Joseph E. Levitt, MD
- Assistant Professor of Medicine, Department of Internal Medicine,
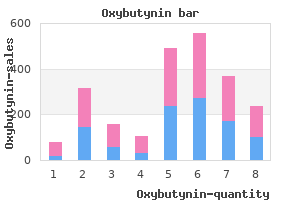
- Division of Pulmonary & Critical Care, Stanford University Medical
- Center, Stanford, CA, USA
There is further subdivision into eight segments based on portal venous symptoms 3 months pregnant cheap oxybutynin 2.5mg, hepatic arterial and bile duct anatomy treatment degenerative disc disease generic oxybutynin 5mg line, first described by Couinaud [3] medicine pouch order oxybutynin american express. The majority of the liver is covered by visceral peritoneum which condenses to form the diaphragmatic attachments of the coronary treatment shingles oxybutynin 5mg without a prescription, left and right triangular symptoms bacterial vaginosis 2.5 mg oxybutynin overnight delivery, and falciform ligaments medicine lux purchase generic oxybutynin on line. Thereisaclearpatterntothedistributionof injury with blunt mechanisms prevailing in European reports [5, 6], usually as the occupant of a motor vehicle [7] compared to a preponderance of penetrating injury in North America [8] and South Africa [9]. Blunt injury causes either deceleration or crush pattern injuries, with deceleration resulting in movement of the liver against its attachments and crush causing direct compression of the hepatic parenchyma. The distinction is important as deceleration injuries tend to create lacerations, primarily within the right lobe, which can include vascular disruption, whereas direct crush tends to involve the central parts of the liver [10]. In patients who are hemodynamically stable, a careful history from the patient, witnesses, and emergency services can provide useful information in predicting the likely pattern of potential hepatic injuries. TheHepaticInjuryScale(Table1)isthemostcom monly used grading system and was produced by the Organ Injury Scaling Commit tee of the American Association for the Surgery of Trauma in 1989 [12] and subse quently revised in 1994 [11]. Initial Management and Investigation Early management should be in accordance with a set trauma protocol, such as the Advanced Trauma Life Support guidelines of the American College of Surgeons Committee on Trauma [14], with attention first directed to airway maintenance and ventilation. The key underlying determinant of subsequent management is, of course, hemo dynamic stability. Unstable patients, in the context of abdominal injury with signs of peritonism, should undergo immediate resuscitative laparotomy without further investigation [14]. However, emergency room laparotomy for those too unstable to survive transfer to the operating room is probably futile [8, 17]. Irrespective of hemodynamic stability, all cases of gunshot wound to the abdomen require explor atory laparotomy, given the radiological difficulties in following a bullet track [18]. In cases where hemodynamic stability is maintained with or without volume resuscitation, and abdominal injury is suspected, prompt radiological imaging 668 A. This patient was managed non operatively on liver intensive care and did not develop any late com plications. Features of the plain trauma series radiographs, which are suggestive of hepatic injury include fractures of the lower ribs, elevation of the right hemi-diaphragm and loss of the psoas shadow [10]. The timing of scan is an important consideration and there is some suggestion that increasing the duration between injury and scanning aids differentiation between hematoma and lacerations [20]. Definitive Management of Liver Trauma Following the acute assessment and initial resuscitation, patients must be selected for either an operative or non-operative approach to management with a conserva tive approach appropriate in around 80% of cases [26]. For both groups, possible complications include early hemorrhage and later bile leak or intra-abdominal collections [26]. Overall, a non-operative approach is associated with a lower transfusion require ment and a lower incidence of abdominal complications [26]. The association of solid organ injury with damage to a hollow viscous is a concern in both groups and, for the non-operative cases especially, a careful review of the radiological imaging is required to exclude concomitant damage in the knowledge that incidence increases with the number of solid organs injured [28]. The outcome after liver trauma has been shown to be dependent on the severity of the liver injury, the mechanism, and also the presence of any other associated injuries [8] with a commonly quoted overall mortality of around 12%. Only one study primarily addressed mortality based on grade of liver injury and a summary of these 175 patients is displayed in Table 2 [6]. Whether or not the patient undergoes surgery the intra-abdominal pressure should be routinely measured and if high, in the presence of organ dysfunction, decompression should be performed. Following decompres sion, or if the abdominal wall is found to be tight at the time of closure following operative management, a temporary abdominal dressing will be required. Several other techniques are described for temporary abdominal closure and at present none has been shown to be superior in the context of a randomized trial. Non-operative Management of Liver Trauma the conservative approach to liver trauma has evolved from pediatric practice [30] and is now well established in the adult setting [31]. The patient must be placed appropriately, usually within the critical care unit, and certainly within an area allowing close monitoring of hemodynamic and hema tological parameters. In addition, repeated clinical examination, ideally by the same clinician, is essential. As an absolute minimum, the entirely stable patient requires frequent checks of heart rate and non-invasive blood pressure, with wide bore venous access in place, although some units would advocate a more aggressive approach and there arenoevidencebasedguidelines. In cases managed non-operatively, hemodynamic instability is an absolute indica 670 A. The liver does, however, have a remarkable capacity to bleed substan tially and then spontaneously stop, so the presence of a large amount of intra-perito neal blood is not an indication for laparotomy per se, unlessitisaccompaniedby hemodynamic instability. Despiterecommendationsthatrepeatedscansonlybeperformedintheeventof clinical deterioration [33], it has been found that 49% of follow-up scans after oper ative management of severe liver injuries demonstrate new liver related complica tions [34], most of which require intervention. Late complications of liver injury can occur following non-operative and opera tive management and include secondary bleeding (usually from pseudoaneurysms. The second image is obtained following control of the aneu rysm by selective coil embolization of the right hepatic artery. Operative Management of Liver Trauma Patients undergoing primary operative management of liver trauma are, by defini tion, hemodynamically unstable, and can also be expected to exhibit other features of critical illness such as coagulopathy, renal dysfunction, and acute lung injury. The chosen surgical intervention should reflect this fact and, by and large, be limited to 672 A. Wendon damage control procedures [37], with the key underlying principle being to limit intervention as far as