Adam Helms, MD
- Chief Medical Resident, Department of Internal Medicine, University of
- Virginia, Charlottesville, VA, USA
Environmental factors have been suggested as triggers for the autoimmune response acne 26 year old female order cheap decadron on line. These suggested factors include viral infec tions acne zeno buy decadron on line, infant feeding practices acne medication order decadron on line, toxins such as N-nitroso derivates skin care manufacturers purchase 8mg decadron otc, vaccinations skin care center cheap decadron 1 mg online, and arsenic exposure acne 70 off decadron 8 mg free shipping, but for the most part evidence supporting these links is lacking. Patients present with respiratory insufficiency due to alveolar haemorrhage, rapidly progressive renal insufficiency, or both. Early diagnosis is mandatory in order to prevent end-stage renal disease or death. The incidence is 1–2 cases per 100 000 per year, with higher rates in males and at older ages (Bogliun & Beghi, 2004; Cuadrado et al. Patients present with rapidly progressive tingling, numbness, muscle weakness, and sometimes pain. About one to three weeks after infection, patients exhibit a progressive paralysis for up to four weeks that reaches a plateau phase. In most patients, recovery is complete or near complete within a period of several months. Diagnostic criteria include progressive weakness of more than two limbs, areflexia, and pro gression for no more than four weeks. Neurophysiological testing may further confirm the presence of a peripheral neuropathy. This is also consistent with the rate of recovery being accelerated by plasma exchange or intravenous immunoglobulin. The antidepressant drug zimeldine was also transiently with drawn because of an association with Guillain-Barré syndrome (see section 8. Autoimmune haemolytic anaemia is a rare disorder; the esti mated incidence, based on studies conducted in the 1960s, is 1–3 cases per 100 000 per year (Gehrs & Friedberg, 2002). Two criteria must be met to diagnose autoimmune haemolytic anaemia: serologi cal evidence of an autoantibody, and clinical or laboratory evidence of haemolysis. These diseases are characterized by a positive direct antiglobulin (Coombs’) test and divided into warm and cold auto immune haemolytic anaemias according to whether the antibody reacts more strongly with red cells at 37 °C or at 4 °C. Furthermore, several drugs may cause so-called drug-induced autoimmune haemo lytic anaemia. Distinction of these three mechanisms can be made on the basis of serological reactions of the serum and the eluate. Warm autoantibodies are responsible for 48–70% of autoimmune haemolytic anaemia cases and may occur at any age; due to the secondary causes, however, the incidence increases starting around 40 years of age. There is an approximate 2:1 female predilection, possibly due to the association with other autoimmune diseases. Warm autoimmune haemolytic anaemia presents as a haemolytic anaemia of varying severity. Red cells are typically coated with IgG and/or complement, as detected in the direct antiglobulin test, and eliminated by cells of the reticuloendothelial system. Further more, red cells may become spherical and are ultimately destroyed in the spleen. Infants born to mothers with autoimmune haemolytic anaemia may also suffer transient haemolysis due to passively acquired maternal autoantibodies. The symptoms of autoimmune haemolytic anaemia may precede the recognition of the underlying illness in the case of secondary autoimmune haemolytic anaemia. Cold autoimmune haemolytic anaemia represents about 16–32% of autoimmune haemolytic anaemia cases. Primary cold autoimmune haemolytic anaemia affects primarily older adults, with a slight female preponderance. Patients with primary disease or disease secondary to a lympho proliferative disorder commonly have a mild, chronic haemolytic anaemia, resulting in pallor and fatigue. Obviously, a cold environ ment may exacerbate the condition; especially in the extremities, acrocyanosis due to agglutination of red cells may be observed in the small vessels. Symptoms due to autoimmune haemolytic anaemia secondary to infection are similar, but transient, and appear two to three weeks after the infection starts. Red cells are typically coated with IgM and/or complement, as detected in the direct antiglobulin test. The cold autoantibodies in idiopathic autoimmune haemolytic anaemia and secondary to a lymphoproliferative disorder are IgM monoclonal antibodies mostly directed against the I-antigen of the Ii blood group system, while antibodies in autoimmune haemolytic anaemia secondary to infections are polyclonal IgM, directed to the I-antigen in the case of Mycoplasma pneumoniae and to the i antigen in the case of infectious mononucleosis. IgM-sensitized red blood cells are generally associated with a combination of intra and extravascular haemolysis, the latter being more common. Intra vascular haemolysis occurs because IgM antibodies readily activate 58 Clinical Expression of Human Autoimmune Diseases the classical complement pathway. Kupffer cells in the liver are the principal effectors of IgM-associated extravascular haemolysis. Drug-induced immune haemolytic anaemia secondary to neoantigen formation or drug absorption has a positive direct antiglobulin test and can be serologically distin guished from true autoimmune haemolytic anaemia because of the requirement for an exogenous drug to detect the antibody. The incidence of all these types of drug-induced immune haemolytic anaemia clearly varies with changes in drug usage in clinical practice. Typically, the haemolytic anaemia gradually disappears when the drug is discontinued, but with true autoimmune haemolytic anaemia, the autoantibodies may persist for several months. It is divided into three types, according to the autoantibody profile, but only two types have mutually exclusive autoantibodies and different clinical profiles (Ben-Ari & Czaja, 2001). Anti-soluble liver antigen antibodies were originally considered typical for type 3 autoimmune hepatitis. Since clinical and laboratory features of patients with anti-soluble liver antigen antibodies are indistinguishable from those of patients with type 1 autoimmune hepatitis, the presence of these antibodies is probably not a hallmark of a separate entity. There are limited data concern ing disease rates, but a recent study from Norway estimated an incidence of autoimmune hepatitis of approximately 2 cases per 100 000 per year and a prevalence of 15 per 100 000 (Boberg et al. Typical symptoms of disease result from liver dysfunction and include fatigue, jaundice, dark urine, anorexia, and abdominal discomfort. A definite diagnosis requires exclusion of viral, drug-induced, alcoholic, and hereditary liver disease. The mechanism by which hepatocytes are destroyed in autoimmune hepatitis has not been unravelled, but both T cell mediated and antibody-dependent cellular cytotoxicity mechanisms have been postulated (Vergani & Mieli-Vergani, 2003). However, this type of autoimmune hepatitis is a distinct clinical entity, different from idiopathic autoimmune hepatitis. Although by definition autoimmune hepatitis is a non-viral disease, there is a clear association between viral infection and the autoimmune response. In particular, autoantibodies associated with autoimmune hepatitis commonly occur in chronic hepatitis B and C infection. Several drugs and chemicals or their metabolites have been shown to induce hepatitis with autoimmune involvement. Halothane is a general anaesthetic agent that has been associated with hepatitis (Neuberger, 1998). Hepatitis is the result of toxic metabolites that are generated by cytochrome P450-mediated drug metabolism and bind covalently to liver components. Additionally, covalent binding of toxic metabolites to cytochrome P450 can lead to the formation of neoantigens and subsequently of anticytochrome P450 antibodies, resulting