Julie Carrier, PhD
- Centre d?tude du Sommeil et des Rythmes
- Biologiques, H?pital du Sacr?-Coeur de Montr?al,
- Montr?al, QC, Canada
If the laboratory has windows that open to the exterior arrhythmia questions and answers buy cheap avalide 162.5 mg line, they are fitted with fly screens pulse pressure in athletes avalide 162.5mg online. The following standard and special practices blood pressure pediatric buy discount avalide 162.5 mg on-line, safety equipm ent hypertension patho purchase avalide with visa, and facilities apply to agents assigned to Biosafety Level 2: A arrhythmia for dummies purchase avalide on line amex. Persons wash their hands after they handle viable materials heart attack reasons cheap avalide on line, after removing gloves, and before leaving the laboratory. Eating, drinking, smoking, handling contact lenses, and applying cosmetics are not permitted in the work areas. Food is stored outside the work area in cabinets or refrigerators designated for this purpose only. All procedures are performed carefully to minimize the creation of splashes or aerosols. All cultures, stocks, and other regulated wastes are decontaminated before disposal by an approved decontamination method such as autoclaving. Materials to be decontaminated off-site from the facility are packaged in accordance with applicable local, state, and federal regulations, before rem oval from the facility. Access to the laboratory is limited or restricted by the laboratory director when work with infectious agents is in progress. In general, persons who are at increased risk of acquiring infection, or for whom infection may have serious consequences, are not allowed in the laboratory or animal rooms. For example, persons who are immunocompromised or immunosuppressed may be at increased risk of acquiring infections. The laboratory director has the final responsibility for assessing each circumstance and determining who m ay enter or work in the laboratory or animal room. The laboratory director establishes policies and procedures whereby only persons who have been advised of the potential hazards and meet specific entry requirements. A biohazard sign must be posted on the entrance to the laboratory when etiologic agents are in use. Laboratory personnel receive appropriate immunizations or tests for the agents handled or potentially present in the laboratory. When appropriate, considering the agent(s) handled, baseline serum samples for laboratory and other at-risk personnel are collected and stored. Additional serum specimens may be collected periodically, depending on the agents handled or the function of the facility. Biosafety procedures are incorporated into standard operating procedures or in a biosafety manual adopted or prepared specifically for the laboratory by the laboratory director. Personnel are advised of special hazards and are required to read and follow instructions on practices and procedures. The laboratory director ensures that laboratory and support personnel receive appropriate training on the potential hazards associated with the work involved, the necessary precautions to prevent exposures, and the exposure evaluation procedures. Personnel receive annual updates or additional training as necessary for procedural or policy changes. Needles and syringes or other sharp instrum ents should be restricted in the laboratory for use only when there is no alternative, such as parenteral injection, phlebotomy, or aspiration of fluids from laboratory animals and diaphragm bottles. Syringes which re-sheathe the needle, needleless systems, and other safety devices are used when appropriate. Containers of contaminated needles, sharp equipment, and broken glass are decontaminated before disposal, according to any local, state, or federal regulations. Cultures, tissues, specim ens of body fluids, or potentially infectious wastes are placed in a container with a cover that prevents leakage during collection, handling, processing, storage, transport, or shipping. Laboratory equipment and work surfaces should be decontaminated with an effective disinfectant on a routine basis, after work with infectious materials is finished, and especially after overt spills, splashes, or other contamination by infectious materials. Contaminated equipment must be decontaminated according to any local, state, or federal regulations before it is sent for repair or maintenance or packaged for transport in accordance with applicable local, state, or federal regulations, before removal from the facility. Spills and accidents that result in overt exposures to infectious materials are immediately reported to the laboratory director. Medical evaluation, surveillance, and treatment are provided as appropriate and written records are maintained. These may include centrifuging, grinding, blending, vigorous shaking or mixing, sonic disruption, opening containers of infectious materials whose internal pressures may be different from ambient pressures, inoculating animals intranasally, and harvesting infected tissues from animals or embryonate eggs. Such materials may be centrifuged in the open laboratory if sealed rotor heads or centrifuge safety cups are used, and if these rotors or safety cups are opened only in a biological safety cabinet. Protective laboratory coats, gowns, smocks, or uniforms designated for lab use are worn while in the laboratory. All protective clothing is either disposed of in the laboratory or laundered by the institution; it should never be taken hom e by personnel. Gloves are worn when hands may contact potentially infectious materials, contaminated surfaces or equipment. Gloves are disposed of when overtly contaminated, and removed when work with infectious materials is completed or when the integrity of the glove is compromised. Bench tops are impervious to water and are resistant to moderate heat and the organic solvents, acids, alkalis, and chemicals used to decontaminate the work surfaces and equipment. Install biological safety cabinets in such a manner that fluctuations of the room supply and exhaust air do not cause the biological safety cabinets to operate outside their parameters for containment. However, planning of new facilities should consider mechanical ventilation system s that provide an inward flow of air without recirculation to spaces outside of the laboratory. Laboratory personnel have specific training in handling pathogenic and potentially lethal agents, and are supervised by competent scientists who are experienced in working with these agents. It is recognized, however, that some existing facilities may not have all the facility features recommended for Biosafety Level 3. In this circumstance, an acceptable level of safety for the conduct of routine procedures. The decision to implement this modification of Biosafety Level 3 recommendations should be made only by the laboratory director. The following standard and special safety practices, equipm ent and facilities apply to agents assigned to Biosafety Level 3: A. Access to the laboratory is limited or restricted at the discretion of the laboratory director when experiments are in progress. Persons wash their hands after handling infectious materials, after removing gloves, and when they leave the laboratory. Eating, drinking, smoking, handling contact lenses, and applying cosmetics are not permitted in the laboratory. Persons who wear contact lenses in laboratories should also wear goggles or a face shield. Food is stored outside the work area in cabinets or refrigerators designated for this purpose only. Work surfaces are decontaminated at least once a day and after any spill of viable material. All cultures, stocks, and other regulated wastes are decontaminated before disposal by an approved decontamination method, such as autoclaving. Materials to be decontaminated outside of the immediate laboratory are placed in a durable, leakproof container and closed for transport from the laboratory. The laboratory director controls access to the laboratory and restricts access to persons whose presence is required for program or support purposes. Persons who are at increased risk of acquiring infection or for whom infection may have serious consequences are not allowed in the laboratory or animal rooms. For example, persons who are immunocompromised or immunosuppressed may be at risk of acquiring infections. The director has the final responsibility for assessing each circum stance and determining who m ay enter or work in the laboratory. The laboratory director establishes policies and procedures whereby only persons who have been advised of the potential biohazard, who meet any specific entry requirem ents. When infectious materials or infected animals are