Ashley H. Vincent, PharmD, BCACP, BCPS
- Clinical Associate Professor, Department of Pharmacy Practice, College of Pharmacy, Purdue University, West Lafayette
- Clinical Pharmacy SpecialistAmbulatory Care, IU Health Physicians Adult Ambulatory Care Center, Indianapolis, Indiana
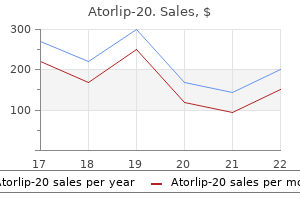
Lying between the two cholesterol levels of heart attack victims purchase atorlip-20 without a prescription, a dense network of muscle fibers perforated in all directions by blood 61 vessels cholesterol test eating cheap atorlip-20 20mg mastercard. The main portion of the uterine wall is formed by this middle layer which consists of an interlacing network of muscle fibers between which extend the blood vessels cholesterol video purchase atorlip-20 20 mg on line. As the result of such an arrangement cholesterol medication chart cheap atorlip-20 20mg without a prescription, when the cells contract after delivery definition of cholesterol ester atorlip-20 20mg fast delivery, they constrict the vessels and thus act as "living ligatures how is cholesterol ratio determined buy atorlip-20 pills in toronto. It has been demonstrated that the uterus has pacemakers to produce the rhythmic coordinated contractions of labor. These pacemaker sites are found near the uterotubal junctions, although the pacemaker cells do not differ anatomically from the surrounding myocytes as they do in cardiac muscle. The interval between contractions diminishes gradually from approximately ten minutes in early labor to as little as two minutes near the end of labor. In the normal process there is a progressive increment in the strength of contractions from approximately 20 mm of mercury at the onset of labor to 50 to 80 mm late in labor. The effect of uterine contractions of this frequency and intensity is twofold on the uterine cervix. First effacement consisting of thinning of the cervix with a shortening of the endocervical canal, is produced. Secondly, cervical dilatation concurs, initially slowly as it accompanies the process of effacement of the cervix, and then more rapidly as cervical effacement has been accomplished (see Figure 1). Progressive contractile activity of the uterus has been demonstrated throughout pregnancy. False labor, Braxton-Hicks contractions, and pre-labor contractions are terms that have been applied to this uterine activity. The latter term is probably the most appropriate, and it is this uterine activity, which accomplishes a significant degree of effacement and even some dilatation in the days or weeks prior to the onset of recognizable labor. Descent of the presenting part of the fetus into the birth canal, particularly in a first pregnancy, is another result of pre-labor. The Mechanism of Normal Labor the definition or clinical diagnosis of labor is a retrospective one. There is no laboratory test that gives a "labor titer" or an x-ray procedure that can define the difference between the laboring and non-laboring patient. Realizing these limitations, the patient is diagnosed as being in labor when a combination of conditions exists. Perhaps a good working definition may be stated as follows: When in the presence of perceived uterine contractions, there is progressive cervical dilatation and descent of the presenting part which leads to the eventual expulsion of the products of conception, the patient is in labor. The "mechanism of labor" refers to the sequencing of events related to posturing and positioning that allows the baby to find the "easiest way out. For a normal mechanism of labor to occur, both the fetal and maternal factors must be harmonious. An understanding of these factors is essential for the obstetrician to appropriately intervene if the mechanism deviates from the normal. The definitions at the beginning of this section should mastered to be able to discuss and understand the mechanism of labor. The single most important determinant to the mechanism of labor is probably pelvic configuration. The classic work of Caldwell and Maloy is reviewed in the text and should be understood. Their classification of the pelvis into four major types (gynecoid, android, anthropoid, and platypelloid) helps the student understand the possible difficulties that may arise in a laboring patient. A quote that should be remembered is: "No two pelves are exactly the same, just as no two faces are the same. For each pelvis 62 there is an optimum mechanism that may be wholly different from the so-called normal mechanism described. Regardless of the shape, the baby will be delivered if size and positioning remain compatible. The narrowest part of the fetus attempts to align itself with the narrowest pelvic dimensions. It must be understood, however, that these are arbitrary distinctions in a natural continuum. This occurs as a result of impingement of the presenting part on the bony and soft tissues of the pelvis. This is anterior and then posterior shoulders, followed by trunk and lower extremities in rapid succession. Abnormal mechanisms of labor do occur, and the operator must be able to recognize these early and intervene when appropriate. Those patients who have undeliverable or uncorrectable problems should be unhesitatingly delivered by the abdominal route because inappropriate operative vaginal intervention may lead to damage to both mother and fetus. Some of the undeliverable situations include persistent mentum posterior, persistent brow presentation, some types of breech presentations, and shoulder presentation. Except for cervical dilatation and fetal descent, none of the clinical features of the parturient patient appears to be useful in assessing labor progression. The graphic representation of labor plotting descent and dilatation against time has become known as the Friedman curve. Graphic portrayal of the relationship between cervical dilatation and elapsed time in labor (heavy line) and between fetal station and time (light line). Labor has been divided functionally into a