in immune-mediated hepatitis associated with dihydrala zine, tienilic acid, and iproniazid. Since the antigens are ill defined in terms of being endogenous or exogenous antigens, it remains questionable whether the inflammatory bowel diseases are bona fide autoimmune dis orders. However, the occurrence of autoantibodies in these diseases warrants further description of the two most common, but distinct, forms of inflammatory bowel disease: Crohn disease and ulcerative colitis. The illness characteristically waxes and wanes and eventually may lead to serious intestinal complications, such as strictures, perforation, and fistulae (Podolsky, 2002). The clinical manifestations of Crohn disease are the results of transmural inflammation of the bowel wall. Any part of the alimentary tract may be involved, although most typically the terminal ileum, colon, and small intestine are affected. The disease is associated with arthritis, uveitis, and sclerosing cholangitis, as well as features of malabsorption. Histopathology reveals granulo matous lesions, associated with crypt abscesses, fissures, and aphthous ulcers with submucosal extensions. The diagnosis of Crohn disease is based on the finding of typical clinical and pathological features and absence of evidence of other mimicking conditions. Factors involved in the pathogenesis of Crohn disease include genes, the mucosal immune system, and the microbial environment in the gut. The gene product is involved in signal transduction upon binding of bacterial lipopolysaccharide. Ulcerative colitis, in contrast to Crohn disease, is limited to the colon and involves mainly the superficial layers of the bowel. Patients typically present with diarrhoea, tenesmus, relapsing rectal bleeding, and lower abdominal cramps and pain with defecation. Ulcerative colitis may present in a very severe form, with transmural damage to the colon, which has a high risk of perforation and death. Extra intestinal manifestations include arthritis, uveitis, pyoderma gangrenosum, erythema nodosum, and sclerosing cholangitis. The superficial mucosal inflammation and ulceration of the rectal and colonic mucosa occur in a continuous pattern, typically decreasing in severity in more proximal areas of the colon. The mucosa has intense infiltration of the colonic crypts with polymorphonuclear cells and surrounding accumulations of lymphocytes and plasma cells. The diagnosis of ulcerative colitis is based on exclusion of infections and subsequent visualization of the rectal and colonic mucosa by flexible 62 Clinical Expression of Human Autoimmune Diseases sigmoidoscopy and biopsy and either total colonoscopy or double contrast barium enema examination. Environmental factors, in particular factors that trigger detrimental mucosal immune responses to enteric bacteria, are considered more important than genetic factors in the pathogenesis of ulcerative colitis (Farrell & Peppercorn, 2002). Of all environmental factors, the protective effect of cigarette smoking remains the most con sistent. Nicotine is probably the main active ingredient in this association, but the mechanisms remain unknown. In patients with long-standing disease, there is an increased risk of colonic dysplasia and adenocarcinoma. The prevalence of the disease is approximately 60 cases per 100 000, and the incidence is 3 cases per 100 000 per year (Jacobson et al. The most apparent clinical presentation of multiple sclerosis includes chronic or relapsing paralysis and problems of vision, sensation, strength, and coordination. Several disease patterns can be distinguished: relapsing-remitting (60–70%), primary progressive (10–20%), and secondary progressive multiple sclerosis (15–25%), all resulting in the accumulation of significant neurological disability (Compston & Coles, 2002). Multiple sclerosis is diagnosed based on the objective demonstration of dissemination of lesions in both time and space, and diagnosis incorporates evidence from magnetic resonance imaging (McDonald et al. Further analysis of the demyelinating lesions may reveal, besides a T cell and macrophage-dominated immune response, immunoglobulin and complement deposition, myelin protein loss, and distinct patterns of oligodendrocyte degeneration. On the basis of these findings, four patterns of demyelination have been identified, suggesting that there exist distinct pathogenetic mechanisms (Kornek & Lassmann, 2003). The primary injury is directed at the myelin itself or its cell of origin, the oligodendrocyte, being responsible for synthesis and maintenance of the myelin sheath of nerve axons. The main concept holds activated auto reactive T cells responsible for driving chronic inflammation and macrophage/microglia activation in the lesions. The presence of antibodies against myelin proteins may add to the immunopathogenetic mechanism. The estimated prevalence of disease varies between 5 and 15 cases per 100 000 (Jacobson et al. There are two peak disease incidences with different male/female ratios: before age 40, women are 3 times more commonly affected, whereas in the older age group, males predominate. The prominent clinical feature of myasthenia gravis is painless, fatigable weakness of selected muscle groups. Anti-acetylcholine receptor antibodies are present in about 85–90% of patients and, when identified in the appropriate clinical setting, are diagnostic for myasthenia gravis. Furthermore, a similar syndrome, Lambert-Eaton syndrome, is associated with antibodies against the presynaptic, voltage-gated calcium channels. Rever sibility of clinical symptoms with anticholinesterase inhibitors in myasthenia gravis is another hallmark of diagnosis. Once a diagnosis has been made, computed tomography or magnetic resonance imaging of the chest should be done to exclude an associated thymoma, which is apparent in about 10% of the patients. Myas thenia gravis is a prototypic autoimmune disease, since its antibody mediated pathogenesis is exclusively directed to the postsynaptic membrane of the neuromuscular junction. Antibodies directed to the acetylcholine receptor lower the number of functional receptors, leading to an impaired neuromuscular signal transduction, resulting in the characteristic fatigable skeletal muscle weakness. Indeed, in muscle biopsy specimens from myasthenia gravis patients, antibodies are attached to the postsynaptic membrane, receptors are lost, and postsynaptic folds are sparse and shallow. The immunopathogenetic role of the autoantibodies is further established by the occurrence of neonatal myasthenia gravis in babies born to women with the disease. In these cases, spontaneous resolution usually occurs within a few weeks due to disappearance of maternal antibodies. This haplotype has also been involved in other human autoimmune diseases, including systemic lupus erythematosus, coeliac disease, insulin-dependent diabetes mellitus, and autoimmune thyroiditis, suggesting that the respective genes could determine non-antigen specific immune dysregulation rather than specify a particular “self” target to the immune system (Garchon, 2003). This may also explain why myasthenia gravis is often associated with other autoimmune diseases, such as insulin-dependent diabetes mellitus and autoimmune thyroiditis. Clinical features of the disease are unexplained con gestive heart failure, chest pain mimicking myocardial infarction, arrhythmias, syncope, and sudden death. Early and definite diag nosis of myocarditis depends on the detection of inflammatory infil trates in endomyocardial biopsy specimens according to the Dallas criteria. Histopathology reveals lymphocytic infiltrates, interstitial oedema, myocardial necrosis, and fibrosis. These antibodies are directed against a multitude of autoantigens, such as the ȕ1-adreno receptor and Į-myosin, and have only limited sensitivity (Caforio et al. For some of these autoantibodies, there is in vitro evi dence for a functional role.