present in the laboratory or containment module, a hazard warning sign, incorporating the universal biohazard sym bol, is posted on all laboratory and animal room access doors. The hazard warning sign identifies the agent, lists the name and telephone number of the laboratory director or other responsible person(s), and indicates any special requirements for entering the laboratory, such as the need for immunizations, respirators, or other personal protective measures. Laboratory personnel receive the appropriate immunizations or tests for the agents handled or potentially present in the laboratory. Baseline serum samples are collected as appropriate and stored for all laboratory and other at-risk personnel. Additional serum specimens m ay be periodically collected, depending on the agents handled or the function of the laboratory. A biosafety manual specific to the laboratory is prepared or adopted by the laboratory director and biosafety precautions are incorporated into standard operating procedures. Personnel receive annual updates or additional training as necessary for procedural changes. The laboratory director is responsible for ensuring that, before working with organisms at Biosafety Level 3, all personnel dem onstrate proficiency in standard microbiological practices and techniques, and in the practices and operations specific to the laboratory facility. This might include prior experience in handling human pathogens or cell cultures, or a specific training program provided by the laboratory director or other competent scientist proficient in safe microbiological practices and techniques. Syringes which re-sheathe the needle, needleless systems, and other safe devices are used when appropriate. Broken glassware must not be handled directly by hand, but must be removed by mechanical means such as a brush and dustpan, tongs, or forceps. Containers of contaminated needles, sharp equipment, and broken glass should be decontaminated before disposal, and disposed of according to any local, state, or federal regulations. All open manipulations involving infectious materials are conducted in biological safety cabinets or other physical containment devices within the containment module. Clean-up is facilitated by using plastic-backed paper toweling on non-perforated work surfaces within biological safety cabinets. Laboratory equipment and work surfaces should be decontaminated routinely with an effective disinfectant, after work with infectious materials is finished, and especially after overt spills, splashes, or other contam ination with infectious materials. Spills of infectious materials are decontaminated, contained and cleaned up by appropriate professional staff, or others properly trained and equipped to work with concentrated infectious m aterial. Contaminated equipment must be decontaminated before removal from the facility for repair or maintenance or packaging for transport, in accordance with applicable local, state, or federal regulations. Spills and accidents that result in overt or potential exposures to infectious materials are immediately reported to the laboratory director. Appropriate medical evaluation, surveillance, and treatment are provided and written records are maintained. Animals and plants not related to the work being conducted are not permitted in the laboratory. Protective laboratory clothing such as solid-front or wraparound gowns, scrub suits, or coveralls are worn by workers when in the laboratory. Gloves must be worn when handling infectious materials, infected animals, and when handling contaminated equipm ent. All manipulations of infectious materials, necropsy of infected animals, harvesting of tissues or fluids from infected animals or embryonate eggs, etc. Respiratory and face protection are used when in rooms containing infected animals. The laboratory is separated from areas that are open to unrestricted traffic flow within the building, and access to the laboratory is restricted. Passage through a series of two self-closing doors is the basic requirement for entry into the laboratory from access corridors. The sink is hands-free or automatically operated and is located near the room exit door. Walls, ceilings, and floors should be smooth, impermeable to liquids and resistant to the chemicals and disinfectants normally used in the laboratory. Openings such as around ducts and the spaces between doors and fram es are capable of being sealed to facilitate decontamination. Bench tops are impervious to water and are resistant to moderate heat and the organic solvents, acids, alkalis, and those chemicals used to decontaminate the work surfaces and equipment. Chairs and other furniture used in laboratory work should be covered with a non-fabric material that can be easily decontaminated. A method for decontam inating all laboratory wastes is available in the facility and utilized, preferably within the laboratory. If waste is transported out of the laboratory, it should be properly sealed and not transported in public corridors. Biological safety cabinets are required and are located away from doors, from room supply louvers, and from heavily-traveled laboratory areas.
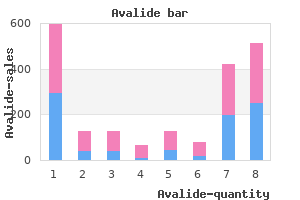
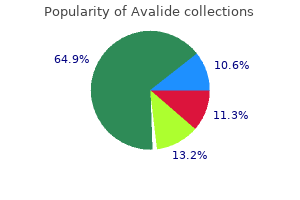
Laboratory supin the practice of reproductive medicine blood pressure values order generic avalide line, it is not intended port for the diagnosis and monitoring of thyroid disease arteria carotida externa purchase avalide line. The incidence of thyroid disorders in the community: a twenty-year mittee and the Board of Directors of the American follow-up of the Whickham Survey venice arrhythmia 2013 generic avalide 162.5 mg otc. The referfinancial relationships with manufacturers or distributors ence range and within-person variability of thyroid stimulating hormone of goods or services used to treat patients arrhythmia prognosis order avalide 162.5 mg overnight delivery. Treatment of thyroid disorders before conception and the discussion or development of this document arteria principal cheap 162.5mg avalide overnight delivery. Effectsofmaternal subclinical hypothyroidism on obstetrical outcomes during early pregnancy hypertension over 60 avalide 162.5 mg lowest price. Effect of levothyrin the first twenty weeks of pregnancy and subsequent fetal and infant oxine treatment on in vitro fertilization and pregnancy outcome in infertile development: a prospective population-based cohort study in China. Improved in vitro fertilization at 11 to 13 weeks of gestation and subsequent fetal death. Thyroid function in women found to have early pregnancy thyroxine substitution are often dysregulated in early pregnancy. Increased prevalence clinical elevations of thyroid-stimulating hormone and assisted reproductive of antithyroid antibodies identified in women with recurrent pregnancy loss technology outcomes. Assisted reproduction and thyroid autoimmunity: an unfortunate comSchiettecatte J, et al. Thyroid autoimmunity in patients with recurrent spontaneous clinical hypothyroidism. Sieiro Netto L, Medina Coeli C, Micmacher E, Mamede Da Costa S, Nazar L, outcome in hypothyroid pregnancies. Abnormalities of maternal thyLevothyroxinetreatmentinthyroidperoxidaseantibody-positive womenunroid function during pregnancy affect neuropsychological development of dergoing assisted reproduction technologies: a prospective study. The cost-effectiveness of universal thyroid dysfunction at delivery of infants born %34 weeks and neurodevescreening in pregnancy for subclinical hypothyroidism. CostSubclinical hypothyroidism in pregnancy: intellectual development of effectiveness of universal and risk-based screening for autoimmune thyroid offspring. Reduction of miscarriages hypothyroid mothers restored to normal thyroxine (T(4)) concentration by through universal screening andtreatment ofthyroid autoimmune diseases. Management of thyroid dysfunction during pregnancy and postfunction in early pregnancy in Japanese healthy women: relation to urinary partum: an Endocrine Society clinical practice guideline. Thyroid disorders are commonly separated into two major categories, hyperthyroidism and hypothyroidism, depending on whether serum thyroid hormone levels (T4 and T3) are increased or decreased, respectively. Thyroid disease generally may be sub-classified based on etiologic factors, physiologic abnormalities, etc. More than 13 million Americans are affected by thyroid disease, and more than half of these remain undiagnosed. Patients often present with vague, general clinical manifestations; in particular, the elderly may not associate the signs and symptoms with a disease process and thus may not bring them to the attention of their primary care provider. The