preparatory division (including latent and acceleration phases of the dilatation curve), a dilatational division comprising only the linear phase of maximum slope of dilatation, and a pelvic division encompassing the linear phase of maximum descent. Functional classification of labor Principal Clinical Features on the Functional Divisions of Labor Characteristic Preparatory Dilatational Pelvic Division Division Division Functions Contractions Cervix actively dilated Pelvis negotiated; coordinated, polarized, mechanisms of labor; oriented, cervix fetal descent delivery prepared Interval Latent and acceleration Phase of maximum Deceleration phase and phases slope second stage Measurement Elapsed duration Linear rate of dilatation Linear rate of descent Diagnosable Prolonged latent phase Protracted dilatation; Prolonged deceler-ation; disorders protracted descent secondary arrest of dilatation; arrest of descent; failure of descent C. Abnormal labor Dystocia (literally difficult labor) is characterized by abnormally slow progress in labor. It is the consequence of four distinct abnormalities that may exist singly or in combination. Uterine forces that are not sufficiently strong or appropriately coordinated to efface and dilate the cervix. Forces generated by voluntary muscles during the second stage of labor that are inadequate to overcome the normal resistance of the bony birth canal and maternal soft parts. Faulty presentation or abnormal development of the fetus of such character that the fetus cannot be extruded through the birth canal. Abnormalities of the birth canal that form an obstacle to the descent of the fetus. Labor Disorders Pattern Diagnositc Criterion Nulliparas 20 hr or more Prolonged latent phase Multiparas 14 hr or more Nulliparas 1. Prolonged latent phase of labor Arrest disorder A Secondary anrst of dilatation pattern with documented cessation of progression in the active phase 67 B Prolonged deceleration phase pattern with deceleration phase duration greater than normal limits C Failure of descent in the deceleration phase and second stage D Arrest of descent characterized by halted advancement of fetal station in the second stage. These four abnormalities are similar in etiology, response to treatment, and prognosis, being readily differentiated from the normal dilatation and descent curves (broken lines). Showing line of axis traction perpendicular to the plane of the pelvis at which the head is stationed. She is observed at be rest, and over the course of the next 24 hours her blood pressure increases to 150 to 160/100 to 110. Define the various hypertensive disorders in pregnancy and the underlying pathophysiology. Know the incidence, clinical course, prognosis, prophylaxis and general management including pharmacologic agents used for these disorders. Late Pregnancy Bleeding Case Presentation A 32-year-old, gravida 6, para 5-0-0-5 at 28 weeks of gestation presents with vaginal bleeding to the emergency room. Her vital signs show a blood pressure of 100/50, a pulse of 98, and respiratory rate of 24. The most common obstetrical and non-obstetrical causes and overall incidence of bleeding late pregnancy. If the unsuspected diagnosis is abruptio placentae, know the pathophysiology, clinical characteristics, maternal and fetal complications and management. If the suspected diagnosis is placenta previa, know the classification, incidence and probable mechanism, methods to localize the placenta clinical characteristics and management Preeclampsia and Eclampsia I. Eclampsia is the occurrence of convulsions, not caused by any coincident neurologic disease in a woman whose condition fulfills the criteria for 70 preeclampsia. Preeclampsia, can occur any time after 20 weeks of gestation but usually becomes clinically evident late in pregnancy. Incidence-Occurs in 6 to 8% of pregnancies and continues to be one of the leading causes of Maternal morbidity and mortality. Magnesium sulfate-typically administered intravenously, monitoring reflexes, respirations and urine output. Delivery is achieved by induction of labor and use of ceasarean section for fetal or obstetrical indications. The goal of management of this disease is to keep the mother healthy and prevent intrauterine fetal demise. The earlier the onset of the illness, the more severe the course with regard to mother and fetus. Definition-Place: Implantation in the lower uterine segment over or near the cervical internal os. This can result in not only a cesarean section but also a postpartum hysterectomy commonly referred to as a cesarean hysterectomy. Low-lying Placenta-placental implantation in the lower uterine segment, but the placental edge does not actually reach the internal os. Painless hemorrhageusually occurring toward the end of the second trimester or later 2. Large placenta such as in multiple gestation and pregnancies complicated by fetal erythroblastosis. Diagnosis: the diagnosis is suspected in the setting of painless bleeding late in pregnancy, a uterus which is soft and nontender, and a presenting part which is high in the uterus. It is dangerous to do a vaginal examination on a patient with third trimester bleeding since this may precipitate uncontrollable hemorrhage. Management In the setting of a premature fetus and no active bleeding, hospitalization and close observation is standard. Delivery by cesarean section is indicated in the setting of fetal maturity or severe maternal hemorrhage. Definition the separation of the placenta from its site of implantation in the uterus before the delivery of the baby. Placental abruption can be complicated by severe maternal hemorrhage, coagulation defects, renal failure, and fetal demise. Management Treatment will vary depending on the well-being of the mother and baby. Close monitoring of fluid balance and coagulation defects is essential to optimize outcome. In couples who conceive normally, 50% do so following 3 tries whereas about 92% conceive following 12 attempts. Sterility: the etiology of infertility is established and there is no possibility for conception. This does not appear to be caused by an increased proportion of infertility within age groupings. Rather, factors contributing to the demand include: a higher absolute number of couples of reproductive age ("baby boomers"), decreasing availability of babies for adoption (largely due to legalized abortion and increasing social acceptance of single parenthood), less stigma regarding infertility, increasing tubal disease due to sexually transmitted disease, and better and more plentiful medical care providers for infertility services. However, the most important contributor to the increased prevalence of infertility visits is delayed childbearing with consequent attrition of ovarian ftinction. A systematic approach should be used to evaluate the cause(s) of infertility for a couple, while the emotional stress that accompanies infertility for both partners must be constantly addressed. The etiology of infertility can be divided into three major categories: (1) female factor, (2) male factor, and (3) undetermined etiology. Approximately 40% of infertility cases, where the etiology has been determined, are due to female factor, 40 % to male factor, and the remaining 20% are due to mixed male/female factors. In 10-20% of couples presenting for evaluation, no diagnosis can be made after standard investigation (unexplained infertility). A sexual history should be obtained, including the frequency and timing of intercourse, the use of potentially spermicidal lubricants and a complete menstrual history. Systematic consideration of major risk factors for each component should be considered during historytaking. Ovariestumors, surgical trauma, endometriosis, radiation / chemotherapy damage, dysgenetic gonads, polycystic ovary syndrome Gametes/ folliculogenesisage, smoking, medications. Also, the basic tests used to evaluate each component of the reproductive system will be reviewed. Pelvic exam offers many clues including assessment of ovarian estrogen production (via observation of cervical mucus production and vaginal cytology). Mullerian abnormalities, leiomyomata uteri, and other pelvic masses and observation of any pelvic pain.
Notice As a parent of a child with a disability or suspected disability low cholesterol foods.com buy atorlip-20 20mg overnight delivery, you will receive notices to tell you about proposed special education services cholesterol levels ati 20 mg atorlip-20, meetings and your rights cholesterol under eyes 20 mg atorlip-20 overnight delivery. There are three kinds of notices that you will receive at various times throughout the special education process cholesterol formula discount atorlip-20 20mg line. It must be provided to you in the language you speak or other kind of communication that you understand unless it is clearly not possible to do so cholesterol test to buy buy discount atorlip-20 20mg on line. It must be provided to you in the language you speak or other kind of communication that you understand cholesterol over 300 cheap 20 mg atorlip-20 fast delivery, unless it is clearly not possible to do so. You must receive a written meeting notice at least five days before the meeting unless you and the school district agree to meet within five days or in certain meetings relating to discipline procedures. If the proposed meeting time or place is not good for you, you may call the school district to ask for a change that is good for both of you. They may call you before a meeting occurs to talk about evaluation results and ask you for information, or they may ask you to participate in the meeting by telephone. If necessary, the district must take steps to make sure that the notice is translated orally or by other means so that you understand the notice. State complaint procedures, including information about how to file a complaint and timelines (page 30). However, if you place your child in a private school because you and the school district disagree that an appropriate program has been made available for your child, you have the right to request an impartial hearing to seek reimbursement for the private school placement. However, the cost of reimbursement may not be reduced or denied because you did not give this notice if you are unable to read and cannot write in English; or if providing notice would likely result in physical or serious emotional harm to your child; or if the school prevented you from providing the notice; or if you did not receive the procedural safeguards notice that tells you about this requirement, then the cost of reimbursement may not be reduced or denied because you did not give this notice. If you refuse to make your child available, any request for tuition reimbursement may be reduced or denied. If you do not inform the school district or make your child available for the evaluation, or if there are other unreasonable actions on your part, an impartial hearing officer or court may reduce or deny the reimbursement of costs of the private school for your child. Review If your child is a child with a disability whose special education programs and services are being reviewed, the Board of Education must arrange for appropriate special education programs and services within 60 school days of the referral for review. If the recommendation is for placement in an approved in-State or out-of-State private school, then the Board of Education will arrange for such programs and services within 30 school days of the Board receipt of the recommendation from the Committee. If you disagree with evaluation results or other proposed actions of the Committee, such as the recommendation, placement or implementation of the program, you should express your disagreement and dissatisfaction. Try to work out differences informally with your school district as soon as they happen. W rite down what was discussed at the meeting, staff present and steps identified to resolve your concerns. If