The Trigger Point Manual skin care 4men wendy best order decadron, Williams & Wilkins acne 6 months after giving birth buy decadron online, Diagnostic Criteria Baltimore acne wash discount decadron online american express, 1983 acneorg safe decadron 8mg. The patient’s pain is aggravated by clinical tests that Definition selectively stress the affected segment acne- buy cheap decadron on-line. Stressing adjacent segments does not reproduce the from an alar ligament as a result of sprain of that liga patient’s pain acne medication accutane proven decadron 8 mg. Presumably involves excessive strain in Upper cervical spinal pain, suboccipital pain, and/or curred during activities of daily living by structures such headache, aggravated by contralateral rotation of the as the ligaments, joints, or intervertebral disk of the af atlas, associated with hypermobility of the atlas in con fected segment. Remarks Diagnostic Criteria this diagnosis is offered as a partial distinction from the patient’s pain must clearly be aggravated by rotation spinal pain of unknown origin, insofar as the source of of the atlas to the side opposite that of the putatively the patient’s pain can at least be narrowed to a particular affected ligament, and hypermobility of the atlas must be offending segment. Presumably the same as for sprains in liga wish to pursue such investigations, or if the pain arises ments of the appendicular skeleton. For this diagnosis to be sustained, the clinical tests used Code should be able to stress selectively the segment in ques 132. X6aR Arm Definition Cervical spinal pain ostensibly due to excessive strains sustained by the restraining elements of a single spinal Traumatic Avulsion of Nerve Roots motion segment. Definition Diagnostic Features Thoracic spinal pain occurring in a patient with a history A presumptive diagnosis can be made on the basis of an of injury, in whom radiography or other imaging studies elevated white cell count or other serological features of demonstrate the presence of a fracture that can reasona infection, together with imaging evidence of the pres bly be interpreted as the cause of the pain. Absolute confirmation relies on Clinical Features histological and/or bacteriological confirmation using Thoracic spinal pain with or without referred pain. Diagnostic Features Schedule of Sites of Infection Radiographic or other imaging evidence of a fracture of X-2. X2bR and/or other features of an infection, in whom the site of infection can be specified and which can reasonably be interpreted as the source of the pain. X4jR Diagnostic Features A presumptive diagnosis may be made on the basis of imaging evidence of a neoplasm that directly or indi rectly affects one or other of the tissues innervated by Thoracic Spinal or Radicular Pain thoracic spinal nerves. Absolute confirmation relies on Attributable to Metabolic Bone obtaining histological evidence by direct or needle bi opsy. X51R Page 114 Thoracic Spinal or Radicular Pain Remarks There is no evidence that congenital anomalies per se Attributable to Arthritis (X-5) cause pain. Although they may be associated with pain, the specificity of this association is unknown. This clas Definition sification should be used only when the cause of pain Thoracic spinal pain associated with arthritis that can cannot be otherwise specified and there is a perceived reasonably be interpreted as the source of the pain. Remarks Clinical Features Osteoarthritis is included in this schedule with some Thoracic spinal pain with or without referred pain, to hesitation because there is only a weak relation between gether with features of the disease affecting the viscus or pain and this condition as diagnosed radiologically. The alternative classification to “thoracic pain due to osteoarthrosis” should be “thoracic zygapophysial joint Diagnostic Features pain” if the criteria for this diagnosis are satisfied (see Imaging or other evidence of the primary disease affect X10), or “thoracic spinal pain of unknown or uncertain ing a thoracic viscus or vessel. Schedule of Diseases Similarly, the condition of “spondylosis” is omitted from X-7. X2 (known infection); between the radiographic presence of this condition and Code 323. X4 bral Anomaly (X-6) Definition Thoracic spinal pain associated with a congenital verte bral anomaly. Thoracic Spinal Pain of Unknown or Uncertain Origin (X-8) Clinical Features Thoracic spinal pain with or without referred pain. Definition Diagnostic Features Thoracic spinal pain occurring in a patient whose clini Imaging evidence of a congenital vertebral anomaly cal features and associated features do not enable the affecting the thoracic vertebral column. Definition As for X-8, but the pain is located in the middle thoracic Diagnostic Features region. Thoracic spinal pain for which no other cause has been found or can be attributed. Diagnostic Criteria As for X-8, save that the pain is located in the midtho Remarks racic region. This definition is intended to cover those complaints that for whatever reason currently defy conventional diagno Pathology sis. It presupposes an organic basis for the pain, but one that cannot be or has not been established reliably by clinical Remarks As for X-8. X8gR Patients given this diagnosis could in due course be ac corded a more definitive diagnosis once appropriate di agnostic techniques are devised or applied. In some instances, a more definitive diagnosis might be attain Lower Thoracic Spinal Pain of Un able using currently available techniques, but for logistic known or Uncertain Origin (X-8. Definition As for X-8, but the pain is located in the upper thoracic Diagnostic Criteria region. Diagnostic Criteria As for X-8, save that the pain is located in the upper Remarks thoracic region. Page 116 Clinical Features lus, or as a result of excessive stresses imposed on the Spinal pain located on the thoracolumbar region. Diagnostic Criteria As for X-8, save that the pain is located in the thora Remarks columbar region. Provocation diskography alone is insufficient to estab lish conclusively a diagnosis of discogenic pain because Pathology of the propensity for false-positive responses, either be As for X-8. X81R Thoracic diskography is particularly hazardous because of the risk of pneumothorax. No publications have for Thoracic Discogenic Pain (X-9) mally described this procedure or experience with it. Until its safety and clinical utility have been established, Definition thoracic diskography should be restricted to centers ca Thoracic spinal pain, with or without referred pain, pable of dealing with potential complications and pre stemming from a thoracic intervertebral disk. X7cS Dysfunctional Diagnostic Criteria the patient’s pain must be shown conclusively to stem from an intervertebral disk by demonstrating Thoracic Zygapophysial Joint Pain either (1) that selective anesthetization of the puta tively symptomatic intervertebral disk com (X-10) pletely relieves the patient of the accustomed pain for a period consonant with the expected Definition duration of action of the local anesthetic used; Thoracic spinal pain, with or without