prevalence and incidence of thyroid disorders is influenced primarily by sex and age. Thyroid disorders are more common in women than men, and in older adults compared with younger age groups. The prevalence of unsuspected overt hyperthyroidism and hypothyroidism are both estimated to be 0. For men more than 60 years of age, the prevalence rate of hyperthyroidism is estimated to be 0. Overt thyroid dysfunction is uncommon in women less than 40 years old and in men <60 years of age. Complications that can arise from untreated thyroid disease include elevated cholesterol levels and subsequent heart disease, infertility, muscle weakness, and osteoporosis. The issue of routine screening is controversial because cost-effectiveness has not been clearly proven. Although it may not be economically feasible or necessary to test all patients for thyroid dysfunction, there are instances when thyroid screening is appropriate. Testing and screening may also be important for patients taking certain medications, herbal drugs and food supplements as described in the final section of this chapter. Treatment of congenital hypothyroidism requires full doses of thyroid hormone as soon after birth as possible to prevent neurologic damage and impaired development. If treatment is delayed beyond 6 months after birth, full neurologic development is impaired and regression of neurologic deficits is not possible. Also, hypothyroidism may occur in the neonate if the mother ingests goitrogens (eg, cabbage or turnips) that inhibit normal feedback mechanisms for regulating thyroid hormone levels, or if the mother becomes hypothyroid through over-treatment with thionamides. The extent to which thioamide therapy is responsible for hypothyroidism in the fetus or neonate is controversial. Some studies have suggested that undiagnosed hypothyroidism impairs fertility, and in the pregnant patient, it results in a four times greater risk for miscarriage during the second trimester. Another opportunity or pharmacists to counsel on thyroid screening is when a woman is seeking advice on ovulation predictor kits and pregnancy tests. If patients on hormone replacement therapies continue to experience mood swings, depression, or sleep disturbances, it would be appropriate to advise these women to request a thyroid function test. They often seek advice about over-the-counter vitamins or herbs (eg, ginkgo biloba) that can help alleviate these symptoms. Tests are available to directly or indirectly measure both bound and unbound hormone. A tracer dose of radioactive iodine (I or 123 I) is administered intravenously, and the thyroid gland is scanned for iodine uptake. A normal test result is 5% to 15% of the dose taken up within 5 hours and 15% to 35% within 24 hours. In patients who are iodine deficient, results indicate a greater uptake of iodine, and in those with an iodine excess, lesser uptake. Additionally, after the administration of radioactive iodine, a thyroid scan can reveal "hot" or "cold" spots indicating areas of increased or decreased iodine uptake, which can be useful in the detection of thyroid carcinoma. Causes, Symptoms and Thyroid Function Tests Hyperthyroidism represents a myriad of thyroid disorders (Table 1) characterized by elevated levels of circulating thyroid hormones. The annual incidence of hyperthyroidism is three per 1,000 in the general population, and the condition is eight times more common in women. It is important to distinguish between these since the prognosis and treatment will be different. The different forms of hyperthyroidism are discussed in more detail in the sections that follow. The major symptoms, physical findings and laboratory values associated with hyperthyroidism are outlined in Table 3 below. It is important to note that hyperthyroid patients may not exhibit all of these symptoms, and may display variable thyroid function test results depending on the form of the disease. Generally, however, hyperthyroidism results in acceleration of many physiologic functions are accelerated. The heart pounds, beats more quickly, and may develop an abnormal rhythm, leading to an awareness of the heartbeat (palpitations). Their skin may become moist as they tend to sweat profusely, and they may develop "myedema". Hyperthyroid patients may develop a fine tremor in their hands, and generally have good deep tendon reflexes. Many people feel nervous, tired, and weak, yet have an increased level of activity. Hyperthyroid patients may have an increased appetite, yet they lose weight due to the increased metabolic actions of thyroid hormone. Most hyperthyroid patients have frequent bowel movements, occasionally with diarrhea, and sleep poorly. They simply become weak, sleepy, confused, withdrawn, and depressed, symptoms often associated with aging. However, heart problems, especially abnormal heart rhythms, are seen more often in older people with hyperthyroidism. Hyperthyroidism is often associated with a goiter or thyroid nodules as discussed more in the sections that follow. Imagining results may be misleading since some small tumors may not be detected, and some patients may have pituitary tumors without hyperthyroidism. Pituitary adenomas may also secrete prolactin and growth hormone and therefore also cause amenorrhea/galactorrhea or signs of acromegaly. The pituitary tumors may also effect the optic nerve and cause visual field defects. This condition is treated with transphenoid pituitary surgery followed by irradiation of the pituitary gland. This is a rare familial syndrome and is observed more commonly in women than men (2:1). Autoantibodies that react with the orbital muscle of the eye and fibroblasts of skin are also produced and initiate the so-called "extrathyroidal" manifestations of Graves disease (see below). Dermopathy appears to be related to the infiltration and deposition of disease-related antibodies in the skin, usually over the shins. The thickened area may be itchy and red and feels hard when pressed with a finger. As with the ocular symptoms described below, these symptoms may begin before or after other symptoms of hyperthyroidism are noticed. Infiltrative changes involving the orbital contents and enlargement of the ocular muscles. These abnormalities typically do not affect ocular function and resolve upon treatment for hyperthyroidism. Infiltrative ophthalmopathy involves lymphocytic infiltration, increased mucopolysaccharide content, fat and water in all retrobulbar tissue. The cause of these manifestations is unknown, but it is suggested that antibodies may react with orbital muscle to cause or mediate development of exophthalmos (and fibroblast tissue to mediate skin changes). In some patient populations unique complications of hyperthyroidism may be expressed. For example, Asians and Hispanics may present with recurrent muscle flaccidity ranging from mild muscle weakness to total paralysis, and markedly diminished deep tendon reflexes a syndrome referred to as hypokalemic periodic paralysis. These symptoms are likely to occur after strenuous exercise or high carbohydrate diets and are related to hypokalemia resulting from a shift of potassium from extracellular to intracellular sites. Treatment of these patients involves correcting hyperthyroidism, administration of potassium, administration of spironolactone to conserve potassium and propranolol to minimize intracellular shifts. Untreated, patients with elevated thyroid hormone levels are at risk for reduced quality of life, atrial fibrillation, and osteoporosis. The objectives of treatment of thyrotoxicosis are to reduce the excess production and availability of thyroid hormones and to reduce or control symptoms of thyrotoxicosis. Therapy is individualized on the basis of patient age, sex, other concurrent medical conditions, and response to previous therapy as discussed in a separate Tutorial. Hyperthyroidism from Thyroid Autonomy: Toxic Adenoma and Diffuse Toxic Goiter/Toxic Multinodular Goiter An autonomous thyroid nodule is a discrete thyroid mass whose function is independent or normal pituitary control. Typically, the older the patient the larger the toxic nodules and the greater thyroid hormone release and degree of thyrotoxicosis. While T4 levels typically are elevated in these patients, sometimes only T3 levels are increased. Therefore if T4 levels are normal in such patients, T3 levels should be determined to rule out T3 toxicosis. The thionamide antithyroid drugs typically are not effective because they do not halt the proliferative process in the nodule. The thyroid gland normally enlarges in response to an increased demand for thyroid hormones that occurs in puberty, pregnancy, iodine deficiency and immunologic, viral or genetic disorders.
