolitis. Influenza Clinical Features Fever, Cough with rapid breathing, (419) Lower chest indrawing, Crepitations/wheezing, Difficulty in feeding Cyanosis. On the basis of clinical features, pneumonia can be classified as mild to very severe disease. Treatment Nonpharmacological Nasal block to be treated with saline nasal drops as and when required, especially before feeds. Pneumonia Patients with age more than 2 months and with absence of features of severe/very severe pneumonia can be treated at home. Severe pneumonia and very severe pneumonia or age <2 months treated as inpatients 1. Continue with oxygen until the signs of hypoxia (such as severe lower chest wall in-drawing or breathing rate of 70/ min) are no longer present.
Jetwatika (Tinospora Cordifolia). Clindamycin.
- What is Tinospora Cordifolia?
- Are there any interactions with medications?
- Diabetes, high cholesterol, upset stomach, gout, cancer including lymphoma, rheumatoid arthritis, liver disease, stomach ulcer, fever, gonorrhea, syphilis, and to counteract a suppressed immune system.
- Allergies (Hayfever).
- What other names is Tinospora Cordifolia known by?
- Are there safety concerns?
- How does Tinospora Cordifolia work?
- Dosing considerations for Tinospora Cordifolia.
Source: http://www.rxlist.com/script/main/art.asp?articlekey=97101