referred pain, or (2) that selective anesthetization of the puta stemming from one or more of the thoracic zyga tively symptomatic intervertebral disk substan pophysial joints. For the be ascribed to some other source innervated by diagnosis to be declared, all of the following criteria the same segments that innervate the putatively must be satisfied. Arthrography must demonstrate that any injection Unknown, but presumably the pain arises as a result of has been made selectively into the target joint, and chemical or mechanical irritation of the nerve endings in any material that is injected into the joint must not the outer anulus fibrosus, initiated by injury to the anu Page 117 spill over into adjacent structures that might other stitutes presumptive evidence that the joint may be wise be the actual source of the patient’s pain. The patient’s pain must be totally relieved following the condition can be firmly diagnosed only by the use the injection of local anesthetic into the target joint. For the diagnosis to be firmly sus tion of local anesthetic is insufficient for the diagno tained, all of the following criteria must be satisfied. The response must be validated by an appropriate control test that excludes false If intraarticular blocks are used, positive responses on the part of the patient, such as: 1. A single positive response to the intraarticular injec into the target joint on separate occasions. The response must be validated by Local anesthetic blockade of the nerves supplying a tar an appropriate control test that excludes false get zygapophysial joint may be used as a screening pro positive responses on the part of the patient, such as: cedure to determine in the first instance whether a. Remarks If periarticular blocks are used, an injection of contrast See also Thoracic Segmental Dysfunction (X-15). X7eS Dysfunctional Definition Thoracic spinal pain, with or without referred pain, stemming from one or more of the costo-transverse joints. Thoracic Muscle Sprain (X-12) Clinical Features Definition Thoracic spinal pain, with or without referred pain, ag Thoracic spinal pain stemming from a lesion in a speci gravated by selectively stressing a costo-transverse joint. Diagnostic Criteria No criteria have been established whereby costotrans Clinical Features verse joint pain can be diagnosed on the basis of the Thoracic spinal pain, with or without referred pain, as patient’s history or by conventional clinical examination. Page 118 Diagnostic Criteria a muscle without a palpable band does not satisfy the the following criteria must all be satisfied. There is a history of activities consistent with the condition are fulfilled, or spinal pain of unknown or un affected muscle having been strained. X7fS Dysfunctional Thoracic Trigger Point Syndrome Thoracic Muscle Spasm (X-14) (X-13) Definition Thoracic spinal pain resulting from sustained or repeated Definition involuntary activity of the thoracic spinal muscles. Thoracic spinal pain stemming from a trigger point or trigger points in one or more of the muscles of the tho Clinical Features racic spine. Thoracic spinal pain for which there is no other underly ing cause, associated with demonstrable sustained mus Clinical Features cle activity. Thoracic spinal pain, with or without referred pain, as sociated with a trigger point in one or more muscles of Diagnostic Features the vertebral column. A trigger point must be present in a muscle, consist vents adequate wash-out of algogenic chemicals pro ing of a palpable, tender, firm, fusiform nodule or duced by the sustained metabolic activity of the muscle. Palpation of the trigger point reproduces the patient’s cle, clinical tests or conventional electromyography have pain and/or referred pain. Elimination of the trigger point relieves the patient’s sustained muscle activity in such situations. Trigger points are believed to represent areas of contracted muscle that have failed to relax as a result Code of failure of calcium ions to sequestrate. Presumably involves excessive strain im paraspinal muscle spasm during sleep in patients with low posed by activities of daily living on structures such as back pain, Clin. X7dS/C Dysfunctional Thoracic spinal pain, with or without referred pain, that can be aggravated by selectively stressing a particular spinal segment. Radicular Pain Attributable to a Pro Diagnostic Criteria lapsed Thoracic Disk (X-16) All the following criteria should be satisfied. Progressive aching, burning pain with paresthesias and sensory and motor impairment in the distribution of a Social and Physical Disability branch or branches of the brachial plexus due to tumor. The tumors are associated with slowly progressive pain and paresthesias, and subsequently severe sensory loss System and motor loss. Burning pain of increasing severity referred to the peripheral nerves occurs frequently in lymphoma, leu upper extremity. Pain Quality: the Includes all those lesions above, the scalenus anticus pain tends to be constant, gradual in onset, aching, and syndrome, and abnormalities of the first thoracic rib or burning, and associated with paresthesias in the distribu the presence of a cervical rib. There is associated sensory loss and muscle wasting depending upon the area of the brachial plexus involved. Pain relief Chemical Irritation of the Brachial is often not adequate, even with significant narcotics. Signs are loss of reflexes, sensation, and muscle severe paroxysms, in the distribution of the brachial strength in the distribution of the involved portion of the plexus or one of its branches, with sensory-motion defi plexus. The diagnosis is usu cits due to effects of local injection of chemical irritants. Electromy ographic studies validate the location of the lesion, Page 122 Site Traumatic Avulsion of the Brachial Upper limb. Definition Pain, most often burning or crushing with super-added Main Features paroxysms, following avulsion lesions of the brachial Prevalence: injections in the shoulder area with any plexus. Site Incidence: the pain begins almost immediately with the Felt almost invariably in the forearm and hand irrespec injection and is continuous. Occasionally, in avulsion of C5 burning in character, superficial, and unaffected by ac root only, pain may be felt in shoulder. It frequently persists even after neurological loss has resolved and is System not necessarily associated with paresthesias or sensory Nerve roots torn from the spinal cord. There are no differences between noxious agents as to time pattern, occurrence, character, intensity, or dura Main Features tion. Prevalence: some 90% of the patients with avulsion of one or more nerve roots suffer pain at some time. Virtu Signs and Laboratory Findings ally all patients with avulsion of all five roots suffer se the signs are of brachial plexus injury. Age of Onset: vast loss, and paresthesias occur in the appropriate area de majority of patients with this lesion are young men be pending upon the portion of the plexus injured. There tween the ages of 18 and 25 suffering from motorcycle are no specific laboratory findings. The older the patient the more likely