possible. In an ideal world, such patients should be managed by specialist hepato-biliary surgeons; however the majority of unstable liver injuries will be treated initially by general or trauma surgeons at the admitting hospital. In this setting, the only appro priate intervention is packing of the liver via a midline laparotomy [38], with subse quent transfer as indicated. Specialist surgical interventions include liver resection, selective hepatic artery embolization, repair of hepatic vein or caval injuries, and ex-vivo liver resection or liver transplantation. The various surgical strategies will be briefly described, along with their relative merits, however, this chapter is by no means a definitive surgical text. Isolated injury to the extra-hepatic biliary tree is encountered only rarely in the trauma population and the mainstay of treatment is control of hemorrhage with adequate drainage pending definitive reconstruction [39]. Isolated gall bladder inju ries may be treated by primary cholecystectomy; however, traumatized bile ducts are best treated by biliary-enteric anastamosis with a roux-en-Y type reconstruction in a manner identical to the management of iatrogenic injuries [40]. Temporary packing has been shown to be effective in the majority of patients, the exception being in the presence of major vascular injury [41]. When stable, the packs can be gently removed from each quadrant in turn and the injuries carefully evaluated. When the right upper quadrant packs are removed it may be possible to control light bleeding with diathermy (ideally via argon beam coagulater, which prevents the tip of the diathermy probe becoming adherent to the tissues [42]), direct pressure applied for several minutes or the topical application of synthetic absorbable hemo static materials. Inflowcontrolmay arrest the bleeding and allow sufficient time for clot formation (especially if any coa gulopathy is reversed during this time by the intravenous administration of clotting factors), and can be maintained for up to one hour [43]. Bleeding that is temporarily controlled by inflow occlusion is likely to be arterial in origin and may require liga tion of the relevant right or left branch. This is, however, a relatively demanding procedure in the face of active hemorrhage. Continued bleeding with the inflow clamped indicates hepatic vein or caval injury, both of which lie behind the liver and are relatively inaccessible. In such cir cumstances, manipulation and mobilization of the liver should be kept to a mini mumasitmayleadtoextensionofvenouslacerationsorairembolismandthecom bination of the weight of the liver and packing can be utilized to tamponade the bleeding, pending specialist input. Packs have been forced into the cavity formed by the initial lacera tion causing further parenchymal disruption and the radio-opaque tapes of the packs are clearly seen within the liver substance. At lapa rotomy, amongst other injuries, the right hepatic artery was found to have been completely transected in the packed cavity. The technique for packing is important, and ideally, the liver should be partially mobilized from its diaphragmatic attachments for packs to be inserted over the superior border. Under no circumstances should packs be inserted into cavities within the liver parenchyma as this will lead to further distraction and disruption of blood vessels. Such cavities should be manually closed and held in position by direct pressure and peri-hepatic packing. The former practice of hepatorrhaphy, whereby sutures are used to compress the hepatic parenchyma, is best avoided due to the risk of inducing hepatic necrosis with subsequent infection [2, 13]. It is gener ally accepted that packs should not remain in position for more than three days due to the risk of infection [41] and that intravenous antibiotic and anti-fungal prophy laxis should be administrated [44]. Following immediate stabilization, transfer of a patient with significant liver trauma to a specialist hepato-biliary surgical unit should be considered as early as possible, even if the initial management has been non-operative. Specialist Surgical Interventions Following transfer, reassessment of hemodynamic stability will take place. The indications for surgery are the same (hemodynamic instability or concurrent injury to other vis cera requiring surgical intervention) and packing remains the mainstay of hemor rhage control. Occasionally, further surgery is necessary but this is best performed after the patient has been fully stabilized in terms of hemodynamics, coagulation, and temperature and should only be undertaken by an experienced specialist sur geon. Liver resection Resectional debridement involves the non-anatomical excision of devitalized liver tissue along the lines of the previous injury [9]. Particular attention must be made to identifying and ligating or repairing segmental bile ducts to avoid subsequent bile leak. Formal anatomical liver resection in the context of acute trauma with active bleeding is a technically difficult exercise and is best avoided. There are only a few reports from highly specialized centers where this technique has been employed suc cessfully in preference to resectional debridement for injuries involving major ves sels or bile ducts [45, 46]. Selective Hepatic Artery Ligation and Embolization Although surgical ligation of the hepatic artery or its branches has been largely dis placed by modern surgical techniques it does remain a viable option where peri hepatic packing fails to control hemorrhage and temporary hepatic artery occlusion is effective [13]. Radiological embolization by placement of coils and/or gel within the arterial tree is an emerging interventional option and data, although limited, are encouraging [47]. The technique has been described for acute and life-threatening hemorrhage from a hepatocellular adenoma [48] and also in the treatment of post-traumatic pseudoaneurysm [35]. Angiography with a view to embolization should now be the investigation of choice for suspected arterial bleeding in a stable patient. As with surgical ligation, gangrenous cholecystitis remains a possible complica tion where the right hepatic artery has been occluded [49] (and sometimes follow ing packing). Repair of Hepatic Vein and Caval Injuries Failure of the Pringle maneuver to arrest the hemorrhage raises the possibility of either aberrant vascular anatomy or else hepatic vein or caval injury. In this situa tion, the most common abnormality is an anomalous right hepatic artery arising from the superior mesenteric artery which is present in around 15% of cases and is usually located posteriorly at the porta hepatis [3]. In order to achieve total vascular exclusion of the liver, in addition to inflow con trol as previously described, it is also necessary to occlude the supra-hepatic and infra-hepaticvenacavaand, inthecontextoftrauma, thismaneuverisusuallycom bined with a shunting procedure to maintain venous return. Such injuries carry a reported mortality of between 50 and 80% [50] with very few centers having any great experience. In one of the largest series, from China, isolated left hepatic vein injury was associated with a higher survival (five out of five survivors) than isolated right hepatic vein (8% mortality) and combined right and left hepatic vein (100% mortality) [51]. Liver Transplantation Data on acute liver transplantation due to uncontrollable hemorrhage are extremely limited. The only true series considered eight patients who underwent total hepa tectomy with temporary portocaval shunting as a life-saving manuever following failure of other surgical procedures. Beyond this small series, occasional case reports exist, however the out come of transplantation for primary hemorrhage control is universally poor [51]. The Management of Liver Trauma 675 Some success has been seen with transplantation for the treatment of sub-acute liver failure due to reperfusion injury on removal of tight packs. In these circumstances, profound hemodynamic and respiratory compromise occur in the operating room, whichisirreversibleandmayonlybecontrolledbytotalhepatectomy. Suchpatients must be super-urgently listed for transplantation and will only survive if a suitable donor liver becomes available within two to three days of the patient being anhepa tic. Conclusion Despite its relatively protected location, the liver is the most commonly injured intra-abdominal organ and liver injury is often associated with injuries to other structures. The majority of liver injuries can be managed non-operatively and grade of injury is not useful in selecting patients for, or predicting outcome of, non-opera tive management. The initial management of liver injuries is effective trauma resus citation and prompt transfer of unstable patients to the operating room, where cor rectly performed peri-hepatic packing can be a life-saving, temporizing measure. The effective surgical management of complex hepatic injuries is best provided in a dedicated specialist center with access to the appropriate surgical, radiological and critical care expertise. High energy deceleration injuries resulting in significant juxta-hepatic vascular and caval injuries are accompanied by an extremely high mortality rate despite aggressive surgical intervention but there is no clear role for acute liver transplantation in these cases at present. Toro K, Hubay M, Sotonyi P, Keller E (2005) Fatal traffic injuries among pedestrians, bicy clists and motor vehicle occupants. Yokota J, Sugimoto T (1994) Clinical significance of periportal tracking on computed tomo graphic scan in patients with blunt liver trauma. Demetriades D, Karaiskakis M, Alo K, Velmahos G, Murray J, Asensio J (2003) Role of post operative computed tomography in patients with severe liver injury. Laopaiboon V, Aphinives C, Pugkem A, Thummaroj J, Puttharak W, Soommart Y (2006) Selective transcatheter embolization for treatment of post-traumatic hepatic artery and por tal vein pseudoaneurysms. Ringe B, Pichlmayr R (1995) Total hepatectomy and liver transplantation: a life-saving proce dure in patients with severe hepatic trauma.
Verification of endotracheal tube placement following intubation symptoms of anemia 5mg oxybutynin visa, Prehosp Emerg Car symptoms nicotine withdrawal cheap 2.5mg oxybutynin with visa. A comparison of GlideScope video laryngoscopy versus direct laryngoscopy intubation in the emergency department treatment yellow tongue cheap 5 mg oxybutynin fast delivery. Comparison of a conventional tracheal airway with the Combitube in an urban emergency medical services system run by physicians symptoms 24 hour flu purchase 2.5 mg oxybutynin with mastercard. Can an airway assessment score predict difficulty at intubation in the emergency department Apneic oxygenation may not prevent severe hypoxemia during rapid sequence intubation: a retrospective helicopter emergency medical service study medicine 0025-7974 order generic oxybutynin line. Before and after establishment of a rapid sequence intubation protocol for air medical use medicine 513 cheap 5mg oxybutynin mastercard. Endotracheal intubation and esophageal tracheal Combitube insertion by regular ambulance attendants: a comparative trial. The effectiveness of out-of-hospital use of continuous end-tidal carbon dioxide monitoring on the rate of unrecognized misplaced intubation within a regional emergency medical services system. Utility of a novel quantitative handheld microstream capnometer during transport of critically ill children. Prehospital endotracheal intubation for trauma does not improve survival over bag-valve-mask ventilation. The assessment of three methods to verify tracheal tube placement in the emergency setting. Noninvasive ventilation in the pediatric intensive care unit for children with acute respiratory failure. A comparison of the GlideScope video laryngoscope and standard direct laryngoscopy in children with immobilized cervical spine. Failed prehospital intubations: an analysis of emergency department courses and outcomes. Comparison of traditional versus video laryngoscopy in out-of hospital tracheal intubation. Barriers to adoption of evidence based prehospital airway management practices in California. Revision Date September 8, 2017 172 Bronchospasm (due to Asthma and Obstructive Lung Disease) (Adapted from an evidence-based guideline created using the National Prehospital Evidence-Based Guideline Model Process) Aliases Asthma, respiratory distress, wheezing, respiratory failure, bronchospasm, obstructive lung disease, albuterol, levalbuterol, duoneb, nebulizer, inhaler Patient Care Goals 1. Deliver appropriate therapy by differentiating other causes of respiratory distress Patient Presentation Inclusion Criteria 1. Wheezing will have expiratory wheezing unless they are unable to move adequate air to generate wheezes ii. Respiratory distress due to a presumed underlying cause that includes one of the following: a. Concurrent symptoms (fever, cough, rhinorrhea, tongue/lip swelling, rash, labored breathing, foreign body aspiration) c. Usual triggers of symptoms (cigarette smoke, change in weather, upper respiratory infections) d. Escalate from a nasal cannula to a simple face mask to a non-rebreather mask as needed, in order to maintain normal oxygenation b. Suction the nose and/or mouth (via bulb, Yankauer, suction catheter) if excessive secretions are present 3. Albuterol 5 mg nebulized (or 6 puffs metered dose inhaler) should be administered to all patients in respiratory distress with signs of bronchospasm. Bag-valve-mask ventilation should be utilized in children with respiratory failure 9. Giving positive pressure in the setting of bronchoconstriction, either via a supraglottic airway or intubation, increases the risk of air trapping which can lead to pneumothorax and cardiovascular collapse. These interventions should be reserved for situations of respiratory failure Notes/Educational Pearls Key Considerations 1. Patients with known asthma who complain of chest pain or shortness of breath should be empirically treated, even if wheezing is absent. Intravenous versus oral corticosteroids in the management of acute asthma in children. Inhaled salbutamol (albuterol) vs injected epinephrine in the treatment of acute asthma in children. Bilevel positive airway pressure in the treatment of status asthmaticus in pediatrics. Asthma severity scores for preschoolers displayed weaknesses in reliability, validity, and responsiveness. Effects of ipratropium bromide nebulizer solution with and without preservatives in the treatment of acute and stable asthma. Does noninvasive positive pressure ventilation