necessary, request a follow-up meeting within a reasonable amount of time to revisit your concerns and to ensure that the steps identified above were implemented as planned. If you decide to use mediation, you must ask for it by writing to the Board of Education (see form on page 35). Any agreement reached by the parties is set forth in a written mediation agreement. W ritten agreements may be presented as part of the record at an impartial hearing. Parties to the mediation process may be required to sign a confidentiality pledge before starting the mediation. Of the 375 special education mediation sessions that took place in New York State during 2000-2001, 91% resulted in agreement. The following comments were made by school district representatives and parents after participating in mediation. I also felt that how the mediation was explained and handled made me, as parent, feel more comfortable. The district was far more sensitive to our concerns once the mediation was involved. Your request for an impartial hearing must be made in writing to the Board of Education. However, the school district may not deny or delay your right to an impartial hearing if you do not provide that information. For threeand four-year-old children, the school district may not begin a hearing if you refuse to give consent to initial evaluation or the initial provision of special education to your child. If requested by you, the school district must provide you with information on free or low-cost legal and other relevant services. If a hearing officer requests an independent educational evaluation as part of the hearing, the cost of the evaluation must be at public expense. The decision of the hearing officer will be based only on recorded information presented at the hearing and will provide the reasons and facts for the decision. The decision will be binding (final) unless you or the school district appeal to the State Review Officer. If an extension has been granted, the findings of fact and decision must be issued no later than 14 days from the date the record is closed including any post hearing submissions and the transcript is received. Impartial hearing officer An impartial hearing officer must be an individual certified by the Commissioner of Education to conduct impartial hearings. The impartial hearing officer makes sure that procedures at the hearing meet due process requirements. An individual employed by such schools or programs may not serve as an impartial hearing officer for two years following the end of his or her employment. A guardian ad litem is appointed from the list of surrogate parents or is a pro bono attorney (an attorney who takes cases at no cost). In the event a guardian ad litem is assigned, the impartial hearing officer must make sure that your due process rights are protected throughout the hearing. Surrogate parents Each school district must try every reasonable way to notify the parents of the child who has been referred or is in need of special education and related services. The person is not an employee of the agency just because he or she is paid by the agency to serve as a surrogate parent. State-Level Appeal of Impartial Hearing Officer Decisions the decision made by the impartial hearing officer is final (must be followed by you and the school district) unless you or the school district ask for a review of the decision of the impartial hearing officer (called an appeal) by the State Review Officer. Procedures and timelines for submitting an appeal are specific and must be followed exactly to avoid delay or dismissal. If a hearing is held, all the parent rights listed under impartial hearings continue. A review involving spoken testimony and/or written evidence (at the discretion of the State Review Officer) must be held at a time and place that is reasonably convenient to the involved parties. The State Review Officer may extend the time beyond the 30 days at the request of you or the school district. During any hearing or appeal, your child will remain in his or her current educational placement. Preschool child Your preschool child will stay in his or her current placement during any hearing or appeal, unless you and the school district agree in writing to other arrangements. School-age child During any hearing or appeal, your school-age child will stay in the school placement he or she is in now, unless you and the school district agree in writing to other arrangements. If the due process proceeding concerns consent for an initial evaluation, your child will not be evaluated while the proceeding is pending. Opportunity to present complaints You have the right to submit a written complaint to the New York State Education Department if you believe that your school district has violated procedures under State or Federal special education laws and regulations. Your complaint must include a statement that the school district has violated special education laws or regulations and include the facts on which you base your statement. This only applies to alleged violations that occurred not more than three years prior to the date of the written complaint. You must send the original signed written complaint to: Coordinator, Statewide Special Education Quality Assurance Office of Vocational and Educational Services for Individuals with Disabilities One Commerce Plaza, Room 1624 Albany, New York, 12234 You will receive a letter stating that your complaint has been received and telling you about your right to submit additional information about the complaint either orally or in writing. You will receive a written, final decision that addresses each claim you raise and contains the findings of fact, and the reasons for the final decision. Any part of the complaint that is currently being addressed in an impartial hearing cannot be investigated.
Purchase atorlip-20 20 mg line. à¤à¥à¤²à¥à¤¸à¥à¤à¥à¤°à¥à¤² मà¥à¤ à¤à¥à¤¯à¤¾ à¤à¤¾à¤à¤ à¤à¥à¤¯à¤¾ ना à¤à¤¾à¤à¤ | Natural home remedies for lowering cholesterol.