Cheap 162.5 mg avalide fast delivery. High Blood Pressure.
Impact of hepatitis B and C infection on health services utilization in homeless adults: a test of the Gelberg-Andersen behavioral model for vulnerable populations hypertension journal article purchase cheap avalide on line. Correlates of hepatitis C virus infection in homeless men: a latent variable approach blood pressure chart jpg cheap avalide 162.5mg fast delivery. Psychosis in a methadone-substituted patient during interferon-alpha treatment of hepatitis C pulse pressure greater than 50 purchase avalide canada. Living with hepatitis C virus: a systematic review and narrative synthesis of qualitative literature pulse pressure high trusted avalide 162.5mg. Global epidemiology of hepatitis B and hepatitis C in people who inject drugs: results of systematic reviews pulse pressure 42 buy generic avalide on line. Meta-regression of hepatitis C virus infection in relation to time since onset of illicit drug injection: the infuence of time and place 1 5 order cheap avalide on-line. Geographic differences in temporal incidence trends of hepatitis C virus infection among people who inject drugs: the InC3 collaboration. Injection drug use and hepatitis C virus infection in young adult injectors: using evidence to inform comprehensive prevention. Hepatitis C virus infection epidemiology among people who inject drugs in Europe: a systematic review of data for scaling up treatment and prevention. Committee on a National Strategy for the Elimination of Hepatitis B and C; Board on Population Health and Public Health Practice; Health and Medicine Division; National Academies of Sciences, Engineering, and Medicine. Eliminating the public health problem of hepatitis B and C in the United States: phase one report. Increases in hepatitis C virus infection related to injection drug use among persons aged fi 30 years Kentucky, Tennessee, Virginia, and West Virginia, 2006-2012. Increases in acute hepatitis B virus infections Kentucky, Tennessee, and West Virginia, 2006-2013. Estimating the cascade of hepatitis C testing, care and treatment among people who inject drugs in Australia. Hepatitis C testing in general practice settings: a cross-sectional study of people who inject drugs in Australia. Hepatitis C virus transmission among human immunodefciency virus-infected men who have sex with men: modeling the effect of behavioral and treatment interventions. Elbasvir-grazoprevir to treat hepatitis C virus infection in persons receiving opioid agonist therapy: a randomized trial. Expert perspectives on Western European prison health services: do ageing prisoners receive equivalent carefi Incidence of primary hepatitis C infection and risk factors for transmission in an Australian prisoner cohort. Incidence and risk for acute hepatitis C infection during imprisonment in Australia. Evaluation of a prison outreach clinic for the diagnosis and prevention of hepatitis C: implications for the national strategy. A descriptive model of patient readiness, motivators, and hepatitis C treatment uptake among Australian prisoners. Diversity of release patterns for jail detainees: implications for public health interventions. A systematic review of provider knowledge of hepatitis C: is it enough for a complex diseasefi Predictors of treatment in patients with chronic hepatitis C infection role of patient versus nonpatient factors. The impact of injecting drug use status on hepatitis C-related referral and treatment. Screening for hepatitis C in genito-urinary medicine clinics: a cost utility analysis. Cost-effectiveness and population outcomes of general population screening for hepatitis C. Cost-effectiveness of generic pan-genotypic sofosbuvir/velpatasvir versus genotypedependent direct-acting antivirals for hepatitis C treatment. The future of viral hepatitis testing: innovations in testing technologies and approaches. Hepatitis C disease burden and strategies to manage the burden (Guest Editors Mark Thursz, Gregory Dore and John Ward). Capacity enhancement of hepatitis C virus treatment through integrated, community-based care. Successful treatment of patients with hepatitis C in rural and remote Western Australia via telehealth. Telemedicine specialty support promotes hepatitis C treatment by primary care providers in the department of veterans affairs. Expansion of treatment for hepatitis C virus infection by task shifting to community-based nonspecialist providers: a nonrandomized clinical trial. Identifcation and clinical management of persons with chronic hepatitis C virus infection Cherokee Nation, 2012-2015. Hepatitis C elimination by 2030 through treatment and prevention: think global, act in local networks. Modelling the elimination of hepatitis C as a public health threat in Iceland: a goal attainable by 2020. National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on a National Strategy for the Elimination of Hepatitis B and C. Emerging epidemic of hepatitis C virus infections among young nonurban persons who inject drugs in the United States, 2006-2012. Hepatitis C care in the department of veterans affairs: building a foundation for success. The community response to viral hepatitis contributions towards achieving the goals of the viral hepatitis action plan. The current and future disease burden of chronic Hepatitis C virus infection in Egypt. Eliminating hepatitis C from Egypt: 2017 update on current trends and policyrecommendations policy brief (English). The role of screening and treatment in national progress toward hepatitis C elimination Georgia, 2015-2016. Cost-effectiveness of hepatitis C treatment for patients in early stages of liver disease. Hepatitis C virus prevention and treatment prioritization ethical, economic and evidential dimensions of early rather than delayed treatment for people who inject drugs. Strengthening hepatitis B and C surveillance in Europe: results from the two global hepatitis policy surveys (2013 and 2014). Hepatitis and liver cancer: a national strategy for prevention and control of hepatitis B and C (2010). If this happens, please ensure the patient understands they may have to pay some or all of the costs. Communication is key, so patients understand why you are recommending certain services and whether Medicare pays for them. Educate, counsel, Based on the results of the review and evaluation services in the previous and refer based on components, provide appropriate education, counseling, and referral. We invite your country to submit its monitoring data and narrative report for the year ending in December 2019. National consultation process during the 1st quarter of the year speeds up the consolidation and validation of the data; this reduces the need to exchange on the details, or going back to original sources of the data; 2. Involvement of civil society to the consultation is critical, especially in responding to the laws and policies related questions, and ensures that all relevant partners are engaged and play their important role in both implementation and reporting; 3. These guidelines describe in more detail the steps in collecting, analyzing, sharing and reporting the data, and the below fowchart helps in summarizing the process. It continues to be one of the leading international accountability mechanisms on any global commitment. These reports are designed to identify challenges and constraints, and to recommend actions to accelerate the achievement of targets. Countries are encouraged to integrate indicators into their ongoing monitoring efforts. Alternatively, countries can submit a recent national epidemiology and response overview report, if available. Indicator data are considered to be an integral part of each country progress report submission. For that reason, both the narrative portion of the country progress report and the indicator data should be considered in