improve outcome in acute hypoxemic respiratory failure Managing asthma exacerbations in the emergency department: summary of the National Asthma Education and Prevention Expert Panel Report 3 guidelines for the management of asthma exacerbations. Noninvasive positive pressure ventilation for the treatment of status asthmaticus in children. The efficacy of nebulized albuterol/ipratropium bromide versus albuterol alone in the prehospital treatment of suspected reactive airways disease. The pediatric respiratory assessment measure: A valid clinical score for assessing acute asthma severity from toddlers to teenagers. Addition of long-acting beta2 agonists to inhaled corticosteroids versus same dose inhaled corticosteroids for chronic asthma in adults and children. Early use of inhaled corticosteroids in the emergency department treatment of acute asthma. Effectiveness of nebulized salbutamol administered in ambulances to patients with severe acute asthma. Pediatric myocarditis: emergency department clinical findings and diagnostic evaluation. Randomized trial of single-dose intramuscular dexamethasone compared with prednisolone for children with acute asthma. Time saved with use of emergency warning lights and sirens during response 177 to requests for emergency medical aid in an urban environment. Effect of injected long-acting epinephrine in addition to aerosolized albuterol in the treatment of acute asthma in children. Predicting the need for hospitalization in acute childhood asthma using end-tidal capnography. Bronchiolitis management preferences and the influence of pulse oximetry and respiratory rate on the decision to admit. Oxygen saturation as a predictor of prolonged, frequent bronchodilator therapy in children with acute asthma. Should inhaled anticholinergics be added to beta2 agonists for treating acute childhood and adolescent asthma Prospective, randomized trial of epinephrine, metaproterenol, and both in the prehospital treatment of asthma in the adult patient. Non-invasive positive pressure ventilation for treatment of respiratory failure due to severe exacerbations of asthma. Out-of-hospital administration of albuterol for asthma by basic life support providers. Magnesium sulfate for treating exacerbations of acute asthma in the emergency department. Effectiveness of steroid therapy in acute exacerbations of asthma: a meta-analysis. Early emergency department treatment of acute asthma with systemic corticosteroids. Nebulized dexamethasone versus oral prednisone in the emergency treatment of asthmatic children. Comparison of nebulized terbutaline and subcutaneous epinephrine in the treatment of acute asthma. Direct supportive efforts towards decreasing afterload and increasing preload Patient Presentation Inclusion Criteria 1. Clinical impression consistent with congestive heart failure Exclusion Criteria 1. If suspect high altitude pulmonary edema, treat per the Altitude Illness guideline Patient Safety Considerations No recommendations Notes/Educational Pearls Key Considerations 1. Theoretical risk of hypotension and pneumothorax as non-invasive positive pressure ventilation increases intrathoracic pressure which decreases venous return and cardiac output iii. Allow patient to remain in position of comfort patients may decompensate if forced to lie down 4. Examples are: sildenafil (Viagra, Revatio ), vardenafil (Levitra, Staxyn ), tadalafil (Cialis, Adcirca ) which are used for erectile dysfunction and pulmonary hypertension. Also avoid use in patients receiving intravenous epoprostenol (Flolan ) or treporstenil (Remodulin ) which is used for pulmonary hypertension. Nitroglycerin reduces left ventricular filling pressure primarily via venous dilation. At higher doses the drug variably lowers systemic afterload and increases stroke volume and cardiac output. Pulmonary edema is more commonly a problem of volume distribution than overload, so administration of furosemide provides no immediate benefit for most patients. High-dose nitrates can reduce both preload and afterload and potentially increase cardiac output. A concern with high doses of nitrates is that some patients are very sensitive to even normal doses and may experience marked hypotension. It is therefore critical to monitor blood pressure during high-dose nitrate therapy. Effectiveness of prehospital continuous positive airway pressure in the management of acute pulmonary edema. Out of hospital continuous positive airway pressure ventilation versus usual care for acute respiratory failure: A randomized controlled trial. Paramedic identification of acute pulmonary edema in a metropolitan ambulance service. Revision Date September 8, 2017 183 Trauma General Trauma Management Aliases None noted Patient Care Goals 1. Rapid and safe transport to the appropriate level of trauma care Patient Presentation Inclusion Criteria 1. Patients of all ages who have sustained an injury as a result of mechanical trauma. Assess for and stop severe hemorrhage [see Extremity Trauma/External Hemorrhage Management guideline] b. Assess airway patency by asking the patient to talk to assess stridor and ease of air movement ii. Look for injuries that may lead to airway obstruction including unstable facial fractures, expanding neck hematoma, blood or vomitus in the airway, facial burns/inhalation injury iii. Signs of hemorrhagic shock include: tachycardia, hypotension, pale, cool clammy skin, capillary refill 2 seconds 184 f. Evaluate for clinical signs of traumatic brain injury with herniation including: 1. Rapid evaluation of entire body to identify sites of penetrating wounds or other blunt injuries. Stop severe hemorrhage [see Extremity Trauma/External Hemorrhage Management guideline] 2. Establish patent airway with cervical spine precautions, per the Airway Management and Spinal Care guidelines b. If respiratory efforts are inadequate, assist with bag-mask ventilation and consider airway adjuncts. If patient is unable to maintain airway, consider oral airway (nasal airway should not be used with significant facial injury or possible basilar skull fracture) c. If impending airway obstruction or altered mental status resulting in inability to maintain airway patency, secure definitive airway 3. If absent or diminished breath sounds in a hypotensive patient, consider tension pneumothorax and perform needle decompression b. If pelvis is unstable and patient is hypotensive, place pelvic binder or sheet to stabilize pelvis b. Minimize scene time (goal is under 10 minutes) and initiate rapid transport to the highest level of care within the trauma system. Palpate head and scalp and face and evaluate for soft tissue injury or bony crepitus 2. Palpate once for instability by applying medial pressure on the iliac crests bilaterally vi. Splint obvious extremity fractures per the Extremity Trauma/External Hemorrhage Management guideline iii. Provide pain medication per the Pain Management guideline Patient Safety Considerations 1. Life-threatening injuries identified on primary survey should be managed immediately with rapid transport to a trauma center, while the secondary survey is performed enroute 2. Patients with compensated shock may not manifest hypotension until severe blood loss has occurred b. Patients with traumatic brain injury may deteriorate as intracranial swelling and hemorrhage increase 3.