he is to suffer pain from the avulsion lesions. Pain Quality: the Usual Course pain is characteristically described as burning or crush Pain is generally acute with the injection and gradually ing, as if the hand were being crushed in a vise or were improves. The pain is constant and is a permanent back that persist continue unabated permanently. These paroxysms stop the patient in his tracks and may cause him to cry out and grip his arm Pathology and turn away. Time Pattern: frequency varies between the pathology is a combination of intraneural and extra a few an hour, a few a day, or a few a week. There is no set pattern to the paroxysms, Summary of Essential Features and the patient has no warning of their arrival. The diagnosis stant pain may also be described as severe pins and nee can only be made by history of injection. In some patients there is a gradual increase in Diagnostic Criteria the intensity of the pain over a period of days, building 1. Burning pain with occasional superimposed parox then gradually subsiding over the next few days. Associated Symptoms Differential Diagnosis Aggravating factors: cold weather, extremes of tempera this includes all of the muscular and bony compres ture, emotional stress, and intercurrent illness all aggra sions, anomalies, and tumors previously described. The pain is almost invariably relieved by distraction involving absorbing work or hobbies. X5 thetic and paralyzed arm or hit the shoulder Page 123 to try and relieve the pain. Drugs are singularly unhelp sharp, shooting pains that last seconds and vary in fre ful and a full range of analgesics is usually tried, but quency from several times an hour to several times a very few patients respond significantly. So characteristic is the pain of an avulsion lesion probably by relaxing the patient and promoting sleep. A that it is virtually diagnostic of an avulsion of one or number of patients have found that smoking cannabis more roots. Traction lesions of the brachial plexus that can markedly reduce the pain, but if so it interferes with involve the nerve roots distal to the posterior root gan their concentration, and very few indeed are regular can glion are seldom if ever associated with pain. Most patients ask their doc tors about amputation as a means of relieving the pain, Code and it has to be made clear to them the pain is central 203.
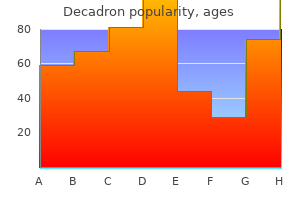
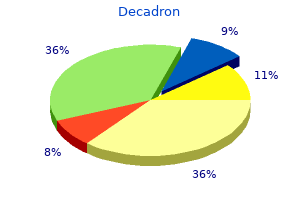
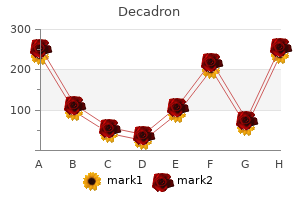
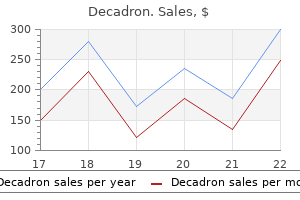
The result is that premium costs are putting healthcare out of reach for employers and individuals acne forum effective 0.5mg decadron. Adding the ability to save on taxes and keep some of the savings achieved by careful consumerism provides even more incentive for consumers to take an active role in controlling healthcare costs acne active buy decadron 4mg online. This can skin care gadgets cheap decadron 1mg line, in turn acne 2007 4mg decadron for sale, lower the average cost of claims through better utilization of healthcare services and help lower your premium costs acne 3 dpo purchase decadron online from canada. At that point acne 60 year old woman order decadron uk, the behavior change that affects utilization patterns and average cost of claims reaches critical mass and employers fnd they have more bargaining power to ask for lower rates from their insurance carriers. Many employers report that they have four primary motivators for adopting the full replacement approach. Their premiums are increasing so quickly, they know they will soon have to start cutting benefts to keep costs low. The sooner they adopt these ways, the more savings they achieve and the more benefts they can preserve for their employees. There is one overriding account holder concern—risk of exposure to high out-of pocket costs. This must be coupled with effective communication and fnancial incentives to build trust among employees. HealthEquity’s clients who have chosen to offer the full-replacement plan option report that a by-product of the approach is increased social networking among employees to comment on the plan and educate each other. On the other hand, client groups that have chosen the opposite approach, offering three or more plan options, report that their employees consistently remain with the same plans. High adoption Full-replacement Medium adoption Dual option Low adoption 3+ options 2. High adoption More than 40 percent diferential Medium adoption 15 percent − 39 percent diferential Low adoption Less than 15 percent diferential 3. High adoption Federally mandated minimum Medium adoption Up to $2,000/$4,000 single/family Low adoption More than $2,000/$4,000 single/family 4. High adoption Equal alternative plan(s) Medium adoption Up to 50 percent higher than alternative plan(s) Low adoption Greater than 51 percent higher than alternative plan(s) Guidelines for employers 149 5. Employees educate each other by discussing ways to build their balances and control costs. High adoption Greater than 60 percent of deductible Medium adoption 25 percent −59 percent of deductible Low adoption Less than 25 percent of deductible 6. Employees may be uncomfortable with this new type of plan, and many will not understand how it works. Employers who provide employees with information and tools to help them make better healthcare decisions, especially decisions on how to use the healthcare system effectively, will see their employees taking full advantage of the opportunity to increase the equity in their accounts and gain every allowable tax beneft. However, it is only necessary to count employees who are eligible individuals and have the same category of coverage (such as self-only or family) (Treas. Part-time employees (customarily those who are employed fewer than 30 hours per week) are tested separately (Treas. Unless it is done through a cafeteria plan, employers may not make matching contributions that are conditional on a contribution by the employee (Treas. For example, through a cafeteria plan, an employer may offer to contribute $500 to your account on the condition that you also contribute to the account. Employers will meet the notice requirement if, by January 15 of the following calendar year, they provide written notice to all affected employees (Treas. Employers must report the contributions in box 12 on Form W-2 for each employee, including amounts the employee contributed through a cafeteria plan (Instructions to Form W-2. Employer contributions are deductible by the employer as contributions to a health plan. Funds the account holder accumulates in an employer-sponsored pension plan are shielded from creditors in the event that the account holder declares personal bankruptcy. If your account is considered dormant for a period of time, the trustee or custodian must forward the amount to the State’s treasury, which will hold it until the account owner claims it back. To prevent this, you will need to make sure your account is active by checking the balance periodically. State and local government employees should look to the agencies charged with administering