the consultation and report preparation process, as outlined in the section on Implementing monitoring at the national level. The procedures outlined in this manual should be used for collecting and calculating the necessary information for each indicator. Measurement tools and data sources the primary measurement tools vary by indicator and include the following: fi Nationally representative population-based sample surveys. Examples include work with young people, key populations at higher risk and pregnant women. In many countries, most of the data required for the national-level indicators may not be available from routine sources. Gathering indicator data may require adapting existing monitoring tools or adding specifc surveys. Spectrum fles are updated every year using the most recent programmatic and surveillance data. Country teams will receive information on the 2020 estimates process in November 2019. This step reduces both the data entry required and the chance for errors, and it improves the consistency of data between the two systems. The Spectrum fles are created by a team of national experts trained in the use of the software. Once the fnal Spectrum fle has been agreed upon by the country, these fnal data should be imported into the online reporting tool. Any data already entered for these selected indicators will be cleared out and replaced by Spectrum data during the import process. Click Add, select your national fle (or subnational fles, if available), then click Open. The system will list all of the indicator data from the imported fle, side-by-side with any data that have been entered in the system. You may select which set of data to use by ticking Use entered data or Take imported data from Spectrum. Click Save to save the settings and data sets that you have chosen to import, or click Cancel to abort the import process. If you have chosen to use the entered data instead of taking data from Spectrum, please be sure to go back to the data entry screens of those indicators to review and enter any missing data. Most national-level indicators use numerators and denominators to calculate the percentages that measure the state of the national response. Countries are strongly encouraged to pay close attention to the dates attached to specifc data when calculating an indicator: collecting data used for the numerator and denominator at different times will compromise the accuracy and validity of that information. The methods described have been designed to facilitate the construction of global estimates from national-level data. Although these methods can be applied at the subnational level, simpler, faster and more fexible approaches tailored to local conditions may be more appropriate to guide decision-making below the national level. Disaggregate the data, especially by sex and age One of the key lessons learned from previous rounds of reporting was the importance of obtaining disaggregated data: for example, breaking it down by sex and age, and providing it for specifc key populations or geographic locations. It is vital that countries collect data in their component parts and not simply in summary form. Without disaggregated data, monitoring the breadth and depth of the response to the epidemic at the national and global levels is diffcult. It is equally diffcult to monitor access to services, the equity of that access, the appropriateness of focusing on specifc populations and meaningful change over time. Key ministries should review their information systems, surveys and other instruments for collecting data to ensure that they capture disaggregated data at the subnational levels, including facility and project levels.
Stable angina arteria hyaloidea persistens buy cheap avalide 162.5 mg online, the most common type arteria zygomatico orbital buy generic avalide 162.5 mg on line, develops during physical activity and usually lasts a short time (approximately five minutes or less) if the physical activity has ended blood pressure medication memory loss order avalide without a prescription. Stress test without imaging: this heart-monitoring test is used to help evaluate how well the heart performs with activity arrhythmia icd 9 code generic 162.5 mg avalide overnight delivery. During a stress test blood pressure and age order avalide 162.5mg with amex, you will usually be asked to perform physical exercise blood pressure guidelines order avalide canada, like walking on a treadmill. Blood tests: the tests can identify certain enzymes such as troponin that leak into the blood after your heart has suffered severe angina or a heart attack. Additionally, the following imaging tests may be performed: Chest x-ray: this noninvasive imaging test helps your doctor rule out other sources of chest pain such as pneumonia. Imaging with x-rays involves exposing the chest to a small dose of radiation to produce pictures of the chest and heart. This imaging test combines special x-ray equipment with sophisticated computers to produce multiple images of the chest and heart. Contrast material is injected through a small line in the arm vein, similar to the ones used to draw blood. If there are areas with decreased blood flow, this could indicate plaque with blood vessel narrowing. This blood flow evaluation may be done twice during the exam with the use of a contrast material. The first time may be performed after the administration of a pharmaceutical, which stresses the heart like exercise. Performing the evaluation both with stress and rest helps determine if the decreased blood flow only occurs with exercise. This exam can also assess function of the heart and determine if there is any scar in the heart muscle. Catheter angiography: In this invasive imaging test, a thin, long plastic tube, called a catheter, is inserted into an artery in your groin or hand using a needle. The catheter is guided with a wire into the coronary arteries and is used to inject contrast material directly into the coronary arteries to determine whether there is any narrowing of the blood vessels. Narrowed portions of the vessels can be reopened using either a balloon or stents. Echocardiogram: During this test, a transducer that produces high-frequency sound waves is used to create moving images of the heart. If there is decreased motion within a portion of the wall of the heart, this could indicate decreased blood flow from narrowing of the coronary artery. Imaging can also be performed with a pharmaceutical agent stressing the heart to detect decreased motion in a portion of the heart muscle with stress. During an imaging stress test, the patient is usually asked to perform some kind of physical exercise like walking on a treadmill. A radioactive tracer will be injected into the blood during the peak of exercise and images of the heart will be taken. The radioactive tracer flows with the blood and will show whether there is an area of the heart with decreased blood flow. Many doctors may recommend certain lifestyle changes such as maintaining a healthy weight, consuming a balanced diet low in fats, discontinuing the use of tobacco products and finding ways to reduce stress. Additionally, you may also be treated with: Medication such as aspirin, statins, beta-blockers, calcium channel blockers, or nitrates. Angioplasty and vascular stenting: In selected cases, following appropriate testing, your doctor may perform angioplasty and stenting. This procedure, which uses balloons and/or stents, is performed to open the blockage in the coronary arteries and improve blood flow to the heart. Disclaimer this information is copied from the RadiologyInfo Web site. To ensure that, each section is reviewed by a physician with expertise in the area presented. However, it is not possible to assure that this Web site contains complete, up-to-date information on any particular subject. Do not attempt to draw