The development of multidisciplinary care seems to be associated with an improvement in maternal and fetal outcomes cholesterol levels and heart disease purchase atorlip-20 20mg amex. If there is a relevant multidisciplinary team available within reasonable travelling distance cholesterol lowering drugs buy atorlip-20 mastercard, women should go there hdl cholesterol in shrimp discount 20 mg atorlip-20 visa. Partner status and subsequent counselling should be clearly documented in the notes cholesterol medication beginning with l buy atorlip-20 cheap. If women have not undergone a preconceptual review ldl cholesterol diet chart purchase 20mg atorlip-20 mastercard, they should be advised to take daily folic acid and D prophylactic antibiotics (if not contraindicated) cholesterol test large small generic atorlip-20 20mg with amex. Iron supplementation should be given only if there is laboratory evidence of iron deficiency. Women who are at increased risk of pre-eclampsia are advised to take low-dose aspirin 75 mg from 12 weeks of gestation, unless they have aspirin sensitivity. Blood pressure and urinalysis should be performed at each consultation, and midstream urine for C culture performed monthly. Women with pre-existing proteinuria or known renal impairment will require more frequent monitoring. Studies have also demonstrated an increase in the incidence of urinary tract infection and asymptomatic bacteriuria,26 so urinalysis should be performed at each antenatal visit and midstream urine should be sent for culture and sensitivity monthly. At each appointment, opportunities should be offered for information and education. In addition, women should be offered serial fetal biometry scans (growth scans) every 4 weeks from 24 weeks of gestation. Serial growth scans allow early detection of fetal growth restriction and hence aid level 2+ appropriate timing of delivery to reduce perinatal mortality and morbidity. A If acute exchange transfusion is required for the treatment of a sickle complication, it may be D appropriate to continue the transfusion regimen for the remainder of the pregnancy. Blood should be matched for an extended phenotype including full rhesus typing (C, D and E) as well A as Kell typing. P Early studies recommended prophylactic transfusion during pregnancy as there was a decrease in Evidence maternal morbidity and perinatal mortality among transfused women compared with historical level 1controls. A randomised controlled trial59 and a retrospective study25 have Evidence demonstrated that prophylactic transfusion decreased the incidence of maternal painful crises but level 1did not influence fetal or maternal outcome. A systematic review60 indicated that there is insufficient evidence to draw conclusions about the role of transfusion in pregnancy. There is no absolute level at which transfusion should be level 4 undertaken and the decision must be made in conjunction with clinical findings, but haemoglobin under 6 g/dl or a fall of over 2 g/dl from baseline is often used as a guide to transfusion requirement. Alloimmunisation is clinically important as it can lead to delayed haemolytic transfusion reactions or haemolytic disease of the newborn62 and can render patients Evidence untransfusable. D Pregnant women presenting with acute painful crisis should be rapidly assessed by the D multidisciplinary team and appropriate analgesia should be administered. Women admitted with sickle cell crisis should be looked after by the multidisciplinary team, involving D obstetricians, midwives, haematologists and anaesthetists. The requirement for fluids and oxygen should be assessed, and fluids and oxygen administered if D required. Thromboprophylaxis should be given to women admitted to hospital with acute painful crisis. Primary care physicians should have a low threshold for referring women to secondary care; all women with pain which does not settle with simple analgesia, who are febrile, have atypical pain or chest pain or symptoms of shortness of breath should be referred to hospital. History should ascertain if this is typical sickle pain or not, and if there are precipitating factors. Examination should focus on the site of pain, any atypical features of the pain and any precipitating factors, in particular whether there are any signs of infection. Initial investigations should include full blood count, reticulocyte count and renal function. Other investigations will depend on the clinical scenario but may include blood cultures, chest X-ray, urine culture and liver function tests. Initial analgesia should be given within 30 minutes of arriving at hospital and effective analgesia Evidence should be achieved within 1 hour. Weak opioids such as co-dydramol, co-codamol or dihydrocodeine can be used for moderate pain, and stronger opiates such as morphine can be used for severe pain. Parenteral opiates can be given by intermittent bolus or patient-controlled administration systems. If the women need strong opiate therapy, they will need to be admitted to hospital: to a medical ward in early pregnancy, or to a level 2 antenatal bed in later pregnancy, under the joint care of obstetricians and haematologists. Assessments of pain score, sedation score and oxygen saturation should be performed at least 2-hourly using a modified obstetric early warning chart. Outline of management of acute pain Rapid clinical assessment If pain is severe and oral analgesia is not effective, give strong opioids. There is a risk of fluid overload in women with preeclampsia; senior experienced staff should be involved in managing the fluid balance of these women. Therapeutic antibiotics should be prescribed if the woman is febrile or there is a high clinical suspicion of infection. Other adjuvants may be required to treat the adverse effects of opiates, such as antihistamines to treat itching or laxatives to prevent opiate-induced constipation, and antiemetics may be required. Opiates are not associated with teratogenicity or congenital malformation but may be associated with transient suppression of fetal movement and a reduced baseline variability of the fetal heart rate. Where a mother has received prolonged administration of opiates in late pregnancy, the neonate should be observed for signs of opioid withdrawal. Acute severe infection