their beneft plans. States and localities may vary widely on issues of reporting, comparability, eligibility, fduciary obligations and recordkeeping. A trustee is a party given legal responsibility to hold property in the best interest of or for the beneft of another entity or person. A custodian on the other hand, is the person or institution in charge of property in terms of maintenance of an account, but with no investment or management responsibilities. The trustee must deal with the trust property honestly, put the benefciary’s interest above its own and closely follow the terms of the trust. Though it may have discretion over investments and day-to-day management, these functions are still governed by the trust agreement. Federal law overlap with state law A plan that meets federal law may not meet state requirements. These provisions of the law are discussed in order of the year in which they became effective. These exchanges enable people to comparison shop for standardized health packages. The healthcare reform law will facilitate enrollment and administer tax credits, so that people of all incomes can obtain affordable coverage. Starting in 2014, most individuals were required to obtain an acceptable level of health insurance coverage or pay a penalty. The penalty for not having coverage was $95 in 2014, $325 in 2015, $695 or up to 2. However, on December 19, 2017, Congress passed the Tax Cut and Jobs Act of 2017 that abolished the Affordable Care Act’s penalty for not having health insurance in 2019 and beyond. Insurers will no longer be able to exclude coverage for treatments based on pre-existing health conditions. Insurers are also prohibited from charging higher rates due to health status, gender or other factors. Premiums will vary only on age (no more than 3:1), geography, family size and tobacco use. Annual limits on the amount of coverage an individual receives eliminated Elimination of annual limits started with some plans in 2010. In 2014, it applied to all major medical health plans (excluding gap or mini-med plans) without exception. This applies to all clinical trials that treat cancer and other life-threatening diseases. If you have to pay for coverage out-of-pocket while in a clinical trial, you at least reduce some of the costs by paying with tax-free dollars. The Cadillac Tax thresholds are expected to increase by an infation adjustment each year, and adjustments will also be made to increase the thresholds for employers with higher-risk occupations or an older workforce. Some estimates suggest that at current trends, as many as 60 percent of employers will be subject to some Cadillac Tax by 2022 for exceeding the threshold. These funds earn tax-free interest (in most cases) and any potential gains that come from investing the funds are also tax-free. Connecting Health and Wealth 165 Introduction to standard retirement accounts Funding retirement There are many accounts and plans that people can use to save for retirement. Many of these retirement accounts are employer-sponsored plans funded through payroll deductions. Deductions depend on your income level and whether you are covered by a workplace retirement account. You can begin making withdrawals without penalty, paying ordinary income taxes on distributions at age 59½. Withdrawals before age 59½ are subject to a 10% penalty in addition to ordinary income taxes. However, once you begin withdrawing funds from the account, any distributions (including interest or earnings) are tax-free if the distribution comes at least fve years after you established the account and at least one of the following has occurred. A 403(b) is nearly identical to a 401(k) but it is used by non-proft or public institutions such as schools, charities and hospitals. There are other minor differences between these two retirement vehicles, but contribution limits and age requirements are the same for both. Connecting Health and Wealth 167 A 401(k) or 403(b) allows you and/or your employer to contribute a portion of your wages to an account specifcally designed for retirement. Most contributions are made pre-tax, income and growth accumulate tax-deferred and distributions are considered taxable income. In 2018, an employee can contribute up to $18,500 each year to their 401(k) or 403(b) ($24,500 for those 50 and older) depending on their individual circumstances. Employers can also contribute up to $36,500 to an employee’s 401(k) depending on that employee’s individual circumstances. The maximum combined employee and employer contribution to an employee’s 401(k) or 403(b) in 2018 is $55,000. A tax advisor or fnancial planner can help you calculate what your maximum contribution limit is based on your individual circumstances. Contribution limits to a 401(k) or 403(b) for 2019 have not been announced as of the printing of this edition of the Guidebook. You are also subject to required annual minimum distributions based on your age, retirement date and other factors. As stated previously, pre-tax contributions lower your taxable income and other tax obligations. When funds are used to pay for qualifed medical expenses, the distribution of both principal and interest/growth is tax-free. For a list of what is and what is not considered qualifed medical expenses, please see Appendix B. If the funds are used to pay for qualifed medical expenses, you still won’t have to pay taxes on distributions. If the money is used to pay for anything other than a qualifed medical expense, you will have to pay income taxes on the distribution but you won’t have to pay a tax penalty. In short, compound interest is calculated on the initial principal and also the accumulated interest of previous periods (interest earned on interest). Various factors determine how much can be earned with compound interest, but generally, the higher the number of compounding periods, the higher the interest you will earn. And the longer you keep the money in the account, the more powerful the effect of compound interest. If John saves that same amount every year for 30 years but doesn’t invest those dollars to leverage the power of compound interest, John would accumulate $90,000 over a 30-year period. However, if John invests his contributions each year in a diversifed investment portfolio and is able to achieve a 7% rate of return, his savings will have grown to over $303,000. That is $213,000 more than the actual amount he invested over that period of time. Different contribution strategies may work better for you based upon your tax status and individual circumstances, but we recommend that you discuss the hierarchy of funding strategy with your accountant or other tax professional. Automated advice (sometimes called ‘robo-advice’) is a way to manage investments using computer algorithms or other formulas. The algorithms are controlled by software and do not require a human fnancial adviser to manage the client’s account or assets. Lower fees mean you will keep more of your investment earnings while higher fees could dramatically reduce your earnings over time. Consider that funds typically carry underlying fees which should be