conclusions or make diagnoses by comparing these images to other medical images, particularly your own. Only qualified physicians should interpret images; the radiologist is the physician expert trained in medical imaging. Commercial reproduction or multiple distribution by any traditional or electronically based reproduction/publication method is prohibited. These declines began in the late 1960s, and have continued to 2015, at varying rates, depending on diseases and age groups. Continued monitoring of changes in cardiovascular disease death rates provides the evidence that is needed to improve population-level prevention strategies for cardiovascular disease. In 2011, cardiovascular disease was the second most burdensome disease group in Australia, behind cancers, causing 15% of the total 4. Controlling risk factors for cardiovascular disease can result in large health gains in the population. It reduces the risk of onset of disease, the progression of disease, and the development of complications in those people with established disease. Despite the magnitude of the current cardiovascular disease burden, deaths from both coronary heart disease and stroke have declined substantially in Australia over the past 50 years. Levels peaked in the late 1960s and early 1970s, with cardiovascular disease responsible for 55% of all deaths each year (about 60,000 deaths). These falls are the result of a combination of improvements in preventing and detecting the disease, as well as clinical management of people who have it. While the falls in death rates for cardiovascular disease in Australia have been widely reported, trends in specifc age groups have received less attention. The slowing of falls in cardiovascular disease death rates are concerning, given the high disease burden, and the potential social and economic impacts. They highlight the need for efective and targeted prevention strategies (Sidney et al. This bulletin helps readers to understand recent trends in cardiovascular disease mortality in Australia, and how these trends have difered across age groups (see Box 1). It considers cardiovascular disease in total, followed by sections on coronary heart disease, heart attack (acute myocardial infarction), and cerebrovascular disease. This report focuses on the total population, and does not include trends by sex and population groups. Long-term trends in cardiovascular mortality Since the late 1960s and early 1970s, deaths from cardiovascular disease, coronary heart disease, and cerebrovascular disease have fallen markedly (Figure 1). The age-standardised death rate for cardiovascular disease rose steadily over the frst half of the 20th century. Between the early 1950s and the late 1960s it levelled, reaching a peak in 1968 of 830 deaths per 100,000 population. From 1968, the age-standardised rate fell by 82% to 151 per 100,000 population in 2015. The main driver of this decline was an 85% fall in coronary heart disease deaths between 1968 and 2015, from 428 to 66 deaths per 100,000 population. The fall in the cerebrovascular disease death rate also made a large contribution, falling by 82%, from 202 deaths per 100,000 population in 1974 to 36 deaths per 100,000 in 2015. The most common and serious forms of cardiovascular disease in Australia are coronary heart disease, stroke, and heart failure. When considered as a broad group of diseases, cardiovascular disease has been a major cause of death in Australia for many decades. In 2015, it was the second leading cause of death (almost 45,400 deaths, or 29% of total deaths), closely following all types of cancer. More than three quarters (78%) of these cardiovascular disease deaths were of people aged 75 and over, and slightly more than half (52%) were women. Over the 35 years from 1980 to 2015, the steady decline in cardiovascular disease death rates that began in the late 1960s has continued (Figure 1). The age-standardised death rate for cardiovascular disease fell by 73%, from 560 to 151 deaths per 100,000 population, or 3. Age-specifc trends While cardiovascular disease death rates fell substantially in each age group between 1980 and 2015, the rate of decline has varied across age groups (Figure 2). For many decades, coronary heart disease has been the single leading cause of death in Australia. In 2015, it was the underlying cause of death for almost 19,800 Australians, or 12% of total deaths. Three-quarters (74%) of these coronary heart disease deaths were of people aged 75 and over, and less than half (44%) were women. Among deaths attributed to coronary heart disease in 2015, heart attack was the underlying cause of more than 8,400 deaths, while chronic coronary heart disease was the underlying cause of more than 10,900 deaths. Over the 35 years from 1980 to 2015, the steady decline in coronary heart disease death rates that began in the late 1960s has continued (Figure 1). The age-standardised death rate for coronary heart disease fell by more than three-quarters (78%), from 297 to 66 deaths per 100,000 population, or 4. Age-specifc trends As for cardiovascular disease, coronary heart disease death rates fell substantially in each age group, with the rate of decline improving for older age groups (those aged 75 and over), but slowing among younger age groups. In 2015, heart attack was the underlying cause of death for 8,440 Australians, or 5% of total deaths. Over the 35 years from 1980 to 2015, the age-standardised death rate for heart attack fell by 86%, from 204 to 28 deaths per 100,000 population, or 5. Age-specifc trends Heart attack death rates fell substantially in each age group (Figure 4). But, as for coronary heart disease, while rates of decline have continued to improve for older age groups (those aged 75 and over), they have slowed among other age groups. Stroke is the most common form of cerebrovascular disease, accounting for 75% of cerebrovascular disease deaths. In 2015, cerebrovascular disease claimed almost 10,900 lives, or 7% of all deaths in Australia. Of these cerebrovascular disease deaths 84% were people aged 75 and over, and 60% were women. Among deaths attributed to cerebrovascular disease in 2015, haemorrhagic stroke was the underlying cause of 2,400 deaths, and ischaemic stroke the underlying cause of 1,200 deaths. Additionally, 4,700 deaths had stroke not specifed as haemorrhagic or ischaemic as the underlying cause, another 2,000 deaths were due to the sequelae (or late efects) of cerebrovascular disease, and 510 deaths were due to other cerebrovascular disease. Over the 35 years from 1980 to 2015, the age-standardised death rate for cerebrovascular disease fell by three-quarters (74%), from 140 to 36 deaths per 100,000 population, or 3. Age-specifc trends Cerebrovascular disease death rates fell substantially in each age group, with the rates of decline varying across age groups (Figure 5). This difers from coronary heart disease, where death rates among older age groups continue to improve. Treatment and medical care Advances in diagnosis and treatment of cardiovascular disease include the development of efective medications for treatment and control of high blood pressure, widespread use of statins to lower cholesterol levels, greater numbers of specialists and other health-care providers focusing on cardiovascular disease, better emergency medical services for heart attack and stroke, and an increase in specialised coronary care and stroke units. Each have contributed to lower case fatality rates and lengthened survival times (Brifa 2009, Ford & Capewell 2011). Risk factors Although cardiovascular disease death rates continue to decline overall in Australia, the rate of decline in younger age groups has slowed. In Australia and in other countries, this has been associated with a growing incidence of disease, and adverse changes in major risk factors at earlier ages (Mensah et al.