with the H1N1 virus in pregnancy can cause a similar clinical picture, and investigation and treatment for this should be instituted. Treatment is with intravenous antibiotics, oxygen and blood transfusion, as in non-pregnant women. If the woman has hypoxia, she should be reviewed by the critical care team and ventilatory support may be required. In women presenting with acute hypoxia, there should be a low threshold for considering pulmonary embolism. In this situation, therapeutic low-molecular-weight heparin should be commenced until the woman has been reviewed by senior staff and definitive investigations have been undertaken. Acute stroke is a medical emergency and a rapid-exchange blood transfusion can decrease long-term neurological damage. If a stroke is suspected, the woman should have urgent brain imaging and the haematologist should be called for consideration of urgent exchange transfusion. Therefore, a reticulocyte count should be requested in any woman presenting with an acute anaemia and, if low, may indicate infection with erythrovirus. With erythrovirus infection there is the added risk of vertical transmission to the fetus, which can result in hydrops fetalis, hence a review by a fetal medicine specialist is indicated. In women who have hip replacements (because of avascular necrosis) it is important to discuss suitable P positions for delivery. There are no randomised controlled trials to dictate the appropriate timing of delivery. However, other studies demonstrating improved clinical outcomes21,22,24,26 all support vaginal Evidence delivery as the recommended mode of delivery with the need for caesarean section based on level 2+ obstetric indications. D Continuous intrapartum electronic fetal heart rate monitoring is recommended owing to the increased D risk of fetal distress which may necessitate operative delivery. There is an increased risk of painful crisis with protracted labour (more than 12 hours), but this is often Evidence secondary to dehydration. In this situation, if the woman is well hydrated and labour is progressing, level 2+ the labour should be carefully supervised; caesarean section should be considered if labour is not progressing well and delivery is not imminent. Venous access can be difficult, especially if they have had multiple previous admissions, and as such anaesthetic Evidence review/intravenous access should be obtained early. The demand for oxygen is increased during the level 4 intrapartum period and the use of pulse oximetry to detect hypoxia in the mother is appropriate during labour. Arterial blood gas analysis should be performed and oxygen therapy instituted if oxygen saturation is 94% or less. Routine antibiotic prophylaxis in labour is currently not supported by evidence, but hourly observations of vital signs should be performed. Continuous level 2+ electronic fetal heart rate monitoring is recommended because of the increased rate of stillbirth, placental abruption and compromised placental reserve. General anaesthesia carries additional risks beyond the normal obstetric case and should be avoided where possible. Regional anaesthesia during labour may reduce the necessity of general anaesthesia for delivery. It is also likely to reduce the need for high doses of opioids if the woman has sickle-related pain in the lower body. Maintain maternal oxygen saturation above 94% and adequate hydration based on fluid balance until D discharge. Low-molecular-weight heparin should be administered while in hospital and 7 days post-discharge D following vaginal delivery or for a period of 6 weeks following caesarean section. Thromboprophylaxis in the form of low-molecular-weight heparin is recommended while the Evidence pregnant woman is in hospital and for 7 days following vaginal delivery or for a period of 6 weeks level 4 following caesarean section. This section should be read in conjunction with the Faculty of Sexual & Reproductive Healthcare guidance on postnatal hormonal contraception. Suggested audit topics fi the proportion of staff who receive appropriate training. Telfer P, Coen P, Chakravorty S, Wilkey O, Evans J, Newell H, et molecular disease. Pregnancy in sickle cell disease: experience of the Research Council Vitamin Study. Effect of hydroxyurea on the frequency of painful and mortality in sickle cell pregnancies in Lago, Nigeria: a case crisis in sickle cell anemia. Hydroxyurea in two pregnant Outcome of pregnancy in homozygous sickle cell disease. Effect of active prenatal management on Bahrain with special reference to sickle cell disease. Pulmonary hypertension in patients with sickle cell agents for preventing pre-eclampsia and its complications. Prophylactic Thalassaemia Screening Programme; 2009 [ transfusions of normal red blood cells during pregnancies sct. Prophylactic transfusions in pregnant patients with sickle of the British Committee for Standards in Haematology Clinical hemoglobinopathies: benefit versus risk. Prophylactic versus selective blood transfusion surveillance tests during sickle cell crisis. Transfusion Placental histology and placental/fetal weight ratios in prevents acute chest syndrome predicted by elevated pregnant women with sickle cell disease: relationship to secretory phospholipase A2. Wright J; British Committee for Standards in Haematology 75 Faculty of Sexual & Reproductive Healthcare. Cerebrovascular accidents in sickle cell Effect of Depo-Provera or Microgynon on the painful crises disease: rates and risk factors. They must be evaluated with reference to individual patient needs, resources and limitations unique to the institution and variations in local populations. Attention is drawn to areas of clinical uncertainty where further research might be indicated. The guidelines review process will commence in 2014 unless evidence requires earlier review. The ultimate judgement regarding a particular clinical procedure or treatment plan must be made by the doctor or other attendant in the light of clinical data presented by the patient and the diagnostic and treatment options available within the appropriate health services. Meiotic errors are correlated with the number and location of recombination events Fig. Team Members (3) Reduce preterm birth, intrauterine growth restriction, congenital anomalies, and Joanne M.