considered in your evaluation of the overall cost of investing with a given provider. The term is derived from a solid bold line on Form 1040 and 1040A above the line for adjusted gross income. A taxpayer can take deductions above the line and still choose whether to claim the standard deduction or itemize deductions. A health insurance plan’s permission to proceed with a medical or surgical procedure. A bill that the participant receives for the portion of an out-of-network provider’s bill that the insurance plan doesn’t cover. When a participant receives services from a healthcare provider that doesn’t participate in the insurer’s network, the healthcare provider isn’t obligated to accept the insurer’s payment as payment in full, and they can bill the participant for the unpaid amount. The calendar year may be different than the plan year; the latter may be any 12-month period established by an employer or insurer for managing the plan and accounting for beneft payments. An enrollee may need to provide this certifcate to be exempt from limitations on coverage for pre-existing conditions. A condition that lasts indefnitely, or recurs frequently, and can be treated, but not cured. Acronym for the Consolidated Omnibus Budget Reconciliation Act of 1985 that provides for the temporary continuation of group health plan coverage after a qualifying event to certain employees, retirees and family members who are qualifed benefciaries. Employer contributions are considered comparable if the employer makes similar contributions on behalf of all eligible employees with similar coverage during the same period. Coverage under an individual insurance policy when group health plan benefts are lost. The amount of covered expenses that an individual pays for out-of-pocket before payments are made by the health plan. For a health plan: A dependent that a health insurance company covers under an individual’s health plan; not the same as a tax dependent. In most cases, the health insurance company and state law decide who is a qualifed dependent under the health plan. For tax purposes: A person who can be claimed as a dependent on your federal tax return. The sudden onset of a condition or an accidental injury requiring immediate medical or surgical care to avoid permanent disability or death. An employee beneft that covers all or part of the cost for employees to receive counseling, referrals and advice in dealing with stressful life issues.
Arthroscopic versus open shoulder stabilization for recurrent anterior instability: a prospective randomized clinical trial skin care knowledge trusted decadron 1mg. Recurrent post-traumatic anterior shoulder dislocation- open versus arthroscopic repair skin care with hyaluronic acid purchase 0.5mg decadron with amex. Effects of posterior-inferior capsular plications in range of motion in arthroscopic anterior Bankart repair: a prospective randomized clinical study skin care usa decadron 0.5 mg sale. Arthroscopic stabilization of the shoulder: a prospective randomized study of absorbable versus nonabsorbable suture anchors skin care clinique purchase decadron 1mg with amex. A prospective acne los angeles buy decadron 8mg fast delivery, randomized skin care gadgets decadron 8mg free shipping, clinical and radiographic study after arthroscopic Bankart reconstruction using 2 different types of absorbable tacks. Posterior and multidirectional instability of the shoulder: challenges associated with diagnosis and management. A clinical and radiographic comparison of absorbable and non-absorbable suture anchors in open shoulder stabilisation. Comparison of open and arthroscopic stabilization for recurrent shoulder dislocation in patients with a Bankart lesion. Comparison of an arthroscopic and an open procedure for posttraumatic instability of the shoulder: a prospective, randomized multicenter study. Arthroscopic versus open treatment of Bankart lesion of the shoulder: a prospective randomized study. Arthroscopy: the Journal Of Arthroscopic & Related Surgery: Official Publication Of the Arthroscopy Association Of North America And the International Arthroscopy Association. Muscle strength after anterior shoulder stabilization: arthroscopic versus open Bankart repair. Arthroscopic capsulolabroplasty for posteroinferior multidirectional instability of the shoulder. Open and arthroscopic techniques for the treatment of traumatic anterior shoulder instability in Australian rules football players. Arthroscopic versus open repair for traumatic anterior shoulder instability: a meta-analysis. Arthroscopy: the Journal Of Arthroscopic & Related © Copyright 2016 Reed Group, Ltd. Arthroscopic compared with open repairs for recurrent anterior shoulder instability. Inferior capsular shift procedure in athletes with multidirectional instability based on isolated capsular and ligamentous redundancy. Inferior capsular shift operation for multidirectional instability of the shoulder in players of contact sports. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder. Arthroscopic inferior capsular shift for multidirectional instability of the shoulder: a preliminary report. Arthroscopic inferior capsular split and advancement for anterior and inferior shoulder instability: technique and results at 2 to 5-year follow-up. A prospective controlled randomized study of arthroscopic lavage in acute primary anterior dislocation of the shoulder: one-year follow-up. Arthroscopic lavage speeds reduction in effusion in the glenohumeral joint after primary anterior shoulder dislocation: a controlled randomized ultrasound study. Arthroscopic lavage compared with nonoperative treatment for traumatic primary anterior shoulder dislocation: a 2-year follow-up of a prospective randomized study. Absorbable versus nonabsorbable sutures for the arthroscopic treatment of anterior shoulder instability in athletes: a prospective randomized study. Early results of Bankart repair with a patient controlled rehabilitation program. Accelerated rehabilitation after arthroscopic Bankart repair for selected cases: a prospective randomized clinical study. Arthroscopic repair of combined Bankart and superior labral detachment anterior and posterior lesions: technique and preliminary results. Nonoperative treatment of superior labrum anterior posterior tears: improvements in pain, function, and quality of life. Superior labral lesions anterior to posterior-evaluation and arthroscopic management. Biceps load test: a clinical test for superior labrum anterior and posterior lesions in shoulders with recurrent anterior dislocations. American Journal Of Physical Medicine & Rehabilitation / Association Of Academic Physiatrists. Arthroscopic fixation of superior labral lesions using a biodegradable implant: a preliminary report. Prevalence and variance of shoulder injuries in elite collegiate football players. Evaluation of the acromioclavicular joint following first and second degree sprains. Prevalence of concomitant intraarticular lesions in patients treated operatively for high-grade acromioclavicular joint separations. Comprehensive functional analysis of shoulders following complete acromioclavicular separation. Treatment of distal clavicle fracture and acromioclavicular joint dislocation with closed reduction and pinning. Repair of complete acromioclavicular separations using the acromioclavicular-hook plate. Migration of a threaded steinmann pin from an acromioclavicular joint into the spinal canal. Failure of acromioclavicular reconstruction using Gore-Tex graft due to aseptic foreign-body reaction and clavicle osteolysis: a case report. Salvage of failed acromioclavicular joint reconstruction using autogenous semitendinosus tendon from the knee. Coracoclavicular ligament reconstruction using a semitendinosus graft for failed acromioclavicular separation surgery. Distal clavicle tunnel widening after coracoclavicular ligament reconstruction with semitendinous tendon: a case report. Biomechanics and comparison of two operative methods of treatment of complete acromioclavicular separation. Acute acromioclavicular dislocations treated by fixation of the joint and ligament repair or reconstruction. Treatment of acromioclavicular injuries, especially complete acromioclavicular separation. Vandekerckhove B, van Meirhaeghe J, van Steenkiste M, de Groote W, Verbeke R, Vertongen P. Effect of chondroitin sulphate in symptomatic knee osteoarthritis: a multicentre, randomised, double-blind, placebo-controlled study. Intermittent treatment of knee osteoarthritis with oral chondroitin sulfate: a one-year, randomized, double-blind, multicenter study versus placebo. Glucosamine, chondroitin sulfate, and the two in combination for painful knee osteoarthritis. Chondroitins 4 and 6 sulfate in osteoarthritis of the knee: a randomized, controlled trial. Randomised, double-blind, parallel, placebo-controlled atudy of oral glucosamine, methylsulfonylmethane and their combination in osteoarthritis. Glucosamine sulfate use and delay of progression of knee osteoarthritis: a 3-year, randomized, placebo-controlled, double-blind study. Long-term effects of glucosamine sulphate on osteoarthritis progression: a randomised, placebo-controlled clinical trial. Clinical effectiveness and dose response of image-guided intra articular corticosteroid injection for hip osteoarthritis. Safety and efficacy of ultrasound-guided intra articular hylan G-F 20 injection in osteoarthritis of the hip: a pilot study. Comparison of the efficacy of lower and higher molecular weight viscosupplementation in the treatment of hip osteoarthritis. What is the evidence for viscosupplementation in the treatment of patients with hip osteoarthritis? Treatment of persistent shoulder pain with sodium hyaluronate: a randomized, controlled trial. Intra-articular treatment of hip osteoarthritis: a randomized trial of hyaluronic acid, corticosteroid, and isotonic saline. The symptomatic effects of intra-articular administration of hylan G-F 20 on osteoarthritis of the hip: clinical data of 6 months follow-up. Repeated ultrasound-guided intra-articular injections of 40 mg of Hyalgan may be useful in symptomatic relief of hip osteoarthritis. Hip osteoarthritis: short-term efficacy and safety of viscosupplementation by hylan G-F 20. Clinical evaluation of sodium hyaluronate for the treatment of patients with rotator cuff tear. Accuracy and outcome of sonographically guided intra-articular sodium hyaluronate injections in patients with osteoarthritis of the hip. Variation of the arthroscopic Mumford procedure for resecting the distal clavicle. The treatment of complete dislocation of the outer end of the clavicle: an hitherto undescribed operation. Arthroscopic resection of the outer end of the clavicle from a superior approach: a critical, quantitative, radiographic assessment of bone removal. Arthroscopic distal clavicle resection in athletes: a prospective comparison of the direct and indirect approach. A prospective functional outcome study of shoulder arthroplasty for osteoarthritis with an intact rotator cuff. Total shoulder arthroplasty: Some considerations related to glenoid surface contact. Clinical experience with total arthroplasty and hemiarthroplasty of the shoulder using the Neer prosthesis. A comparison of hemiarthroplasty and total shoulder arthroplasty in the treatment of primary glenohumeral osteoarthritis: results of a multicenter study. Total shoulder replacement compared with humeral head replacement for the treatment of primary glenohumeral osteoarthritis: a systematic review. Early effectiveness of shoulder arthroplasty for patients who have primary glenohumeral degenerative joint disease. Functional outcome after shoulder arthroplasty for primary osteoarthritis: a multicenter study. Shoulder arthroplasty with or without resurfacing of the glenoid in patients who have osteoarthritis. Cemented polyethylene versus uncemented metal-backed glenoid components in total shoulder arthroplasty: a prospective, double-blind, randomized study. Effect of humeral head component size on hemiarthroplasty translations and rotations. Humeral resurfacing hemiarthroplasty with meniscal allograft in a young patient with glenohumeral osteoarthritis. Biologic resurfacing of the arthritic glenohumeral joint: Historical review and current applications. The effect of articular conformity and the size of the humeral head component on laxity and motion after glenohumeral arthroplasty. Geometrical analysis of Copeland surface replacement shoulder arthroplasty in relation to normal anatomy. Copeland surface replacement arthroplasty of the shoulder in rheumatoid arthritis. Arthroscopic glenoid resurfacing as a surgical treatment for glenohumeral arthritis in the young patient: midterm results. Outcome after cup hemiarthroplasty in the rheumatoid shoulder: a retrospective evaluation of 39 patients followed for 2-6 years. Comparison of the short-term functional results after surface replacement and total shoulder arthroplasty for osteoarthritis of the shoulder: a matched-pair analysis. Resurfacing arthroplasty of the humerus: indications, surgical technique, and clinical results. Quality-of-life outcome following hemiarthroplasty or total shoulder arthroplasty in patients with osteoarthritis. Increasing number and incidence of osteoporotic fractures of the proximal humerus in elderly people. Changes in the incidence of fracture of the upper end of the humerus during a thrirty-year period. Risk factors for proximal humerus, forearm, and wrist fractures in elderly men and women: the Dubbo Osteoporosis Epidemiology Study. Radial and humeral fractures as predictors of subsequent hip, radial or humeral fractures in women, and their seasonal variation. Comparison of the use of the humerus intramedullary nail and dynamic compression plate for the management of diaphyseal fractures of the humerus. Randomized prospective study of humeral shaft fracture fixation: intramedullary nails versus plates. Fixation of fractures of the shaft of the humerus by dynamic compression plate or intramedullary nail. Routine aspirin or nonsteroidal anti-inflammatory drugs for the primary prevention of colorectal cancer: U.
Buy discount decadron 4 mg on-line. Olivia Culpo's Nighttime Skincare Routine | Go To Bed With Me | Harper's BAZAAR.