Children with minor illnesses blood pressure equation buy avalide 162.5mg otc, such as upper respiratory tract infections connexin 43 arrhythmia purchase avalide from india, may be immunized (see Vaccine Safety arteria tibialis anterior buy avalide 162.5 mg on-line, p 41) pulse pressure change during exercise buy 162.5 mg avalide with visa. However hypertension 3rd class medical buy generic avalide 162.5mg online, if other manifestations suggest a more serious illness zofran arrhythmia order avalide 162.5mg free shipping, the child should not be immunized until recovered. Hypersensitivity reactions occur rarely and usually are minor, consisting of wheal and fare reactions or urticaria at the injection site. Reactions have been attributed to trace amounts of neomycin or gelatin or some other component in the vaccine formulation. People with allergies to chickens or feathers are not at increased risk of reaction to the vaccine. Most often, however, neomycin allergy manifests as contact dermatitis, which is not a contraindication to receiving measles vaccine. The decision to immunize these children should be based on assessment of immunity after the frst dose and the benefts of protection against measles, mumps, and rubella in comparison with the risks of recurrence of thrombocytopenia after immunization. The risk of thrombocytopenia is higher after the frst dose of vaccine than after the second dose. The risk of exposure to measles for immunocompromised patients can be decreased by immunizing their close susceptible contacts. Children with a personal or family history of seizures should be immunized after parents or guardians are advised that the risk of seizures after measles immunization is increased slightly. In the immunization of adolescents and young adults against measles, asking women if they are pregnant, excluding women who are, and explaining the theoretical risks to others are recommended precautions. Every suspected measles case should be reported immediately to the local health department, and every effort must be made to obtain laboratory evidence that would confrm that the illness is measles, especially if the illness may be the frst case in the community. Subsequent prevention of spread of measles depends on prompt immunization of people at risk of exposure or people already exposed who cannot readily provide documentation of measles immunity, including the date of immunization. People who have not been immunized, including those who have been exempted from measles immunization for medical, religious, or other reasons, should be excluded from school, child care, and health care settings until at least 21 days after the onset of rash in the last case of measles. During measles outbreaks in child care facilities, schools, and colleges and other institutions of higher education, all students, their siblings, and personnel born in 1957 or after who cannot provide documentation that they received 2 doses of measles-containing vaccine on or after their frst birthday or other evidence of measles immunity should be immunized. People receiving their second dose as well as unimmunized people receiving their frst dose as part of the outbreak-control program may be readmitted immediately to the school or child care facility. The maculopapular and petechial rash is indistinguishable from the rash caused by some viral infections. Signs and symptoms of meningococcal meningitis are indistinguishable from those associated with acute meningitis caused by other meningeal pathogens (eg, Streptococcus pneumoniae). The overall case-fatality rate for meningococcal disease is 10% and is higher in adolescents. Less common manifestations of meningococcal infection include conjunctivitis, pneumonia, febrile occult bacteremia, septic arthritis, and chronic meningococcemia. Invasive infections can be complicated by arthritis, myocarditis, pericarditis, and endophthalmitis. A self-limiting postinfectious infammatory syndrome occurs in less than 10% of cases 4 or more days after onset of meningococcal infection and most commonly presents as fever and arthritis or vasculitis. Serogroup A has been associated frequently with epidemics outside the United States, primarily in sub-Saharan Africa. An increase in cases of serogroup W-135 meningococcal disease has been associated with the Hajj pilgrimage in Saudi Arabia. Since 2002, serogroup W-135 meningococcal disease has been reported in sub-Saharan African countries during epidemic seasons. The incidence of meningococcal disease varies over time and by age and location. During the past 60 years, the annual incidence of meningococcal disease in the United States has varied from 0. Serogroups B, C, and Y each account for approximately 30% of reported cases, but serogroup distribution varies by age, location, and time. Approximately three quarters of cases among adolescents and young adults are caused by serogroups C, Y, or W-135 and potentially are preventable with available vaccines. Since introduction in the United States of Haemophilus infuenzae type b and pneumococcal polysaccharide-protein conjugate vaccines for infants, N meningitidis has become the leading cause of bacterial meningitis in children and remains an important cause of septicemia. Historically, freshman college students who lived in dormitories and military recruits in boot camp had a higher rate of disease compared with people who are the same age and who are not living in such accommodations. Close contacts of patients with meningococcal disease are at increased risk of becoming infected. Patients are considered capable of transmitting the organism for up to 24 hours after initiation of effective antimicrobial treatment. Asymptomatic colonization of the upper respiratory tract provides the source from which the organism is spread. Outbreaks occur in communities and institutions, including child care centers, schools, colleges, and military recruit camps. However, susceptibility testing is not standardized, and clinical signifcance of intermediate susceptibility is unknown. Ceftriaxone clears nasopharyngeal carriage effectively after 1 dose and allows outpatient management for completion of therapy when appropriate. For patients with a serious penicillin allergy characterized by anaphylaxis, chloramphenicol is recommended, if available. If chloramphenicol is not available, meropenem can be used, although the rate of cross-reactivity in penicillin-allergic adults is 2% to 3%. The postinfectious infammatory syndromes associated with meningococcal disease often respond to nonsteroidal anti-infammatory drugs. Currently licensed vaccines are not 100% effective, and some cases will be caused by serogroup B. Rifampin, ceftriaxone, ciprofoxacin, and azithromycin are appropriate drugs for chemoprophylaxis in adults, but neither rifampin nor ciprofoxacin are recommended for pregnant women. If antimicrobial agents other than ceftriaxone or cefotaxime (both of which will eradicate nasopharyngeal carriage) are used for treatment of invasive meningococcal disease, the child should receive chemoprophylaxis before hospital discharge to eradicate nasopharyngeal carriage of N meningitidis. Ciprofoxacin, administered to adults in a single oral dose, also is effective in eradicating meningococcal carriage (see Table 3. For control of meningococcal outbreaks caused by vaccinepreventable serogroups (A, C, Y, and W-135), the preferred vaccine in adults and children 2 years of age and older is a meningococcal conjugate vaccine (see Table 3. Three meningococcal vaccines are