Becoming pregnant from a sexual assault is a significant concern of sexual assault patients cholesterol lowering super foods discount atorlip-20 20 mg otc, and patients of different ages cholesterol ratio of 2.4 discount atorlip-20 master card, social cholesterol whole milk purchase atorlip-20 visa, cultural cholesterol norms order generic atorlip-20 from india, and religious/spiritual backgrounds may have varying feelings regarding acceptable treatment options cholesterol test hdl ldl buy atorlip-20 20mg visa. Most programs offer pregnancy prevention or interception for sexual assault patients if they are seen within 120 hours of the assault cholesterol equation order cheapest atorlip-20 and atorlip-20. The risk of pregnancy from sexual assault is estimated to be 2 to 5 percent, similar to the risk of pregnancy from a one-time sexual 287 encounter. The 2005 National Crime Victimization Study reported 64,080 female victims of rape; therefore, statistically speaking, up to 3,204 pregnancies could have resulted from the rapes. Any female of reproductive capability (Tanner Stage 3 and above, irrespective of menarche) can potentially become pregnant from any single exposure. Determination of the probability of conception also depends upon other variables, for example, the use of contraceptives, regularity of the menstrual cycle, fertility of the victim and the perpetrator, time in the cycle of exposure, and whether the perpetrator ejaculated intravaginally. Although many transgender male individuals believe they are infertile as a result of using testosterone, cases have been reported of unexpected pregnancies. Therefore, if a transgender male individual has not had a hysterectomy, is still within childbearing years, and the nature of the assault suggests it, the possibility of pregnancy should be discussed, even if he has not been menstruating. If a patient is pregnant, the pregnancy may affect what medications can be administered or prescribed in the course of or after the exam. Most commercially available urine pregnancy tests are sensitive to about 50 milli-international units/ml and will detect pregnancy 8 to 9 days after conception, before a menstrual period is missed. If the pregnancy test is positive, emergency contraception is contraindicated and decisions about other medications. If the test is negative and the patient has had unprotected intercourse within the last 10 days and would continue that pregnancy if conception has occurred, then she may be considered to be pregnant and emergency contraception would not be administered. Discuss treatment options with patients in their preferred language, including emergency 290 contraception. Therefore, discuss treatment options with patients, including emergency contraception. If the case is prosecuted, the prosecutor should work to address concerns such as this one. Another option is to forgo immediate treatment and have the patient follow-up with their primary care provider. Discuss options with the patient and information regarding the timeframe for emergency contraception provision, so she can make an informed decision. Inform the patient that the provision of any emergency contraception will not prevent sexually transmitted infections. The conversation with the patient should include a thorough discussion, including mechanism of action for each treatment option, side effects, dosing, and follow-up. This information should also be provided in writing in the preferred language of the patient, if possible. A victim of sexual assault should be offered prophylaxis for pregnancy, subject to informed consent and consistent with current treatment guidelines. Offer/provide the patient with emergency contraception pills and anti-nausea medication if they are at risk, 292 according to facility policy. Emergency contraception is a hormonal method of preventing pregnancy that can be used after sexual assault. It is recommended, however, 293 294 295 that levonorgestrel, a synthetic hormone, be used. This option is recommended for its higher efficacy 296 rate and ease of dosing, and the fewest number of side effects, particularly nausea and vomiting. Levonorgestrel will not end a pregnancy that is already in progress and is considered a safe and easy treatment for victims of assault in preventing a pregnancy. Levonorgestrel is most effective if used within 297 120 hours and can reduce the risk of pregnancy by up to 89 percent. If no bleeding has occurred within three weeks, the patient should be reevaluated and a repeat pregnancy test performed. The patient must be advised not to have unprotected intercourse until after the menses has occurred, or the repeat pregnancy test is negative. If no referral is available, provide the patient with the following phone numbers: 1-888-not2late or the online 300 reference: not-2-late. The only absolute contraindication for the use of Plan B is preexisting pregnancy. Mechanism of Action of Hormonal Preparations Used for Emergency Contraception; a Review of the Literature. Increasing access to emergency contraception through community pharmacies: lessons from Washington state. Health care personnel have important tasks to accomplish prior to discharging patients, as do advocates and law enforcement representatives (if involved). These responders should coordinate their activities as much as possible to reduce repetition and avoid further overwhelming patients. Discuss 301 with patients whether they have any other medical and/or mental health concerns related to the assault. If injuries or trauma have not been treated yet, examiners should refer patients to exam facility clinicians. The discharge form could also include contact information and hours of operation for local advocacy programs. Follow-up may be indicated to document developing or healing injuries (for example, bruising) and complete resolution of healing. Forensic follow-up may also be indicated to further evaluate nonspecific findings (such as redness, swelling, or cervical abnormalities) that may be related to acute trauma or may be normal variants. If appointments are not scheduled, at least indicate to patients which appointments are needed and if sites are different than the initial exam. Make it clear that patients do not 302 have to disclose the assault to receive follow-up medical care. The main purposes of such a call are to check on medical status and remind patients about the necessity of follow-up testing and care. An optimal time for a first medical follow-up contact is 24 to 48 hours following discharge. Personnel following up with patients should be familiar with the 303 case, confidentiality issues, and potential medical needs. They also may encourage patients to discuss with health care providers their concerns about initial and follow-up medical care. Involved responders should come to agreement about who is responsible for each step below and where coordination is necessary. For example, while advocates usually explain advocacy services and law enforcement representatives explain the investigative process, each responder may have a role in helping patients plan for their safety and well-being. If health care personnel are the only responders involved, however, they may need to provide patients with much of the information below. Jurisdictional and exam site policies should be in place to facilitate this process. Assist patients in developing a postexam plan that addresses their physical safety and emotional well-being. For example, if patients with physical disabilities require shelter, the shelter must be accessible and staff able to meet their needs for 304 personal assistance with activities of daily living. If patients living in institutional settings have been assaulted by another resident, a staff person, or person who has easy access to residents, the institution should offer alternative living arrangements and reduce the likelihood that patients have to come into contact with the assailant again. Coordinate follow-up contact of involved agencies as much as possible, keeping the number of responders contacting patients to a minimum. Explain if contact procedures are different for patients with limited English proficiency or specific communities or institutions. Consider offering patients prepaid phone cards they can use to call a contact person with concerns or questions. Sexual assault advocacy programs typically offer a host of services for victims and their significant others, in addition to those provided during the exam process. Some advocacy programs provide professional mental health counseling, but many refer patients to community or private agencies. Before being discharged, advocates should ask patients if they can follow up with them. During follow-up contacts, advocates can help patients reassess their safety; offer support and crisis counseling; answer their questions and provide additional referrals and information; and help coordinate other advocacy services and counseling based upon identified needs. Explain if contact procedures are different for patients with limited English proficiency or for specific communities or institutions. Patients should receive contact information of involved law enforcement representatives and agencies and a case report number. They should be aware that they will be contacted by the prosecution office if their case goes forward. Ask patients if they want to be contacted by law enforcement in these situations and, if so, determine the best contact method. For patients who have not made a report and when law enforcement is not involved, patients should be given information on who to contact and how if they decide that they do want to make a report. They should also be given information on where the kit will be stored and how it will be tracked (for example if there is a tracking number, it should be provided). It can be helpful for them to know the range of time it typically takes in that jurisdiction for evidence to be analyzed and for cases to be forwarded to prosecution or tried in court. At the same time, they must understand that every case is different and typical time estimates from the past may not apply. It should be expected that examiners will be called on to testify in court as either fact and/or expert 307 witnesses, even though in some cases, a plea bargain may be agreed upon, or the prosecuting attorney may decide not to try the case. Examiners should always conduct and document each examination knowing that legal testimony may ultimately be required. This information should assist examiners in explaining to patients during the exam their potential role as a witness should the case be prosecuted. In almost every case that is litigated, cross-examination after initial testimony will occur. Cross-examination is a part of our constitutional framework, but as defense counsel represent alleged offenders, their questions may be perceived by examiners as intimidating and hostile. It is critical that examiners are prepared to effectively handle such situations and have a support system in place to help them prepare for and deal with related stress they may experience. Involve trainers from health care, prosecution, and the judiciary in trainings on court testimony. Also, include defense attorneys who can educate examiners on defense perspectives. In addition to attending trainings, examiners should stay abreast of cutting-edge practices and related case law. Expert witnesses may give opinions in court on matters in which their expertise is relevant. Nonexpert witnesses normally cannot give opinions in response to questions in court, but can only testify to the facts (what has been observed, collected, or heard). Beyond preparing examiners, it is critical to encourage training for attorneys who try these cases on how to properly interpret and use the medical forensic examination. In addition, they need an accurate understanding about the education and clinical preparation, roles, and responsibilities of the forensic examiner. Like examiners, they can benefit from participating in mock trials and need ongoing education to stay abreast of the latest best practices and related case law. Prosecutors should be aware of and share related case law and protocol guides with judges as references to qualify examiners as expert witnesses. They can also share questions they plan to ask to establish credentials of these witnesses. Additionally, prosecutors must understand how to educate the jury about evidence that will be presented. Similarly, it is important to encourage judicial education on issues related to examiner testimony. Judges may not understand all that occurs during the exam process or the full extent of examiner expertise. Understanding Sexual Violence: Prosecuting Adult Rape and Sexual Assault Cases, Video Library I: Presenting Medical Evidence in an Adult Rape Trial, 2002, is a useful resource for prosecutors and judges (for more information, see. Examiners should be informed well in advance of a trial if they are being called as witnesses. It may be helpful for attorneys calling them (both prosecutors and defense attorneys) to first develop relationships with coordinators of examiner programs, if they exist, or staff that oversee examiners at the exam site. In some facilities, they may need to reach out to risk management departments, which oversee all potential areas of liability for the facility. Attorneys should regard examiners they call as witnesses with respect for the knowledge and expertise examiners offer to the court.