Order cheapest oxybutynin. Five early symptoms of pneumonia parents must watch out for.
Spot pulse oximetry in these circumstances is of no clinical value and frequently results in unnecessary application of supplemental oxygen medicine 3x a day 5mg oxybutynin free shipping. Respiratory rate and effort combined with auscultory findings medications while pregnant order cheap oxybutynin line, radiograph medicine 751 m buy 2.5mg oxybutynin with visa, and subjective patient complaints are much better determinants of respiratory failure than arterial desaturation medicine 627 generic 5mg oxybutynin with visa. In the latter circumstance medications 126 purchase generic oxybutynin pills, supplemental oxygen should be used along with pulmonary toilet symptoms migraine cheap oxybutynin 5 mg fast delivery. Central nervous system injury Patients with head and/or spinal cord injury do not have normal pulmonary toilet. These patients rely heavily on positioning, mobilization, and active pulmonary toilet to avert respiratory failure. Nasotracheal suctioning along with chest physiotherapy, bronchodilators, and breathing exercises should be used liberally in this patient group. Tracheostomy Tracheostomy is frequently required for the management of airway, pulmonary toilet, and/or respiratory failure in patients with complex critical illness and/or injury. The vast majority of these are performed percutaneously although some are still placed using the older, but still reliable, open surgical technique. Regardless of placement technique, complications, daily tracheostomy tube/site care, and downsizing/decannulation are the same. Complications Dislodgement: the most common early and lethal complication of tracheostomy is tube dislodgement. In order to prevent this complication the tracheostomy tube is secured to the skin with sutures and fixed in place with a secure neck strap. Sutures often give a false sense of security and will not in and of themselves eliminate dislodgement. The most important defense against early dislodgement is a secure neck strap and strict avoidance of undue tension and/or torque on the fresh tracheostomy. After four days, dislodgement rarely 141 results airway compromise and the tube can simply be reinserted through the neck. Prior to four days, airway loss is likely and the patient may require endotracheal intubation to reestablish the airway. This is a true emergency that requires the immediate attention of the surgical house staff. The patient can be temporized with 100% oxygen delivered via bag valve mask and gentle occlusion of the tracheostomy site. Plugging: the most common intermediate complication of tracheostomy is mucous plugging. Secretions build up in the tracheostomy tube lumen leading to sudden occlusion and airway compromise. The routine practice of maintaining cuff deflation and routine inspection/cleaning of the inner cannula will prevent this complication. Virtually all tracheostomies (85%) are associated with some degree of tracheal stenosis. Only 1-2% of patients develop critical stenosis that compromises the airway and produces clinical symptoms. The duration of endotracheal intubation (> 11 days) prior to tracheostomy, technique used (open > percutaneous), higher placement (between rings 1-2 vs. Almost all clinically significant stenosis occur within twelve weeks of tracheostomy. The hallmark of clinically significant tracheal stenosis is respiratory distress and/or stridor and wheezing when the tracheostomy tube is plugged or removed. If plug removal or tracheostomy tube reinsertion alleviates symptoms the tube should remain in place until a diagnostic evaluation can be performed. Tracheal-arterial fistula: Small amounts of bleeding may occur simply from the irritation of suctioning, site care and/or the tube itself. A rare but lethal complication of tracheostomy is tracheal-arterial fistula that occurs from erosion of the tip of the tracheostomy tube into the great vessels of the upper thorax. If bleeding persists or produces airway compromise, the endotracheal tube cuff can be inflated to tamponade bleeding and maintain the airway. Site care and appropriate antimicrobial therapy are effective in controlling this complication. Tracheocutaneous fistula: this is a rare complication of tracheostomy that is defined as a persistent air leak present for more than one week after decannulation. While a small percentage of these will close after 7 days most will require a surgical intervention to achieve closure. Bronchorrea: Copious secretions usually indicate a residual or recurrent pulmonary problem. If the patient still requires a tracheostomy (coma), a drying agent such as robinol can be used. Tracheostomy tube/site care the tracheostomy tube and site should be inspected at least once daily. Gentle cleansing with a small amount of soap and water followed by a dry dressing provides ample site care. The inner cannula should be removed, inspected, and cleaned as necessary to remove build up of dried secretions. The tracheostomy tape should be snug enough to prevent excess movement of the tube but not so tight as to produce skin breakdown/ulceration. Tracheostomy bypasses the normal humidification provided by the oro/nasopharynx so patients are prone to evaporative water loss and desiccation of the airway mucosa. Humidified air or oxygen (if required) should be used at all times to prevent the latter complications. Downsizing and decannulation the general practice of downsizing a tracheostomy tube prior to decannulation is controversial. The stated advantages are a reduction in size of the tract to reduce tracheocutaneous fistulas and to detect tracheal stenosis prior to decannulation. After four days a well-established tract exists between the surface and the trachea. Respiratory failure should be stable or improving and suctioning requirements should be nominal (>2-4 hours). As a first step, the plastic tracheostomy tubes (Usually Shiley occasional Portex or Bivona) are removed and replaced with a 6mm metal tube (Jackson). If the patient tolerates plugging (see complications: tracheal stenosis), has a good cough and minimal secretions, decannulation can proceed. The patient should be monitored closely over the next 24 hours for any evidence of respiratory distress. Dysphagia and aspiration following tracheostomy Dysphagia and/or aspiration following tracheostomy are very common. If managed correctly, this is rarely a clinical problem and oral feeding can be safely resumed without an elaborate ritual. Almost 30% percent of normal individuals will have some amount of aspiration on barium swallow. Contrast studies often overestimate the problem and lead to unnecessary, complicated, and expensive solutions to a simple problem. This is complicated by the fact that the tracheostomy itself may interfere with swallowing. To initiate oral intake, cuffed tracheostomy tubes should be deflated or downsized to a smaller metal tracheostomy. The initial oral feeding challenge should be with thickened liquids and/or solids. Intravenous Access Three quarters (75%) of all hospital bactermia events are associated with intravenous catheters! Many catheters are placed under less than ideal conditions and should be removed as soon as possible. Proper inspection and site care should be used to maintain function and sterility. There is a widely held misconception that more frequent wound care somehow makes wounds heal faster. Keeping wounds clean, moist, and covered allows the body to heal the wounds considerably faster. Astringents, frequent dressing care, and overzealous packing are more often responsible for delays in healing. Wound Classification Clean Wounds these are surgical incisions that follow an elective surgical procedure that does not involve the aerodigestive tract. Examples would be neurosurgical procedures, vascular procedures, hernias, most elective orthopedic procedures. The difference between contaminated and dirty wounds is really the degree of contamination. Complex wounds with large devitalized areas, gross fecal contamination, large amounts of purulent material, dirt, foreign bodies etc. Dehiscence can further defined as involving the skin and subcutaneous tissue (superficial) or extending to the deeper layers (fascial dehiscence). Not all dehiscence has evisceration but by definition all eviscerations have dehiscence. Bacterial counts are lowest in the wound at this point and delayed primary closure has the greatest success. After that point it is very unlikely that environmental contamination would compromise the wound. After that point the wounds can be covered with a light dry dressing to absorb minor drainage, prevent irritation and for patient comfort. These wounds should be carefully inspected at least once a day for signs of infection (redness, swelling, excessive tenderness, purulent drainage). The subjective patient complaint of wound pain (fever may or may not be present) that increases or is out proportion to wound size is often the earliest sign of surgical wound infection. The main clinical reason for this practice is the high incidence of wound infection if the wounds are closed. The wounds are generally packed tightly to achieve hemostasis after the initial operative procedure. Unless there is a planned return to 144 the operating room for exam under anesthesia, further debridement, and irrigation, these dressings should be taken down and the wound examined at 24 hours. The first dressing change can be quite painful and provisions should be made for adequate analgesia prior to proceeding. Most of the pain emanates from the densely innervated wound edge and care should be taken in this area. If the dressing is adherent gentle wetting with saline will facilitate removal and reduce discomfort. At the first dressing change the decision can be made to initiate saline wet to dry dressing or application of a vacuum dressing. At this point a decision can also be made about washing/showering the wound with soap and water. Dressing changes need only be once or twice a day and packing of the wound should be gentle. As mentioned previously, astringents should be avoided and every effort should be made to avoid wound dessication by irrigating the wound in between dressing changes if necessary. Regarding dressing fixation, the skin should be protected from tape adhesives by using duoderm and Montgomery straps or by application of Bandnet dressing (preferred). Patients should be given clear instructions on clean wound care, showering should be encouraged. When possible, wounds can/should be dressed with tap water rather than sterile saline which is considerably more expensive and unnecessary for most wounds. Dehydration from evaporative water loss and malnutrition from protein loss are significant problems with large wounds. The patients should be assessed for signs of volume depletion such as excessive thirst, diminished skin turgor, and or low urine output. Keeping the wounds covered and moist reduces evaporative water loss and may reduce protein loss as well. Wound infection the earliest and most frequent sign of wound infection is excessive wound pain and tenderness. Low grade fever, wound redness, and drainage often appear later and can be easily seen with a good exam and dressing change. Wounds should be opened in the affected area to allow drainage, irrigation, and gentle packing just like in open wounds. Wound culture and antibiotics are totally unnecessary except in rare circumstances such as when patients exhibit signs of systemic illness and/or there is prosthetic material in the wound. When dealing with abdominal wall wounds, drainage may indicate deep wound problems such as fascial failure and/or evisceration. Gastrointestinal Tract There is a widely held misconception that the gastrointestinal tract in quiescent following illness, injury, and/or surgery. The gut plays an active role in overall host defenses, gastrointestinal stress ulceration, and systemic inflammation. This practice is outdated and not consistent with what is currently known about bowel function in illness. The stomach and small bowel function very well following illness, injury, and /or operative intervention unless there has been mesenteric ischemia or long standing obstruction.
The serum albumin concen tration decreases early in the course of a critical illness and does not increase again until the recovery phase of the illness treatment mrsa buy 5 mg oxybutynin with visa. In the develop ing countries the predictors of stomal complications such as anemia medicine 6 year order 5 mg oxybutynin fast delivery, serum albumin and indicators of sepsis have not been specifically studied and these could be the strong variables associated with poor outcome due to their high prevalence levels in these countries [24] medicine 66 296 white round pill purchase cheapest oxybutynin. Results of Study In the recent study on predictors of stomal complications (ileostomy symptoms ear infection buy discount oxybutynin 5mg on line, colostomy) in a tertiary centre of North India medications gerd discount 5 mg oxybutynin otc, three factors emerged to be the most important predictors of major complications (unpublished data) medicine wheel buy oxybutynin 5 mg overnight delivery. In short though considered to be a relatively simple surgery, creation and care of hassle free stoma is a surgical challenge and many factors dictate the successful outcome of this surgery. Many of the complications of early pregnancy Pregnancy-related Miscarriage (Chapters 2 and 13), present with some form of abdominal pain. There ectopic pregnancy (Chapter 12), are several causes of abdominal pain during early uterine rupture (rare), pain associated pregnancy, some being directly related to preg with uterine growth nancy while others are unrelated medical or surgi Non-pregnancy cal conditions. Table 1 gives an overview of possible related differential diagnoses of lower abdominal pain in Gynecological Ovarian cyst accident and ovarian early pregnancy. Specific pregnancy-related com torsion (Chapters 5 and 11), acute plications are commonly limited to a certain gesta urinary retention, pelvic infection (Chapter 17), complications of tional age. The diag disease, colitis ulcerosa, irritable nosis and management of medical and surgical bowel syndrome causes of lower abdominal pain in pregnancy is Surgical Appendicitis, gastroenteritis, ureteric beyond the scope of this chapter. Most gyneco calculus, intestinal obstruction/ logical causes are described in the respective volvulus chapters as indicated in Table 1. Common causes of lower abdominal pain in the Many patients presenting with lower abdominal first trimester include ectopic pregnancy, abortion/ pain in clinics are not aware of their pregnancy or miscarriage, ovarian cyst accidents. Table 2 summarizes the signs and symptoms consider pregnancy in any of your patients with of the most common differential diagnoses for lower abdominal pain who are of reproductive age lower abdominal pain in the first trimester. In order to make this diagnosis you must keep in mind that a pregnancy might exist, Chapter 1 describes how to take a gynecological even if the patient is not aware of it. If ruptured, signs of shock may be present which include increased pulse/heart rate, increased respiration rate, hypotension, sweating, cold extremities and pallor. Patient may give history of amenorrhea corresponding to between 6 and 10 weeks of gestation. Paracentesis will reveal blood in the abdomen Abortion/miscarriage Cramping abdominal pain confined to the suprapubic area with or without vaginal bleeding. In more severe forms such as incomplete abortion or septic abortion, the patient will present with severe lower abdominal pain, intense vaginal bleeding, sometimes with high fever and shock (fast weak pulse, sweating, hypotension, fast breathing, possibly with altered mental status). Bowel sounds may be reduced, with abdominal distention/rigidity and rebound tenderness. Uterus may be palpable suprapubically On pelvic examination, there may be obvious vaginal bleeding with or without products of conception protruding in the vagina or cervical os. In inevitable and incomplete abortion cervix will be open with products of conception protruding through the cervix. If a proper history is taken and a thorough examination is done, the diagnosis of abortion may be achieved in most cases Ovarian cyst accident Unilateral dull pain, may be associated with bloating, constipation. Cyst rupture or torsion may lead to peritonism with guarding and rebound tenderness and increasingly sharp pain Acute urinary retention Suprapubic pain, often sharp, urge to urinate, suprapubic distention, retroverted uterus in late first trimester. As a consequence the cervix is positioned very cranially and anteriorly in the vagina and might even not be reachable Appendicitis Nausea, vomiting, diarrhea or obstipation, peritoneal signs, point of maximum tenderness moves upwards and laterally in late first trimester and bimanual examination. In a ruptured crampy in early stages but with time it becomes ectopic pregnancy with severe blood loss, patient sharp and stabbing. Recent studies have shown appendicitis, ectopic pregnancy, torsion of that one-third of patients with unruptured ectopic ovarian tumor. In typical ruptured cases, a ness is an indication of appendicitis, ectopic woman will present with pallor, tachycardia, low pregnancy or torsion of ovarian tumor. Bimanual examina may reveal products of conception in the vagina tion (which has to be done cautiously to avoid or at the cervical os found in incomplete abor provoking bleeding) reveals positive cervical tion. It may reveal frank blood in ectopic preg excitation test in about three-quarters of the nancy. See explain the minimal required treatment for the Chapter 12 for more details on management. Abortion/miscarriage Ectopic pregnancy Abortion is one of the most common causes of Ectopic pregnancy remains one of the common lower abdominal pain in early pregnancy and it causes of maternal deaths especially in low-resource should be considered as a differential diagnosis countries. The incidence has been increasing when a woman of a reproductive age presents with steadily in the past four decades due to increased lower abdominal pain. Ectopic pregnancy should be con the pain associated with abortion/miscarriage is sidered in a woman with lower abdominal pain usually cramping in nature confined to the supra with or without vaginal bleeding, especially within pubic area. In more severe forms of the cases ovarian cysts occurring in the first trimester disease such as incomplete or septic abortion, the regress with time as pregnancy advances. Uterus serous cystadenoma, ovarian mucinous cystad may be palpable suprapubically. On pelvic examination, there may be obvious Symptoms that tend to accompany ovarian cysts vaginal bleeding with or without products of con in pregnancy are pain during sexual intercourse or ception protruding in the vagina or cervical os. In during defecation, or pain in the abdomen that may septic abortion, there may be a foul-smelling dis radiate to the thighs and buttocks. Depending on the stage of the abortion, the ovarian cysts may be complicated by rupturing or cervix may be open or closed. If the Torsion of the ovarian cyst is the total or partial abortion is complete, the cervix may either be rotation of the cyst around its axis or pedicle5. In most hence higher chances of torsion, and the size of the cases, the uterus will be enlarged and soft. When torsion occurs, there is vessel blockage, proper history is taken and a thorough examination hence, stasis, congestion, hypoxia, necrosis and is done, the diagnosis of abortion will be achieved hemorrhage. The risk of ovarian torsion rises by five In severe conditions where the patient presents fold during pregnancy making the incidence of 5 with severe bleeding and signs of shock, she should cases per 10, 000 pregnancies5. In inevitable, incomplete, missed abortion, displaced in the anterior and cranial position, and uterine evacuation is done for complete removal of you may even not be able to palpate the cervix. Details on the manage is a rare but serious complication in pregnancy and, ment of abortion are provided in Chapter 13. Round ligament pain in a normal uterine Cases Journal 2009; 2:9405 pregnancy Many pregnant women experience some pain dur ing pregnancy due to the fact that the growing uterus puts traction on bands and ligaments. This is not a serious condition that needs treatment, but all serious complications (see Table 1) should be excluded. E-AvrA strain led to salmonellosis causes symptoms such as abdominal enhanced bacterial invasion, both in vitro and in pain, diarrhea, nausea, vomiting, fever and vivo. Taken together, our data reveal a novel role 1 Copyright 2016 by the American Society for Biochemistry and Molecular Biology, Inc. Enteritidis is also increasingly activation domain, and this signaling pathway reported in cases of invasive and extra-intestinal generally contributes to inflammatory responses infections, such as septicemia, arthritis, (34). However, the role of the major serotype, Salmonella Enteritidis, is poorly bacterial effector AvrA in Salmonella Enteritidis understood. The AvrA a plasmid-mediated complemented strain in protein in Salmonella Typhimurium is an anti Salmonella Enteritidis. E-AvrA mutant and restored in the + the intestinal epithelium is formed by a complemented strain S. Our Western blot data component of intercellular junctional complexes showed that the AvrA protein was absent in the formed by integral membrane proteins such as mutant strain (S. E-AvrA) and over-expressed in + occludin, claudin family members and junctional the complemented strain (S. The cytoplasmic Ponceau S staining indicated even protein loading domain of occludin and claudins binds to in each lane. The mutant and complemented solute and water flow through the paracellular strains were characterized biochemically using the space, and inhibit bacterial invasion (29). E-AvrA infection compared epithelial cells upon infection by Salmonella + to wild type S. There was no change in the results in enhanced invasion of epithelial cells by adhesion junction protein E-cadherin with or Salmonella Enteritidis. In the current study, we report that the Next, we investigated bacterial invasion in Salmonella Enteritidis effector protein AvrA the mouse colon. E-AvrA colonized colon tissue than in wild type + signaling pathway, which was demonstrated in S. Enteritidis-infected increases cell permeability, reduces bacteria mice, using Luminex assays. E-AvrA infected mice + are the first to report that the Salmonella compared to wild type S. There are numerous serotypes of Salmonella; different serotypes are increased in S. Our results indicate that Salmonella Enteritidis AvrA found in different animal hosts or environments, decreases bacterial invasion and reduces and they may cause different symptoms in inflammation. Typhimurium, including delayed pathological Our previous study showed that AvrA of S. Bacterial effector proteins the adherens junction protein E-cadherin was paralyze or reprogram eukaryotic cells to benefit decreased in the colon of mice treated with wild pathogens. Protein the AvrA deletion mutant was constructed levels were determined by Western blotting. The primers used in Water and food were withdrawn 4 hours this study are listed in Table 2. All bands detected on blots Mouse epithelial cells were scraped and lysed were consistent with production information from in lysis buffer (1% Triton X-100, 150 mM NaCl, the companies and other scientific reports which 10 mM Tris pH 7. Each analysis was 1 to 10 goblet cells/high-power field; and 3, <1 performed in triplicate for each tissue section on a goblet cell/high-power field. Epithelial integrity was scored as follows: 0, no detectable pathological changes in Quantitative pathological analysis 10 high-power fields (400x magnification); 1, Segments of the cecum and colon were fixed epithelial desquamation; 2, erosion of the and embedded in paraffin according to standard epithelial surface (gaps of 1 to 10 epithelial procedures. Cryosections (5 m) were mounted on cells/lesion); and 3, epithelial ulceration (gaps of glass slides, air dried for 2 hours at room 10 epithelial cells/lesion; at this stage, there is temperature, and stained with hematoxylin and generally granulation tissue below the epithelium). Pathological evaluations were We averaged the two independent scores for performed by two pathologists in a blinded manner. The scheme for quantitative pathological analysis of combined pathological score for each tissue cecal inflammation in H&E-stained sections (5 m) sample was determined as the sum of these was followed. The combined pathological score Submucosal edema was scored as follows: 0, no ranged between 0 and 13 arbitrary units and pathological changes; 1, mild edema (submucosa: covered the following levels of inflammation: 0, 0. All expression levels were treatment group differences among the wild type, + normalized to actin levels in the same sample. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 50, 882-889 3. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 43, 512-517 4. Journal of the American Society of Echocardiography: official publication of the American Society of Echocardiography 22, e1-3 9. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 46, 963-969 10. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 49, 606-611 13. Proceedings of the National Academy of Sciences of the United States of America 97, 6640-6645 51. Proceedings of the National Academy of Sciences of the United States of America 109, 14007-14012 56. Bacterial strains and plasmids used in this study Strains/Plasmids Characteristics References Strains S. Construction of the AvrA deletion mutant and complemented strains from Salmonella Enteritidis strain C50336. Epithelial cells were colonized with Salmonella Enteritidis wild type, AvrA mutant or AvrA complemented strains. E-AvrA or wild type strain were significant for follow-up measurements at 1-8 hours. Enteritidis AvrA deletion mutant leads to a more severe inflammatory response in the mouse cecum. The semi-quantitative inflammatory scores for murine cecal mucosa from H&E staining of sections at 8 hours (B) and 4 days (C) post-infection encompassed individual scores for edema, polymorphonuclear cell infiltration, decreased goblet cell number, and epithelial layer integrity, as described in the Materials and Methods.