licensed in the United States for use in children and adults against serotypes A, C, Y, and W-135. Both meningococcal conjugate vaccines are administered intramuscularly as a single 0. However, a 1 meningococcal conjugate vaccine is recommended for children and adolescents who are in high-risk groups as a 2-dose series at 9 months through 55 years of age (Table 3. Children 2 through 10 years of age who travel to or reside in countries in which meningococcal disease is hyperendemic or epidemic should receive 1 dose. Recurrent infection occurs throughout life and, in healthy people, usually is mild or asymptomatic. Serologic studies suggest that all children are infected at least once by 5 years of age. Prolonged shedding (weeks to months) has been reported in severely immunocompromised hosts. Serologic testing of acute and convalescent serum specimens is used in research settings to confrm the frst episode of infection. Data suggest that asymptomatic infection is more common than originally suspected. Multiple genera, including Encephalitozoon, Enterocytozoon, Nosema, Pleistophora, Trachipleistophora, Brachiola, and Vittaforma and Microsporidium, have been implicated in human infection, as have unclassifed species. Spores also have been detected in other body fuids, but their role in transmission is unknown. Use of stool concentration techniques does not seem to improve the ability to detect Enterocytozoon bieneusi spores. However, fumagillin is associated with signifcant toxicity, and recurrence of diarrhea is common after therapy is discontinued. None of these therapies have been studied in children with Microspordia infection. Molluscum contagiosum is a self-limited infection that usually resolves spontaneously in 6 to 12 months but may take as long as 4 years to disappear completely. Vertical transmission has been suggested in case reports of neonatal molluscum contagiosum infection. Infectivity generally is low, but occasional outbreaks have been reported, including outbreaks in child care centers. The incubation period seems to vary between 2 and 7 weeks but may be as long as 6 months. If questions persist, nucleic acid testing via polymerase chain reaction is available at certain reference centers. Adolescents and young adults with genital molluscum contagiosum should have screening tests for other sexually transmitted infections. Lesions in healthy people typically are self-limited, and treatment may not be necessary. However, therapy may be warranted to: (1) alleviate discomfort, including itching; (2) reduce autoinoculation; (3) limit transmission of the virus to close contacts; (4) reduce cosmetic concerns; and (5) prevent secondary infection. These options require a trained physician and can result in postprocedural pain, irritation, and scarring. Because physical destruction of the lesions is painful, appropriate local anesthesia is required. Cidofovir is a cytosine nucleotide analogue with in vitro activity against molluscum contagiosum; successful intravenous treatment of immunocompromised adults with severe lesions has been reported. For outbreaks, which are common in the tropics, restricting direct person-to-person contact and sharing of potentially contaminated fomites, such as towels and bedding, may decrease spread. Duration of carriage by infected and colonized children and the period of communicability are unknown. Culture of middle ear or sinus aspirates is indicated for patients with unusually severe infection, patients with infection that fails to respond to treatment, and immunocompromised children. Concomitant recovery of M catarrhalis with other pathogens (Streptococcus pneumoniae or Haemophilus infuenzae) may indicate mixed infection. Polymerase chain reaction tests for M catarrhalis are under development in research laboratories. If parenteral antimicrobial therapy is needed to treat M catarrhalis infection, in vitro data indicate that cefotaxime and ceftriaxone are likely to be effective. Approximately one third of infections do not cause clinically apparent salivary gland swelling and may be asymptomatic (subclinical) or may manifest primarily as respiratory tract infection. Mumps vaccine was licensed in the United States in 1967 and recommended for routine childhood immunization in 1977. Because 2 doses of mumps-containing vaccine are 1 not 100% effective, in settings of high immunization coverage such as the United States, most mumps cases likely will occur in people who have received 2 doses. The incubation period usually is 16 to 18 days, but cases may occur from 12 to 25 days after exposure. Students who continue to be exempted from mumps immunization because of medical, religious, or other reasons should be excluded until at least 26 days after onset of parotitis in the last person with mumps in the affected school. A second dose may be considered for preschool-aged children and other adults depending on outbreak epidemiology. Some studies and investigations conducted during the mumps outbreaks in the late 1980s and in 2006 indicate that vaccine-induced immunity might wane, possibly explaining the recent occurrence of mumps in the 15through 24-year age group. Adequate immunization is 2 doses of mumps-containing vaccine for school-aged children and adults at high risk (ie, health care personnel, students at post-high school educational institutions, and international travelers), and a single dose of mumps-containing vaccine for other adults born in or after 1957. Temporally related reactions, including febrile seizures, nerve deafness, aseptic meningitis, encephalitis, rash, pruritus, and purpura, may follow immunization rarely; however, causality has not been established. Allergic reactions also are rare (see Measles, Precautions and Contraindications [p 497], and Rubella, Precautions and Contraindications [p 634]). However, if other manifestations suggest a more serious illness, the child should not be immunized until recovered. People who have experienced anaphylactic reactions to gelatin or topically or systemically administered neomycin should receive mumps vaccine only in settings where such reactions could be managed and after consultation with an allergist or immunologist. Most often, however, neomycin allergy manifests as contact dermatitis, which is not a contraindication to receiving mumps vaccine (see Table 1. This interval is based on the assumptions that immunologic responsiveness will have been restored in 3 months and the underlying disease for which immunosuppressive therapy was given is in remission or under control. For patients who have received high doses of corticosteroids (2 mg/kg/day or greater or greater than 20 mg/day of prednisone or equivalent) for 14 days or more and who otherwise are not immunocompromised, the recommended interval is at least 1 month after corticosteroids are discontinued (see Immunocompromised Children, p 74). Mumps immunization during pregnancy has not been associated with congenital malformations (see Measles, p 489, and Rubella, p 629). Bullous myringitis, once considered pathognomonic for mycoplasma, now is known to occur with other pathogens as well. Acute bronchitis and upper respiratory tract illness caused by M pneumoniae generally are mild and self-limited. Bilateral diffuse infltrates or focal abnormalities, such as consolidation, effusion, or hilar adenopathy can occur. Mycoplasma hominis infection has been reported in neonates (especially at scalp electrode monitor site) and children (both immunocompetent and immunocompromised).
Additional information: